Definition
Pyelonephritis is a urinary tract infection that affects the kidneys, typically originating from the urethra and bladder and spreading to one or both kidneys. When pyelonephritis is sudden and severe, it is referred to as acute pyelonephritis. This condition can cause kidney swelling and permanent damage, potentially threatening life if not promptly treated, as the infection may spread into the bloodstream.
In cases where infections persist or recur in the kidneys, it is termed chronic pyelonephritis. Although rare, this condition may occur in pediatric patients or individuals with urinary tract obstructions.
Treatment for kidney infections usually involves antibiotics; in some cases, hospitalization may be necessary to ensure proper and timely care.
The estimated incidence of acute pyelonephritis in the United States is approximately 15-17 per 10,000 cases in women and 3-4 per 10,000 cases in men annually. Young, sexually active women are the population most affected by acute pyelonephritis. However, older adults, infants, and pregnant women are also at risk due to anatomical abnormalities, hormonal changes, and other factors. Pregnant women, in particular, have an incidence rate of around 20-30%, with most cases occurring in the second and early third trimesters.
Causes
Pyelonephritis commonly arises from an infection in the lower part of the urinary tract, such as a urinary tract infection (UTI). Bacteria enter the body through the urethra and proliferate, ascending from the bladder to the kidneys. In particular, bacteria like E. coli are frequent culprits in causing this infection. However, severe bloodstream infections can also disseminate to the kidneys, leading to acute pyelonephritis.
Risk factor
Various factors can disrupt normal urine flow, increasing the risk of acute pyelonephritis. Abnormalities in the size or shape of the urinary tract can heighten susceptibility to this condition. Additionally, the shorter length of the female urethra than males facilitates bacterial entry, raising the risk of kidney infection and acute pyelonephritis. Additional risk factors include:
- History of chronic kidney stones or abnormalities in the kidneys or bladder
- Advanced age
- Compromised immune systems, such as those with diabetes, HIV/AIDS, or cancer, reduce the ability to fight off infections
- Men with an enlarged prostate obstruct urine flow and increase the risk of urinary tract infections
- Using urinary catheters introduces bacteria into the urinary tract and increases infection risk
- History of urinary tract surgery, disrupting normal urinary function and increasing susceptibility to infections
- Certain medications that suppress the immune system or affect urinary tract function
- Disorders of the nerves or spinal cord interfere with normal bladder function and urine flow
In chronic pyelonephritis, recurrent urinary tract infections and abnormalities in the anatomy or shape of the urinary tract are potential risk factors. Notably, chronic pyelonephritis is more commonly observed in the pediatric population than in adults.
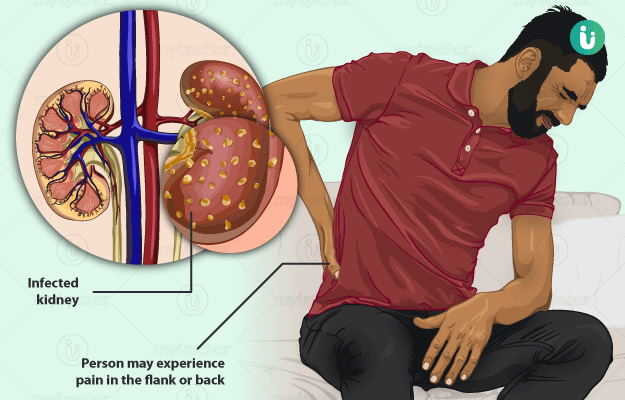
Symptoms
Symptoms o
- Fever with a temperature exceeding 38.9°C
- Abdominal, back, waist, or groin pain
- Pain or burning sensation during urination
- Cloudy yellow urine
- Urine containing pus or blood
- Frequent urination
- Urine with a foul odor
Additional symptoms may include chills, nausea, vomiting, fatigue, muscle aches, and decreased consciousness.
Symptoms may vary in children and the elderly compared to other populations. In the elderly, decreased consciousness is a relatively common complaint and may be the sole symptom of pyelonephritis.
Individuals with chronic pyelonephritis may experience mild symptoms or may remain asymptomatic.
Diagnosis
Diagnosing pyelonephritis typically involves a medical interview, physical examination, and diagnostic tests as needed. During the medical interview, the doctor will inquire about the patient's signs, symptoms, and medical history, paying particular attention to symptoms suggestive of pyelonephritis.
In the physical examination, the doctor will look for clinical signs. In cases of pyelonephritis, doctors may observe fever, indicated by a temperature above 38.0°C measured with a thermometer, or tenderness upon percussion over the affected kidney area, which can be severe and disruptive.
Diagnostic tests for confirming the diagnosis of pyelonephritis include a complete urine examination to assess the presence of bacteria, blood, or pus in the urine, indicating a urinary tract infection. Additionally, imaging studies such as ultrasound or CT scans can help identify the presence of cysts, tumors, or other obstructions in the urinary tract.
Management
Home management of pyelonephritis may involve temporarily relieving pain with paracetamol at the recommended dosage. However, it's crucial to note that this pain reliever does not address the underlying cause of pyelonephritis. Therefore, individuals should promptly seek medical attention at the nearest healthcare facility. Once diagnosed, the treatment of choice is antibiotics, which are the first-line treatment for addressing pyelonephritis. Antibiotic therapy typically lasts for 10-14 days.
If outpatient treatment fails to alleviate symptoms, hospitalization may be necessary. Hospital-based treatment may include intravenous administration of medications, fluid therapy, and continued antibiotic treatment.
Surgical intervention may be considered to manage pyelonephritis in cases of recurrent infections. Surgery aims to remove or correct obstructions or abnormalities in the kidneys or urinary tract.
Complications
Complications that may arise from pyelonephritis include:
- Chronic kidney disease and permanent kidney damage
- Rare cases of bloodstream infection, known as sepsis, which can be life-threatening
- Recurrent kidney infections
- Infections in the surrounding area of the kidneys
- Acute kidney failure
- Kidney abscesses are collections of pus in the kidney
Prevention
Preventive measures for reducing the risk of urinary tract infections, including pyelonephritis, include:
- Drinking adequate water, at least 2 liters per day, increases urine production and flushes bacteria from the urethra
- After intercourse, promptly clean the genital area and urinate to help eliminate bacteria that may have entered the urethra
- When wiping after using the toilet, always wipe from front to back to prevent spreading bacteria from the anus to the urethra
- Avoid using products that can irritate the urethra, such as feminine sprays commonly used by women
When to see a doctor?
If you notice worsening symptoms, it's advisable to seek consultation with a doctor. The doctor will conduct a thorough medical interview, physical examination, and specific diagnostic tests to diagnose the underlying condition precisely and determine the appropriate management tailored to your individual needs.
Looking for more information about other diseases? Click here!
- dr. Yuliana Inosensia
Belyayeva M, Jeong JM. Acute Pyelonephritis. [Updated 2021 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519537/
Healthline. Pyelonephritis. March 2019. https://www.healthline.com/health/pyelonephritis
Mayo Clinic. Kidney infection. July 2022. https://www.mayoclinic.org/diseases-conditions/kidney-infection/symptoms-causes/syc-20353387