Definition
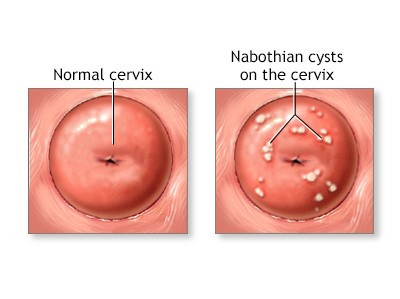
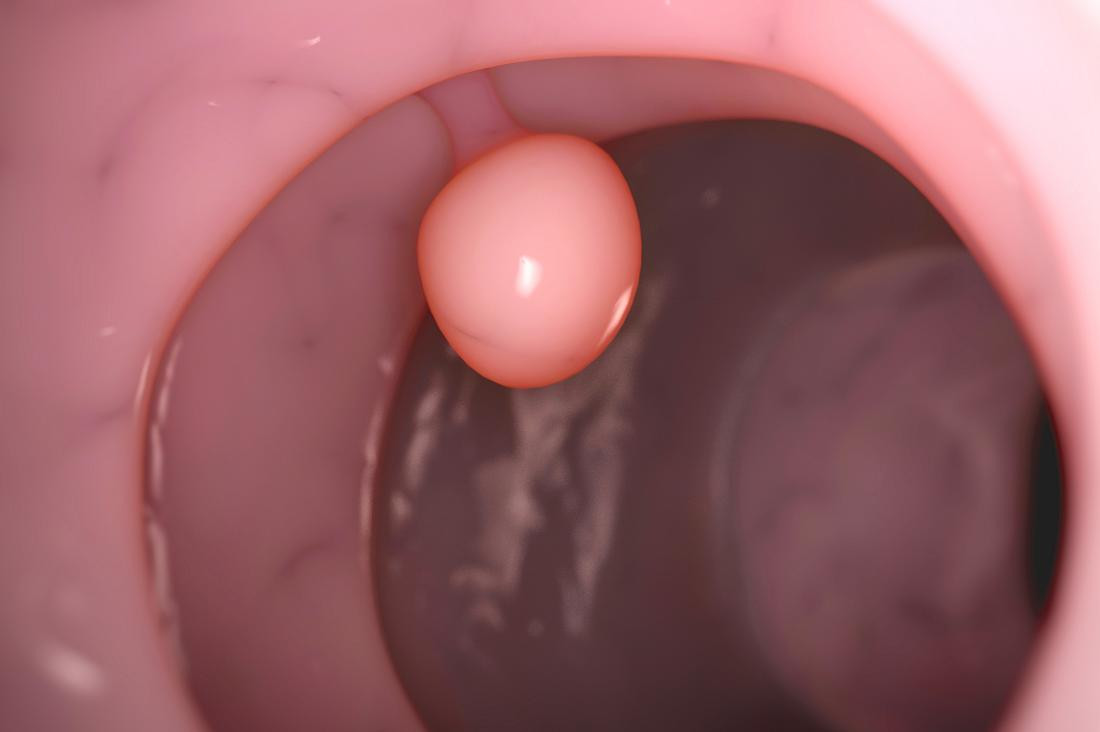
Cervicitis is a condition characterized by inflammation of the cervix, or the neck of the uterus. This inflammation can be caused by irritation, infection, or injury, particularly to the columnar epithelial cells of the cervix.
Inflammation of the cervix can appear suddenly or persist for a long time. These conditions are usually caused by different factors. Cervicitis is a common disease, often associated with sexually transmitted infections. It is estimated that more than half of adult women will experience cervicitis at some point in their lives. Recurrence of cervicitis occurs in about 8–25% of women.
If you are interested in reading more about sexually transmitted infections, you can read it here: Sexual Transmitted Infections - Definition, Cause And Risk Factors.
Causes
The causes of cervicitis are divided into two categories: infectious and non-infectious.
Infectious
Infection is the most common cause of cervicitis. Several infectious agents can cause cervicitis, including bacteria, viruses, fungi, or parasites.
- Bacteria: Chlamydia trachomatis is one of the most frequent causes of cervicitis
- Bacteria: Neisseria gonorrheae
- Virus: Herpes simplex
- Parasite: Trichomonas vaginalis
- Bacteria: Mycoplasma genitalium
- Overgrowth of normal bacteria in the vagina
Non-Infectious
Non-infectious causes of cervical inflammation include:
- Allergic reactions to certain chemicals or products. Latex from condoms and vaginal cleaning fluids can cause allergies.
- Irritation from chemicals like soap and spermicides (chemicals that kill sperm).
- Injury causing cervical trauma, such as the insertion of a device into the uterus or post-surgical procedures.
- Systemic inflammatory diseases are also associated with cervical inflammation.
- Hormonal imbalances, particularly low estrogen and high progesterone, impair the body's ability to maintain healthy cervical tissue.
- Radiation therapy can cause changes in the cervical lining.
Risk Factor
Certain groups of individuals are at a higher risk of cervicitis, including:
- Multiple sexual partners
- High-risk sexual behaviors that increase the chance of sexually transmitted infections
- Early age at first sexual intercourse
- Sexual partners suspected of having sexually transmitted infections and not using condoms
- Previous history of sexually transmitted infections
Symptoms
Most women do not experience symptoms or signs when they have cervicitis. It is often discovered during routine vaginal or uterine examinations. If symptoms do appear, they may include:
- Vaginal discharge that can be bloody, yellow, green, or gray, varying in amount
- Pain during urination or increased frequency of urination
- Pain during sexual intercourse
- Bleeding after sexual intercourse
- Vaginal bleeding outside of menstrual periods
- Itching or irritation in the vaginal area
- Unpleasant odor in the genital area
- Rarely, abdominal or back pain and fever
- Lower back or genital pain
- A sensation of fullness or pressure in the lower abdomen
Diagnosis
If a doctor suspects a disease related to the reproductive organs, they will interview and examine you. First, the doctor will ask about your symptoms and complaints. Questions related to reproductive health may include:
- Sexual behavior
- Genital hygiene
- Contraceptive use
- Pregnancy history
- Previous sexually transmitted infections and cervicitis
The doctor will then perform a physical examination, especially of the lower abdomen, back, genitalia, and uterus. If necessary, to help diagnose and rule out other diseases, the doctor may recommend a vaginal and cervical swab test. Fluid/mucus from the genitalia or cervix will be collected using a swab tool. This test aims to identify the exact cause of cervicitis by analyzing the fluid/mucus sample under a microscope.
Management
Treatment for cervicitis includes both medication and non-pharmacological approaches. The cause of cervicitis must be determined first to decide on the treatment, whether infectious or non-infectious.
Medications for infectious cervicitis depend on the cause. Antibiotics are prescribed if cervicitis is caused by bacteria. It is crucial to complete the antibiotic course to prevent bacterial resistance. Antibiotic therapy may also be recommended for women at high risk of sexually transmitted infections.
Medications can be administered orally or by injection, depending on the severity of cervicitis. Hormonal therapy may be provided if cervicitis is caused by hormonal imbalances, commonly seen in menopausal patients.
Treatment aims to address and prevent complications, especially those caused by infections. Successful treatment depends on adherence to medication, advising sexual partners to undergo treatment, and avoiding sexual intercourse until the treatment is completed and the patient is declared cured.
The doctor will then re-evaluate the effectiveness of the treatment. Generally, cervicitis can be cured within 1-2 weeks with appropriate treatment.
Articles about menopause are available here: Menopause - Definition, Cause And Risk Factor.
Complications
The cervix is part of the uterus and protects the uterus from various infectious agents such as bacteria, viruses, or fungi. Infection of the cervix can spread to the uterus, fallopian tubes, and even the pelvic cavity.
A serious complication of cervicitis is pelvic inflammatory disease (PID). PID causes inflammation and scar tissue formation in reproductive organs such as the ovaries and fallopian tubes.
This condition can lead to:
- Formation of pus-filled sacs (abscesses) in the pelvic cavity or ovaries.
- Persistent infection or pain
- Pregnancy Outside of the Uterus (ectopic pregnancy)
- Infertility issues
Therefore, if you experience the mentioned symptoms, it is crucial to seek treatment to prevent complications.
Prevention
These several preventive measures can help reduce the risk of cervicitis:
- Use condoms to prevent infections
- Be faithful to one partner and avoid having multiple sexual partners
- Seek treatment for sexually transmitted infections and encourage your partner to do the same
- Avoid sexual intercourse with partners showing symptoms of genital discharge
- Avoid using vaginal cleaning products that can irritate the vagina and cervix
- Avoid leaving objects or devices in the vagina for extended periods, such as tampons
When to See a Doctor?
If you experience vaginal discharge or bleeding accompanied by pain and are at risk of sexually transmitted infections, you should see a doctor. You can consult a specialist in dermatology and venereology for further management.
Looking for more information about other diseases? Click here!
- dr. Alvidiani Agustina Damanik
Cervicitis – mountsinai. (2022). Retrieved 5 November 2022, from https://www.mountsinai.org/health-library/diseases-conditions/cervicitis.
What is cervicitis and what causes it? – medicalnewstoday. (2022). Retrieved 5 November 2022, from https://www.medicalnewstoday.com/articles/321666#causes.
Cervicitis – mayoclinic. (2022). Retrieved 5 November 2022, from https://www.mayoclinic.org/diseases-conditions/cervicitis/symptoms-causes/syc-20370814.
Cervicitis – clevelandclinic. (2022). Retrieved 5 November 2022, from https://my.clevelandclinic.org/health/diseases/15360-cervicitis.
Iqbal U, Wills C. Cervicitis – StatPearls. (2022). Retrieved 5 November 2022, from https://www.ncbi.nlm.nih.gov/books/NBK562193/.
Goodman B. Cervicitis – WebMD. (2022). Retrieved 5 November 2022, from https://www.webmd.com/women/guide/cervicitis.