Definition
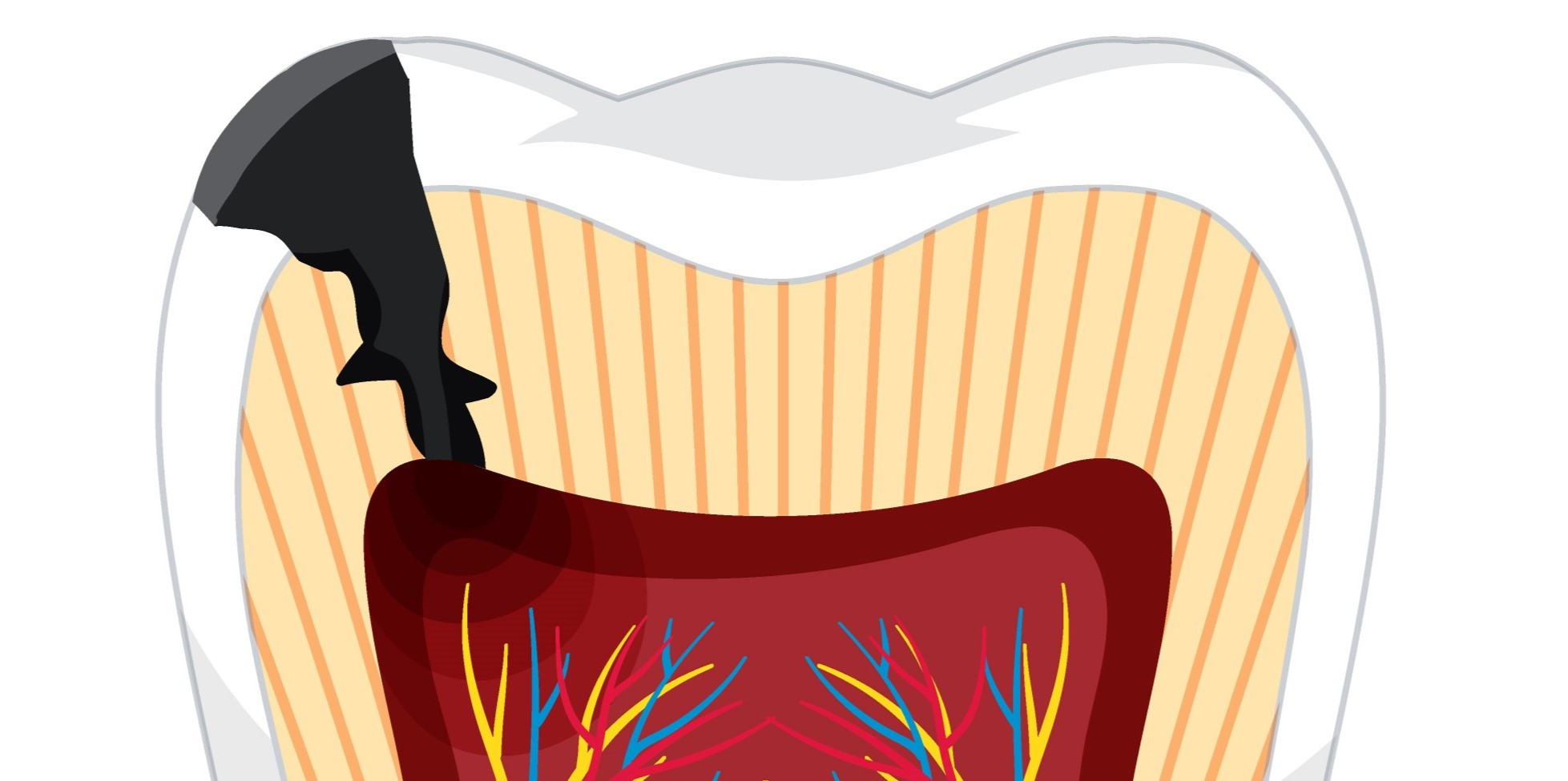
Pulpitis is a painful inflammation of the pulp, which is the innermost soft tissue of the tooth. The pulp contains nerves, blood vessels, and connective tissue, and it plays a crucial role in maintaining tooth health by supplying blood and nutrients to the hard outer tooth layers.
Pulpitis is inflammation of the pulp of the tooth caused by bacterial infection. It can occur in one or more teeth and result in swelling of the infected area. Dentists classify pulpitis into two types based on the severity of the infection.
- Reversible pulpitis
At this early stage, the inflammation is minimal, and the pulp can be reversed with a dental intervention, including indentation and subsequent filling.
- Irreversible pulpitis
The inflammation has intensified at this stage, rendering the tooth incapable of healing. The condition is referred to as pulp necrosis.
Pulpitis is a highly prevalent condition. According to the Centers for Disease Control and Prevention (CDC) of the United States, untreated dental caries, which have the potential to induce pulpitis, are present in approximately one-fourth of adults aged 20 to 64 years.
Causes
The hard enamel of your teeth protects the pulp. If the enamel is damaged, this can lead to pulpitis. Tooth decay can result from:
- Dental caries
Bacteria in your mouth produce acids, which can cause damage to the enamel and lead to cavities in your teeth.
- Microfractures
Chewing hard food and tooth injuries can cause small fissures, known as microfractures.
- Dental procedures
Inadequate tooth coverage during a dental procedure might cause filling leakage and pulpitis.
- Damaged enamel
Teeth grinding (bruxism) and vigorous brushing can destroy enamel and inflame the nerves.
Risk factor
People living in areas without fluoridated water or with particular medical conditions, such as diabetes, may be at a higher risk of developing pulpitis.
Although dental hygiene is frequently a determining factor, children and the elderly may be at higher risk.
Furthermore, lifestyle factors can contribute to an elevated chance of pulpitis, including:
- Lack of dental hygiene, such as not brushing after eating and not seeing a dentist frequently,
- Sugary foods and drinks, such as processed carbs,
- Specific jobs with a high risk of getting a mouth injury, such as boxing or hockey,
- Persistent bruxism
Symptoms
Both types of pulpitis have primary symptoms of pain and sensitivity in the teeth. The pain experience will be different depending on the state of inflammation. Reversible pulpitis can cause less severe pain that only appears when you eat. When permanent pulpitis is present, the discomfort might be more intense, and the symptoms can manifest at any time of the day or night.
Reversible pulpitis symptoms include:
- There is no pain when the dentist taps your tooth
- No sensitivity to heat
- Sensitivity to cold or sweet tastes quickly disappears. It is commonly described as a sharp pain.
Symptoms of irreversible pulpitis include the following:
- Severe pain experienced during dental examination;
- Prolonged sensitivity to hot, cold, or sweet flavors;
- Pain that endures for an extended period. This pain may be dull, throbbing, or sharp.
- Halitosis
- Unpleasant flavor sensation in the oral cavity.
If pulp necrosis happens and nerve tissue has been destroyed, it is possible that you will not feel any sensitivity to hot, cold, or sweet temperatures. However, your tooth may still hurt when the dentist taps on it.
Diagnosis
An essential method for a dentist to diagnose pulpitis is evaluating the teeth's sensitivity. Some examples of sensitivity tests include:
- Electric pulp test
This examination will reveal if the pulp is viable or if pulp necrosis has developed due to the infection. Your dentist uses a gadget to send tiny electrical pulses to your teeth. You may experience the stimulation if your pulp is still alive. If pulp tissue is dead, no electrical pulse is felt.
- Thermal test
The dentist will apply a thermally contrasting material to your teeth. In cases of irreversible pulpitis, the sensation will persist for longer. Lack of sensation is an indication of pulp tissue necrosis.
- Knocking test
The dentist will tap your teeth softly. It is a sign of irreversible pulpitis if you experience pain after tapping.
Your dentist will also recommend an X-ray examination to look for abnormalities or problems in the teeth and signs of infection.
Management
To treat reversible pulpitis, your dentist will first treat the cause. The decaying tissue is removed as part of the treatment, and a regular filling is put on top of the tooth. For irreversible pulpitis, more intensive treatment is required to eliminate pulp tissue. The following therapy options include:
- Endodontic treatment
For root canal treatment, you will typically be directed to a dentist specializing in preserving teeth and treating infections in the dental pulp. The dentist will extract the infected pulp and sanitize the tooth's root. Subsequently, the dentist will fill the vacant root canals and securely seal the tooth. You will have a follow-up appointment with the dentist in a few weeks to receive a dental crown, which will be used to cover your tooth.
- Dental extraction
A common choice is to remove teeth. The dentist will discuss potential solutions for tooth replacement, such as dental implants or dental bridges.
Antibiotics may prevent infection but are not the primary treatment for pulpitis.
Complications
An infection or periapical abscess might result from untreated pulpitis. A periapical abscess is a dental root infection that creates a pus pocket. This may cause:
- Severe pain
- Fever
- Neck lymph nodes are swollen
If untreated, the infection can spread to your jawbone (osteomyelitis), head, neck, and chest soft tissues. The transmission of this infection can be fatal if left untreated.
Prevention
Maintaining proper oral hygiene is the most effective method to prevent pulpitis. This includes the following:
- Brush your teeth twice a day.
- Floss your teeth frequently.
- Visit your dentist for regular cleanings and examinations.
- If you grind your teeth at night, wear a guard.
- See your dentist immediately if you have toothaches or sensitive teeth.
When to see a doctor?
Consult a dentist if you experience toothaches or sensitivity to hot, cold, or sweet foods and drinks. Early treatment can reduce the risk of developing more severe dental issues.
Looking for more information about other diseases? Click here!
- dr. Yuliana Inosensia
Pulpitis: types, symptoms, and treatment. Cleveland Clinic. (n.d.). Retrieved March 6, 2023, from https://my.clevelandclinic.org/health/diseases/23536-pulpitis
Whelan, C. (2019, April 17). Pulpitis: treatment, types, symptoms, causes, and more. Healthline. Retrieved March 6, 2023, from https://www.healthline.com/health/pulpitis
WebMD. (n.d.). Pulpitis: causes, symptoms, and treatments. WebMD. Retrieved March 6, 2023, from https://www.webmd.com/oral-health/what-is-pulpitis