Definition
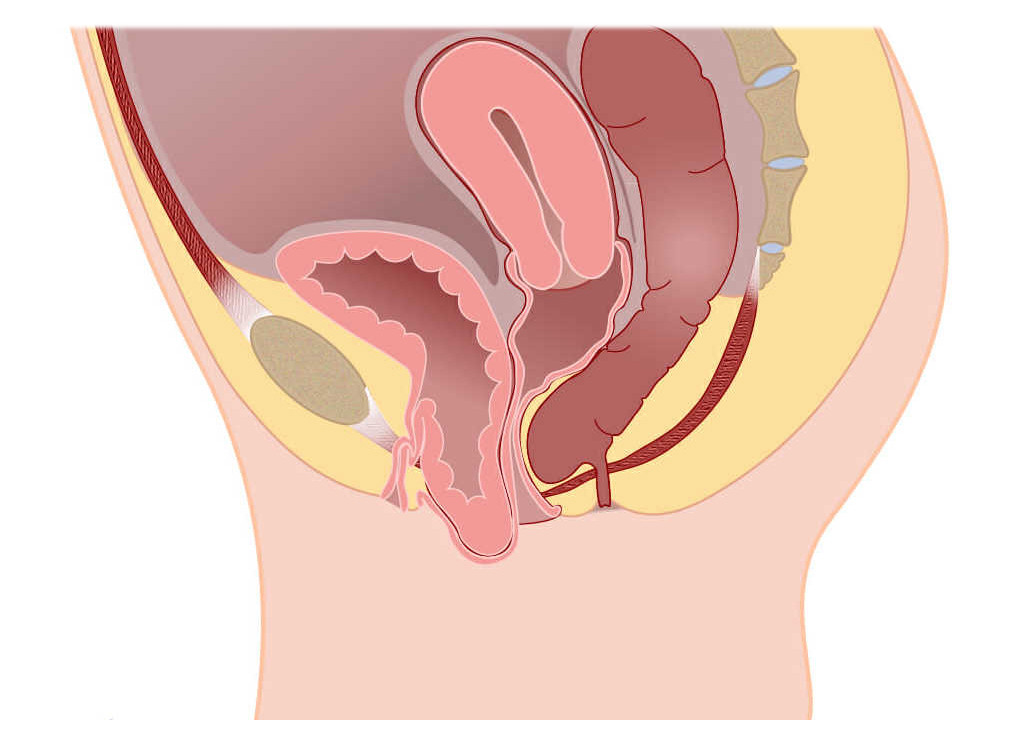
Cystocele is a condition where the bladder descends from its normal position in the pelvis and pushes against the vaginal wall. It is the most common type of pelvic organ prolapse. Experts estimate that nearly half of women who have given birth experience pelvic organ prolapse to varying degrees. Pelvic organ prolapse occurs when the walls of the vagina, the uterus, or both lose their normal supporting tissues, causing the pelvic organs to descend or protrude into the vaginal canal or out of the vaginal opening. Other pelvic organs, such as the bladder or intestines, can also be involved and descend from their normal positions in the body.
Cystocele is a commonly encountered condition. Doctors typically categorize cystocele into several stages:
- Stage 1: Mild cystocele, where the bladder only descends slightly into the vagina.
- Stage 2: Moderate cystocele, where the bladder descends further and reaches the vaginal opening.
- Stage 3: Advanced cystocele, where the bladder protrudes out of the vagina.
Causes
The pelvic floor comprises muscles, ligaments (elastic tissues that connect bones and stabilize joints), and connective tissue that support the bladder and other pelvic organs. Over time, the connection between the pelvic organs and ligaments can weaken, or it may occur due to trauma or injury resulting from the childbirth process or straining habits. When this happens, the bladder can descend and protrude into the vagina.
Factors contributing to the stretching or weakening of muscles and connective tissues in the pelvis include:
- Pregnancy and childbirth, especially vaginal delivery
- Conditions that cause repeated straining or increased pressure in the pelvic area, such as:
- Constipation
- Overweight or obesity
- Heavy lifting
- Chronic coughing or bronchitis
- Aging
- History of pelvic surgery
- Muscle weakness around the vagina due to decreased estrogen hormone levels after menopause
Risk factor
Cystocele can occur in women of all ages; however, the risk increases with age due to the weakening of muscles and body tissues. Other factors that can increase the risk of cystocele include:
- Pregnancy and vaginal childbirth
Women who have had vaginal deliveries, multiple pregnancies, or babies with a high birth weight are at a higher risk of developing cystoceles.
- Menopause
The risk of cystocele increases with age, especially after menopause. After menopause, the body's estrogen production decreases, and estrogen helps maintain the strength of the pelvic floor.
- Genetic factors
Some women are born with weaker connective tissue, which makes them more susceptible to cystocele. Additionally, a family history of pelvic organ prolapse also increases the risk of cystocele.
- Other factors
A history of pelvic surgery such as hysterectomy (removal of the uterus) or pelvic organ prolapse repair surgery, as well as obesity, can increase a woman's risk of developing cystocele.
Symptoms
Many women with cystocele, especially those with mild cases, may not exhibit any symptoms. However, as the severity of cystocele increases, symptoms are more likely to manifest. Symptoms of cystocele include:
- The sensation of heaviness, fullness, pressure, or discomfort in the pelvis or lower abdomen. This sensation is exacerbated when standing, lifting heavy objects, coughing, or throughout the day.
- The sensation of something protruding or descending through the vagina, which may be visible or palpable.
- Lower back pain.
- Recurrent urinary tract infections.
- Increased frequency of urination or difficulty in holding urine.
- Unintentional urine leakage (urinary incontinence).
- The feeling of incomplete bladder emptying after urination.
- Needing to exert pressure to initiate urination.
- Constipation or difficulty in passing stool.
- Requiring manual assistance to elevate the bladder for complete emptying.
- Pain during sexual intercourse.
- Difficulty in inserting or removing tampons or vaginal applicators.
These symptoms often intensify after prolonged periods of standing and may alleviate when lying down.
Diagnosis
To diagnose cystocele, a doctor will conduct a medical interview to gather information about the patient's medical history, perform a physical examination, and recommend diagnostic tests as needed to identify any other issues in the urinary tract. Additional tests that the doctor may suggest include:
- Cystourethrogram or voiding cystogram: This involves an X-ray examination of the bladder while the patient is urinating, with the bladder and urethra outlet filled with contrast fluid. This procedure helps to visualize the shape of the bladder and detect any obstructions in the urinary tract.
- MRI imaging tests: MRI scans can be utilized to assess the stage of cystocele and provide detailed imaging of the pelvic region.
Management
Treatment for cystocele depends on its severity. Mild to moderate cases can often be managed without surgery. However, for more severe cases, surgical intervention may be necessary to ensure proper positioning of the vagina and other pelvic organs. Additionally, treatment considerations take into account the impact on the individual's quality of life, with the doctor evaluating daily activities and functions affected by cystocele.
Treatment options for cystocele include:
- Activity modification: Avoiding activities such as heavy lifting or straining during bowel movements, which can exacerbate cystocele.
- Kegel exercises: Regular pelvic floor muscle exercises can significantly strengthen the pelvic floor muscles and provide benefits.
- Insertion of a vaginal pessary or ring: This is a non-surgical option to support the bladder and maintain its position.
- Surgical procedures: Surgery may be recommended to reposition the bladder if other treatments do not provide lasting relief.
- Hormone replacement therapy: This option can help strengthen the muscles around the vagina and bladder. However, it's essential to consult with a doctor regarding its potential risks and benefits before considering hormone replacement therapy.
Complications
While not life-threatening, cystocele can significantly diminish a woman's quality of life if left untreated. Without intervention, the condition can worsen over time. In severe cases, cystocele may impede urination, leading to potential complications such as kidney damage or infection.
Prevention
While cystocele typically cannot be prevented, there are strategies to alleviate symptoms and mitigate its progression. These include:
- Pelvic floor muscle exercises: Strengthening the pelvic floor muscles through exercises like Kegels can provide support to pelvic organs.
- Maintaining a healthy weight: Excess weight can exert pressure on the pelvis, so adopting a balanced diet rich in fruits and vegetables and engaging in regular exercise can help maintain an ideal body weight.
- Avoiding heavy lifting or lifting correctly: When lifting heavy objects, it's important to use the strength of the legs rather than straining the back or waist.
- Preventing or managing constipation: Consuming an adequate amount of fiber, staying hydrated, and staying physically active can help prevent constipation, which can exacerbate symptoms of cystocele.
- Managing chronic coughing: Seeking treatment for chronic cough or bronchitis and quitting smoking, if applicable, can help reduce strain on the pelvic floor muscles and prevent worsening of cystocele symptoms.
When to see a doctor?
While cystocele typically causes discomfort rather than pain, it can significantly interfere with urinary function. If left untreated, cystocele may lead to a urinary tract infection due to difficulty in urination. If you're experiencing symptoms that disrupt your daily activities or quality of life, it's advisable to consult a doctor for evaluation and appropriate management.
- dr. Yuliana Inosensia
Cystocele. (2022). Retrieved 6 July 2022, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/cystocele
Anterior vaginal prolapse (cystocele) - Symptoms and causes. (2022). Retrieved 11 July 2022, from https://www.mayoclinic.org/diseases-conditions/cystocele/symptoms-causes/syc-20369452
Health, N. (2022). Cystocele | NIDDK. Retrieved 11 July 2022, from https://www.niddk.nih.gov/health-information/urologic-diseases/cystocele
Cystocele (Fallen or Prolapsed Bladder): Symptoms & Treatment. (2022). Retrieved 11 July 2022, from https://my.clevelandclinic.org/health/diseases/15468-cystocele-fallen-bladder#outlook--prognosis