Definition
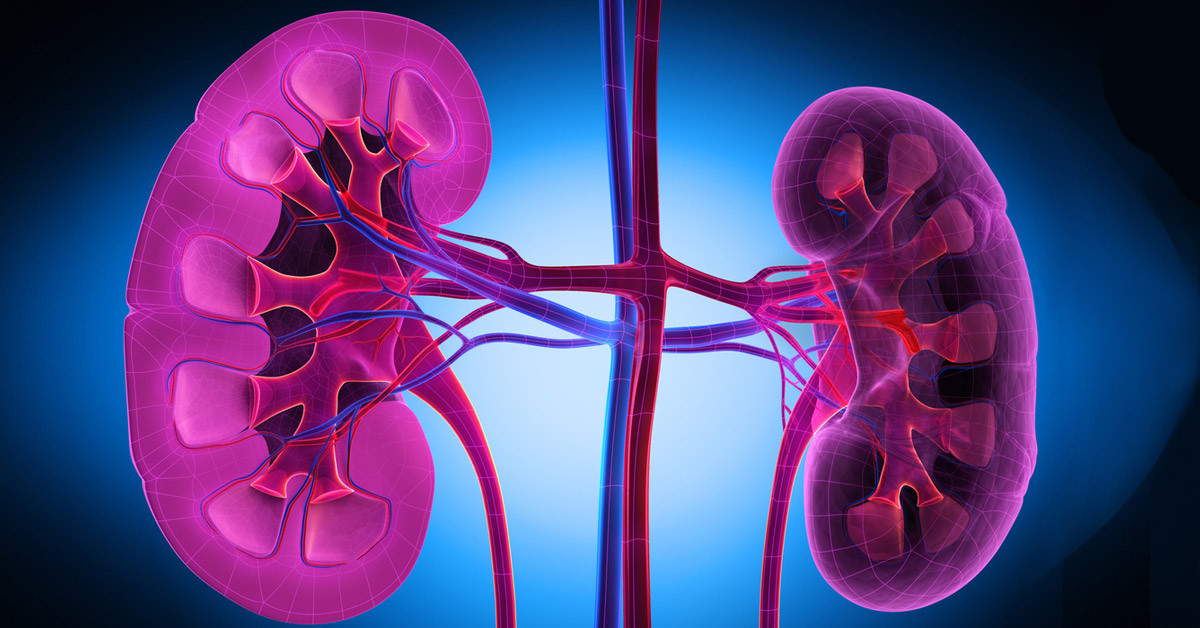
Lupus nephritis is a kidney disease that occurs as a complication of systemic lupus erythematosus (SLE). SLE, or lupus, is an autoimmune disease in which the body's immune system attacks its own organs, including the kidneys. The kidneys are essential for filtering metabolic waste from the blood.
The kidneys play a crucial role in the body by removing metabolic waste from the bloodstream. When this organ is compromised, it can lead to illness. Individuals with impaired kidneys may require regular hemodialysis, which helps cleanse the blood using a filtration machine. In cases of severe kidney damage due to Lupus Nephritis, a kidney transplant may be necessary.
According to multiethnic international studies, lupus nephritis is most commonly found in males, young individuals, and those of African, Asian, and Hispanic ethnicities. A study conducted in Spain revealed that Lupus Nephritis was microscopically diagnosed in 30.5% of patients with SLE (Systemic Lupus Erythematosus). The average age at the diagnosis of Lupus Nephritis was 28.4 years old. The risk of developing Lupus Nephritis is notably higher in younger individuals and males.
Causes
The main cause of Lupus Nephritis is an autoimmune disease called systemic lupus erythematosus (SLE). This condition is characterized by abnormalities in the immune system. Normally, the immune system's job is to protect the body from infections and harmful substances. However, in people with autoimmune disorders like SLE, the immune system loses its ability to distinguish between harmful substances and healthy tissues. As a result, it mistakenly targets and attacks healthy cells and tissues.
SLE can inflict damage on various components of the kidneys, potentially leading to disorders such as interstitial nephritis, nephrotic syndrome, membranous glomerulonephritis, and, ultimately, kidney failure. Additionally, there is a suspicion that certain genetic factors may contribute to the development of Lupus Nephritis. Among the genes associated with lupus nephritis patients are PTPN22, CRP, STAT4, and others.
Risk factor
Several factors increase the risk of lupus nephritis. Some of these risk factors include:
- Hispanic ethnicity
- Being male
- Younger age; studies indicate that children with SLE have a higher risk of kidney involvement than adults
Symptoms
The signs and symptoms of Lupus Nephritis often resemble those of other kidney diseases and may include:
- Dark urine
- Blood in the urine
- Foamy urine
- Increased frequency of urination, especially at night
- Progressive swelling in the legs and ankles
- Weight gain
- High blood pressure
However, in some cases, individuals may not experience any symptoms. Nevertheless, laboratory tests may reveal the following indicators of active Lupus Nephritis:
- Elevated blood creatinine levels
- Reduced levels of albumin
- Presence of protein or sediment in the urine
Diagnosis
Diagnosing lupus nephritis involves a comprehensive approach, including a medical interview, physical examination, and diagnostic tests as necessary and available.
During the medical interview, the doctor will inquire about the patient's signs, symptoms, and medical history, particularly to systemic lupus erythematosus (SLE) and lupus nephritis.
In the physical examination, the doctor will search for clinical signs, such as swelling in the legs and ankles and high blood pressure, common in lupus nephritis cases.
Diagnostic tests for diagnosing lupus nephritis include laboratory tests (urine and blood tests), imaging studies, and biopsy.
In a complete urine examination, visible blood or very foamy urine may be among the initial signs of lupus nephritis. Blood tests such as creatinine and urea may reveal elevated levels in the blood.
Ultrasound examination can help identify abnormal sizes and shapes in the kidneys.
A biopsy is the most accurate but invasive test to confirm kidney disease. During this procedure, a doctor inserts a needle through the abdomen and into the kidney to obtain a tissue sample for analysis, aiming to determine if there are signs of kidney damage.
Management
Currently, there is no known cure for lupus nephritis, and treatment aims to manage the condition and prevent further kidney damage. Early intervention is crucial in halting the progression of kidney damage and may avoid the need for kidney transplantation.
Treatment strategies also focus on alleviating symptoms associated with lupus nephritis. Some approaches include dietary modifications such as reducing protein and salt intake, along with medication to control high blood pressure. Steroids may be prescribed to reduce inflammation and swelling.
Immunosuppressive drugs, like cyclophosphamide or mycophenolate mofetil, may be recommended in certain cases. However, special consideration is necessary for pediatric or pregnant patients. In cases of severe kidney damage, additional management strategies may be required.
Complications
The most severe complication of Lupus Nephritis is kidney failure, which necessitates dialysis or kidney transplantation. Dialysis serves as the initial treatment, albeit not a permanent solution. Over time, many individuals on dialysis will necessitate a kidney transplant. However, the wait for a suitable donor organ can extend from months to years.
Prevention
Currently, there is no meaningful prevention method for avoiding cases of Lupus Nephritis. However, several lifestyle factors may help reduce the risk of developing the condition:
- Maintaining a balanced diet
- Avoiding exposure to cigarette smoke and refraining from smoking
- Limiting alcohol consumption
- Regular exercise
- Ensuring adequate rest and relaxation
When to see a doctor?
If you experience worsening symptoms, such as increasing blood in the urine and worsening swelling in the ankles and feet throughout the day, it's advisable to seek further evaluation from a doctor, either internist or pediatrician.
The doctor will conduct a thorough medical interview, physical examination, and specific diagnostic tests to establish a definitive diagnosis of the underlying disease and determine the appropriate management tailored to your needs.
Looking for more information about other diseases? Click here!
- dr. Yuliana Inosensia
Musa R, Brent LH, Qurie A. Lupus Nephritis. [Updated 2021 Aug 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499817/
Medline Plus. Lupus nephritis. July 2021. https://medlineplus.gov/ency/article/000481.htm
Healthline. Lupus nephritis. August 2018. https://www.healthline.com/health/lupus-nephritis