Definition
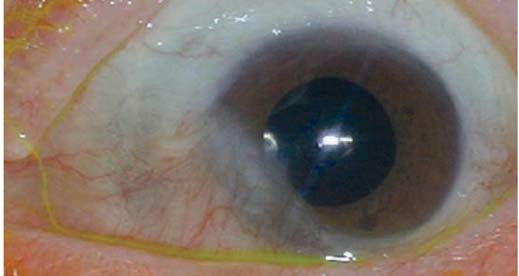
Pseudopterygium, also known as cicatricial pterygium, is a condition characterized by a white layer affecting the conjunctiva and cornea of the eye. This condition resembles pterygium but differs in shape and cause. In pseudopterygium, the layer is firmly attached to the conjunctival and corneal tissue, unlike pterygium, where the white layer can be removed.
In pterygium, the layer appears from the pingecuela or an abnormal layer that grows on the conjunctival layer which is round and yellowish in color. Pseudopterygium results from damage to the corneal tissue at the edge, often caused by trauma such as tearing, burning, or inflammation, leading to the conjunctival tissue adhering to the cornea.
Pseudopterygium often occurs in someone who has experienced a previous traumatic event. This is different from pterygium, where the occurrence is often experienced together with exposure to UV rays from sunlight which is more frequent and felt throughout the day.
Causes
Based on existing data, several conditions have been found that can cause pseudopterygium. Pseudopterygium is most commonly caused by eye trauma involving the conjunctiva. Trauma triggers an inflammatory process on the eye's surface, leading to pseudopterygium formation. Other causes include:
- Corneal ulcer: An open wound on the cornea.
- Conjunctivitis: Inflammation of the conjunctival lining of the eye.
- Contact lens trauma: Often due to insufficient lubrication on the corneal surface.
Risk Factor
Several conditions increase the susceptibility to pseudopterygium, including:
- Trauma to the eye affecting the conjunctiva or cornea.
- Prolonged inflammatory processes in the eye, such as corneal ulcers or conjunctival inflammation.
- Eye surgeries that cause the conjunctiva to adhere to the cornea.
- Use of contact lenses, leading to eye irritation.
Symptoms
Mild pseudopterygium, where the white layer is small, often does not cause symptoms. Symptoms arise if the white membrane covers the visual pathway and may include:
- Presence of white tissue from the conjunctiva to the cornea that cannot be removed with tools.
- Gradual blurred vision due to shifting visual focus.
- Excessive tear production.
- Sensation of a foreign object in the eye.
- Earlier onset of pain symptoms in contact lens users due to wound edges lifting when removing the lens.
- Symptoms typically follow a traumatic event to the eye.
Diagnosis
Diagnosis of pseudopterygium aims to differentiate it from pterygium. One effective examination is the Bowman Probe Test, which assesses the condition under a doctor's supervision. During this test, a probe is inserted under the pseudopterygium layer. In pseudopterygium cases, the probe cannot pass through the white layer, distinguishing it from pterygium.
Management
In asymptomatic cases or those without significant symptoms, patients are advised to use sunglasses when outdoors to avoid exposure to UV rays. For more severe cases, surgery is recommended to remove the pseudopterygium. However, surgical intervention often leads to recurrence, with 80% of patients experiencing repeated symptoms post-surgery. Surgery is considered if:
- Vision in the eye is impaired due to pseudopterygium.
- The pseudopterygium is large and cosmetically disturbing.
- The scar tissue blocks eyeball movement.
The surgical technique involves removing the scar tissue or performing a tissue transplant. Post-surgery care includes using eye protection for a specific period and applying eye drops for about a month.
Complications
Complications of pseudopterygium can include decreased visual acuity due to corneal shifts, such as astigmatism. Surgical procedures sometimes also cause complications. Post-surgical complications may include:
- Recurrence of pseudopterygium, sometimes up to 12 months after surgery. Recurrence rates are higher in patients who do not undergo transplantation at the removal site.
- Corneal abnormalities, such as wounds or perforations.
- Strabismus (misalignment of the eyes).
Prevention
Eye trauma can happen during everyday activities such as cooking or when you play with your children. To prevent pseudopterygium, consider the following actions:
- Use protective gear when playing with small objects or engaging in activities that may cause flying debris.
- Wear protective glasses when handling harsh chemicals like bleach or cleaning fluids.
- Supervise children when they use sharp tools such as scissors, forks, and knives.
- Avoid using toys that shoot projectiles or playing with laser pointers, as lasers can cause temporary or permanent retinal damage.
When to See a Doctor?
Seek medical attention immediately if you experience any of the following eye-related complaints:
- Severe pain in one or both eyes accompanied by sudden visual disturbances.
- Trauma to the eye or eyelid from objects or liquids.
- Difficulty moving one or both eyes.
- Blood in the white part of the eye.
- A foreign object in the eye that is difficult to remove.
These symptoms can indicate eye emergencies, and if left untreated, can lead to prolonged inflammation and other serious complications.
Looking for more information about other diseases? Click here!
- dr Hanifa Rahma
Pseudopterygium | Columbia Ophthalmology. Columbiaeye.org. (2021).
Pseudopterygium. EyeRounds.org: Online Ophthalmic Atlas. Webeye.ophth.uiowa.edu. (2021).
Pterygium - Europe. American Academy of Ophthalmology. (2021).
Byrd, L., & Martin, N. (2021). Corneal Ulcer. Ncbi.nlm.nih.gov.
Nuzzi, R., & Tridico, F. (2018). How to minimize pterygium recurrence rates: clinical perspectives. Clinical Ophthalmology, Volume 12, 2347-2362. https://doi.org/10.2147/opth.s186543
Strabismus (Crossed Eyes): Types, Causes, Symptoms & Treatment. Cleveland Clinic. (2021).
Tips for avoiding eye injuries at home. Mayo Clinic. (2021).