Definition
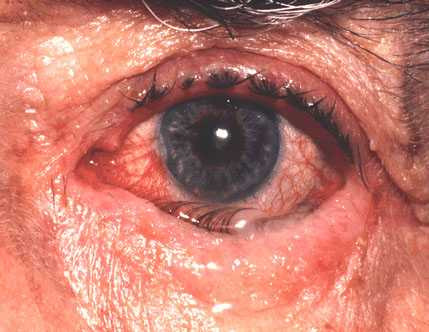
Keratoglobus is an eye disorder where the cornea becomes round and thin, especially at the edges, making it more susceptible to rupture from minor trauma. This rare condition is believed to be genetically inherited, although its specific cause remains unknown.
Causes
The specific cause of keratoglobus remains unknown. However, it is believed to be genetically inherited and associated with several genetic disorders, including:
- Ehlers-Danlos syndrome type VI: An inherited genetic disorder affecting connective tissue, leading to symptoms in the joints and skin.
- Marfan syndrome: A disorder impacting connective tissue, typically affecting blood vessels, eyes, heart, and bones. Individuals with Marfan syndrome are generally taller than average.
- Blue sclera syndrome (Van Der Heave syndrome): A disorder causing a bluish tint in the sclera, affecting connective tissue formation.
- Leber's congenital amaurosis: A retinal disorder characterized by eye-rubbing or pressing movements to alleviate pain.
- Vernal conjunctivitis: Chronic inflammatory eye condition due to an allergic reaction, causing swelling around the eyes.
- Chronic marginal blepharitis: Chronic inflammation of the eyelids.
- Corneal ectasia: Weakening of the cornea caused by repeated eye-rubbing movements
Risk Factor
Currently, there are no identified risk factors for keratoglobus. However, congenital abnormalities running in the family may increase susceptibility to this eye disorder.
Symptoms
Typical signs and symptoms of keratoglobus are visible in the cornea of the eye. There are two distinct types of keratoglobus that an individual might experience, depending on the underlying cause. This condition can either be present from birth, as part of a congenital disorder that runs in families, or it may develop due to other health issues. These include vernal conjunctivitis, a condition of the eye, thyroid-related eye diseases, and long-term inflammation of the eyelids. Physically, various symptoms can be observed, such as:
- Nearsightedness with astigmatism. Difficulty correcting visual acuity with glasses, affecting both eyes.
- Difficulty using contact lenses due to the irregular shape of the cornea.
- Eye pain occurring intermittently or repeatedly, accompanied by impaired vision.
- Irregular retinal reflexes, identified by healthcare professionals.
- Thin corneal layer, detected through further examination, showing thinner edges than the middle.
Diagnosis
Diagnosing keratoglobus involves several examinations that can be conducted by a doctor. Examinations that can be performed on patients, including eye examinations using tools to examine the condition of the eyes more clearly to laboratory tests to explore the cause of the symptoms. Examinations that can be performed by a doctor to see the condition of your eyes are:
- Eye vision and refractive disorder assessment to evaluate visual acuity.
- Slit lamp examination to examine the anterior chamber of the eye.
- Optic nerve, retina, choroid, and blood vessel examination to assess potential complications.
- Other diagnostic tests such as ultrasound or corneal topography to evaluate corneal condition.
Management
The treatment of keratoglobus varies depending on the severity of the corneal condition and the specific complaints of the patient. The following are measures that can be taken to address the symptoms and prevent complications:
- Use of glasses: Glasses can help correct refractive errors and protect the eyes from trauma, aiding in daily activities. However, refractive errors in keratoglobus patients are often challenging to correct completely.
- Diagnostic tests: Genetic examinations or laboratory tests may be conducted to identify congenital abnormalities.
- Contact lenses: Soft or hard contact lenses, under the supervision and advice of a doctor, can assist in correcting refractive errors. Permanent contact lenses may be particularly beneficial.
- Surgery: Surgical intervention to repair the thin corneal layer may be considered, but it is not a first-line treatment, and there is no established gold standard for surgery in keratoglobus management.
Complications
Keratoglobus can lead to severe eye conditions, including:
- Acute corneal hydrops: Sudden corneal cloudiness due to fluid accumulation in the anterior chamber, causing pain and sudden vision loss.
- Corneal perforation: Spontaneous or trauma-induced rupture of the cornea, potentially due to infection, autoimmune conditions, or nerve loss in the cornea.
Prevention
There is no known method to prevent keratoglobus, given its inherited nature. Regular check-ups with an ophthalmologist are recommended for individuals with keratoglobus to monitor and prevent complications.
When to See a Doctor?
The sensations you experience may vary, so it is important to be aware of these signs in order to recognize potential eye emergencies as early as possible. Immediate medical attention is necessary if you experience any of the following symptoms:
- Sudden pain in one or both eyes.
- Sudden blindness or significant vision impairment.
- Eye injury accompanied by vision loss.
- Cloudiness in the cornea with associated vision loss.
Looking for more information about other diseases? Click here!
- dr Hanifa Rahma
Keratoglobus : Symptoms, Causes, Diagnosis, Management and Complications -. Aimu.us. (2021).
Ehlers-Danlos syndromes. nhs.uk. (2021).
Marfan syndrome - Symptoms and causes. Mayo Clinic. (2021).
Leber congenital amaurosis: MedlinePlus Genetics. Medlineplus.gov. (2021).
Vernal conjunctivitis: MedlinePlus Medical Encyclopedia. Medlineplus.gov. (2021).
Putnam, C. (2016). Diagnosis and management of blepharitis: an optometrist’s perspective. Clinical Optometry, Volume 8, 71-78. https://doi.org/10.2147/opto.s84795
Fenzi, C., Bunya, V., & Rose, L. (2021). Keratoglobus - EyeWiki. Eyewiki.aao.org. Retrieved 21 November 2021, from https://eyewiki.aao.org/Keratoglobus.
Keratoconus, C. (2021). Corneal Hydrops: A Complication of Keratoconus. Emra.org.
Weiner, G. (2021). Corneal Perforations. American Academy of Ophthalmology. Retrieved 21 November 2021, from https://www.aao.org/eyenet/article/corneal-perforations.
Kanski, J. J. (2020). Clinical diagnosis in ophthalmology. Elsevier Mosby.