Definition
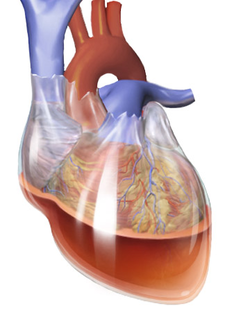
Cardiac tamponade is an emergency heart disease characterized by a build-up of fluid in the pericardial sac, the space between the outermost covering of the heart and the muscle layer of the heart. The presence of fluid in this space can cause pressure on the heart. The additional pressure on the heart can prevent the ventricles from fully expanding to pump blood, making it difficult for the heart to distribute blood throughout the body.
Cardiac tamponade can cause organ failure, shock, and death because the body's organs do not receive adequate blood supply from the heart to function properly. Therefore, cardiac tamponade is a serious and life-threatening medical condition that needs to be treated as soon as possible once diagnosed. If you or someone else is experiencing symptoms and signs of cardiac tamponade, seek medical attention at your nearest health facility for a thorough examination by a doctor.
According to current data, the estimated incidence of cardiac tamponade caused by certain medical conditions is 2 per 10,000 people.
Causes
The fluid buildup in cardiac tamponade can be caused by various factors, including bleeding, infection, tumor tissue, or inflammation of the heart organ. Fluid buildup can include blood, transudate (extracellular fluid from tissues), and exudate (fluid released by blood vessels due to inflammation or cell damage). Some medical conditions that can cause fluid build-up include:
- Aortic aneurysm dissection (partial tearing of the wall lining of an abnormally dilated aortic blood vessel)
- End-stage lung cancer
- Heart attack
- Heart surgery
- Pericarditis (an inflammatory disease of the lining of the heart due to bacterial or viral infection)
- Injury to the heart from a gunshot or stab wound to the chest
- Heart tumors
- Kidney failure
- Leukemia or blood cancer
- Radiation therapy to the chest
- Systemic lupus erythematosus (a skin disease that occurs when the immune system attacks healthy skin cells)
- Heart failure
- Dermatomyositis (an inflammatory disease characterized by muscle weakness and rashes on the surface of the skin)
Risk factor
Several factors can increase a person's risk of developing cardiac tamponade, including:
- Tuberculosis infection or myocarditis (inflammation of the heart muscle lining)
- Autoimmune disease is when the body's immune cells attack the body’s healthy cells
- Cancer disease
- Uremia (elevated levels of urea in the body)
- Other inflammatory diseases such as pericarditis (inflammation of the outer lining of the heart)
- Patients with HIV or end-stage renal failure\
Symptoms
Patients with cardiac tamponade may experience several signs and symptoms, including:
- Anxiety and discomfort in the chest area
- Low blood pressure
- Weakness
- Sharp chest pain that radiates to the neck, shoulders, or back
- Chest pain that intensifies during deep breathing
- Coughing
- Difficult breathing
- Rapid breathing
- Feeling uncomfortable and better when sitting and leaning forward
- Fainting
- Spinning dizziness
- Loss of consciousness
- Pale colored skin
- Gray to bluish
- Rapid heart rate
- Swelling of the legs or abdomen
- Skin may turn yellow
- Sleepiness
- In some cases, the heart rate may become weak or disappear
Diagnosis
The diagnosis of cardiac tamponade can be made through a medical interview, physical examination, and supporting examinations when available and necessary.
Interview and Physical Examination
During the medical interview, the doctor will inquire about the patient's current symptoms and when they began. The doctor will also inquire about the patient's medical history and the treatments they have received. This information is necessary for the doctor to make a specific medical diagnosis.
During the physical examination, the doctor will conduct an examination based on the patient's symptoms in order to identify several clinical signs, which are objective signs obtained by the doctor through physical examination. The doctor will check vital signs such as blood pressure, listen to the patient's heart sounds, and examine the neck veins for dilation. If the necessary equipment is available, the doctor will recommend a supportive examination.
Supporting Examination
Supporting examinations also help to establish or confirm the diagnosis of cardiac tamponade. Supporting examinations that can be done include:
- ECG (electrocardiography)
- Blood test
- Chest X-ray imaging can show images of heart enlargement
- Echocardiography (ultrasound of the heart) can help confirm the presence of cardiac tamponade and determine its size
- CT or MRI of the chest
- Coronary angiography imaging test to see images of the heart's coronary blood vessels
Management
Cardiac tamponade is a serious condition that requires immediate hospitalization. The fluid between the heart's outermost layer and the heart's muscle layer must be removed as soon as possible using specific procedures. A syringe removes as much of the fluid as possible in these procedures. A surgical procedure known as pericardiectomy may also be performed to cut and remove part of the heart’s outer layer (pericardium). In some cases, certain medications may be prescribed.
The most important thing in cases of cardiac tamponade is to determine the exact cause and treat it as best as possible so that it does not occur again.
Complications
Complications that can arise in cardiac tamponade are:
- Heart failure
- Pulmonary edema
- Bleeding
- Shock
- Death
Prevention
There is no specific prevention for cardiac tamponade. However, there are steps you can take to avoid the occurrence or worsening of medical conditions that may be the cause of cardiac tamponade, such as:
- Doing regular dialysis for patients with end-stage renal failure
- Exercise regularly at least 3-5 times per week with a minimum duration of 30 minutes
- Maintain food intake with balanced nutritional food consumption
- Manage stress well
- Routine appointment with a doctor for chronic kidney disease patients
- Quit smoking
- Stop consuming alcohol
When to see a doctor?
Cardiac tamponade is an emergency that requires immediate treatment. If you or a family member experiences symptoms such as chest pain, palpitations, shortness of breath, fainting, or loss of consciousness, seek medical attention right away.
You can also seek further medical attention from a heart and blood vessel specialist or a cardiovascular consultant internal medicine specialist. The doctor will conduct a medical interview, physical examination, and additional tests to determine the exact diagnosis and appropriate treatment.
Looking for more information about other diseases? Click here!
- dr. Yuliana Inosensia
Stashko E, Meer JM. Cardiac Tamponade. [Updated 2021 Dec 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431090/
Medline Plus. Cardiac tamponade. May 2020. Available from: https://medlineplus.gov/ency/article/000194.htm#.
Healthline. Cardiac tamponade. June 2019. Available from: https://www.healthline.com/health/cardiac-tamponade#.