Definisi
Perforasi/ruptur kornea adalah perlubangan kornea yang dapat disebabkan oleh berbagai hal. Biasanya, hal ini terjadi sebagai komplikasi dari berbagai kondisi pada mata ataupun bagian tubuh lainnya. Namun, hal ini tidak menutup kemungkinan bahwa perforasi kornea disebabkan oleh trauma. Perforasi kornea merupakan kegawatdaruratan, sehingga jika Anda mencurigai diri Anda atau orang di dekat Anda mengalami perforasi kornea, segeralah bawa ke IGD terdekat.
Penyebab
Penyebab perforasi kornea dapat dibagi ke dalam 2 jenis: trauma dan non trauma. Pada perforasi kornea akibat trauma, trauma dapat disebabkan oleh penyebab eksternal atau pembedahan. Penyebab eksternal yang dapat menyebabkan perforasi kornea adalah benda-benda yang mengenai mata dengan kecepatan tinggi serta kail ikan yang digunakan saat memancing. Sementara itu, pembedahan yang berisiko menyebabkan perforasi kornea adalah pengambilan benda asing kornea dan pembedahan lainnya seperti katarak dan glaukoma.
Penyebab perforasi kornea non-trauma dapat dibagi lagi menjadi dua, yaitu keratitis dan penyakit sistemik lainnya (mempengaruhi beberapa atau seluruh tubuh). Keratitis merupakan peradangan pada kornea yang dapat terjadi akibat infeksi bakteri atau jamur. Namun, yang tersering merupakan infeksi bakteri, terutama Pseudomonas, Haemophilus, dan Moraxella. Keratitis yang terjadi tanpa didahului infeksi dapat terjadi akibat kerusakan saraf pada kornea, kerusakan bagian pinggir kornea, serta akibat rosacea (kemerahan pada kulit terutama kulit wajah).
Penyakit sistemik yang dapat menyebabkan perforasi kornea adalah penyakit-penyakit degeneratif atau distrofi. Penyakit degeneratif adalah penyakit-penyakit yang menyebabkan kerusakan struktur pada tubuh secara tidak normal sehingga fungsinya menjadi terhambat. Sementara itu, distrofi merupakan kelainan bentuk atau struktur yang berpotensi merugikan. Penyakit autoimun seperti Sjogren dan rheumatoid arthritis (RA) dapat pula merusak kornea sehingga berisiko pada terjadinya perforasi kornea.
Faktor Risiko
Faktor risiko perforasi kornea akan tergantung dari penyebabnya. Misalnya, orang tanpa kondisi spesifik akan lebih rentan terhadap perforasi kornea akibat trauma ataupun infeksi. Sementara itu, orang dengan penyakit seperti yang telah disebutkan pada bagian Penyebab akan lebih rentan mengalami perforasi kornea sebagai komplikasi dari penyakit tersebut. Penyakit-penyakit terkait perforasi kornea tersebut pun memiliki faktor risiko yang berbeda-beda, misalnya rheumatoid arthritis dan Sindrom Sjogren lebih umum terjadi pada wanita.
Jika Anda memiliki riwayat pembedahan mata atau memiliki luka pada kornea, hal ini meningkatkan risiko Anda mengalami perforasi kornea.
Gejala
Gejala yang umum terjadi pada perforasi kornea adalah gangguan penglihatan, nyeri pada mata, serta mata berair. Mata berair ini perlu ditelusuri lebih lanjut karena dapat disebabkan oleh kebocoran bola mata bagian depan. Pada umumnya, keluhan mata berair ini muncul berulang. Jika sebelumnya Anda mengalami infeksi, mata dapat pula bernanah.
Diagnosis
Diagnosis perforasi kornea dapat dilakukan oleh dokter. Dokter biasanya akan menanyakan riwayat trauma ataupun infeksi, serta penyakit lainnya. Jika terdapat riwayat trauma, dokter akan memeriksa bagian mata lainnya seperti kelopak mata bagian dalam untuk memastikan luas daerah yang terdampak oleh trauma tersebut. Jika terdapat riwayat infeksi, dokter dapat meminta pemeriksaan laboratorium seperti pemeriksaan darah lengkap, hitung jenis sel darah putih, serta kultur bakteri dan jamur.
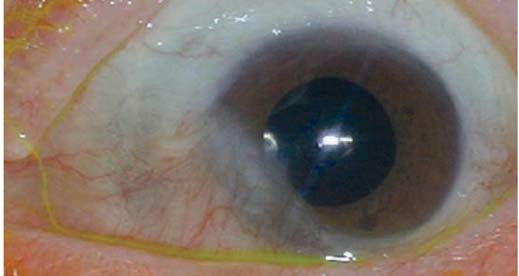
Selanjutnya, dokter dapat melakukan pemeriksaan bola mata depan untuk mencari penipisan atau pendangkalan bagian tersebut. Pemeriksaan akan dilakukan pada dua mata, terutama bila penyebab berupa kondisi sistemik. Selain itu, dokter dapat menggunakan zat pewarna untuk dua hal: pertama, mengetahui lokasi dan besar lubang pada kornea; kedua, untuk melihat apakah ada kebocoran cairan dari bagian depan bola mata. Dokter dapat melakukan pemeriksaan ini sambil menekan bola mata, karena kebocoran tersebut terjadi sebagai akibat dari peningkatan tekanan bola mata, meskipun kecil. Selain itu, dokter juga dapat menemukan adanya pigmen selaput pelangi pada bagian kornea yang berlubang.
Jika ada infeksi atau peradangan, dokter kemungkinan perlu menangani hal tersebut sebelum dapat mendiagnosis perforasi kornea. Hal ini disebabkan oleh kemungkinan jaringan mati menutupi bagian kornea yang mengalami perforasi.
Tata Laksana
Tata laksana pada perforasi kornea sangat bergantung dari penyebab dan ukurannya. Jika penyebab perforasi kornea adalah trauma, dokter akan mengecek terlebih dahulu. Jika penyebab perforasi kornea adalah infeksi, dokter akan meresepkan antibiotik salep untuk dioleskan pada mata. Sementara itu, jika penyebab perforasi adalah penyakit sistemik, dokter spesialis mata dapat merujuk Anda ke dokter spesialis lainnya seperti penyakit dalam untuk menangani kondisi tersebut.
Perforasi kornea dapat dicegah dan ditangani dengan pengeleman kornea menggunakan zat khusus. Zat ini berfungsi untuk mempercepat pertumbuhan jaringan kornea serta mencegah terjadinya infeksi pada mata. Pilihan pembedahan lainnya dapat dilakukan dengan mengambil jaringan dari konjungtiva (lapisan bening pada permukaan mata dan bagian dalam kelopak mata) atau bagian lainnya, kemudian dijahit. Pembedahan-pembedahan ini terutama dilakukan jika perforasi cukup parah dan berukuran besar. Penggunaan lensa kontak dan lapisan ketuban dapat pula membantu proses ini.
Selain itu, vitamin C dapat pula diberikan karena vitamin C mendukung sintesis kolagen, zat yang diperlukan dalam pembentukan jaringan pelindung pada mata. Jika perforasi cukup kecil, dokter dapat memberikan obat untuk mengurangi cairan dalam bola mata agar tidak bocor. Pada umumnya, perforasi yang berukuran kecil dapat sembuh sendiri.
Dokter juga dapat menyarankan Anda untuk dirawat inap agar dapat melakukan pemantauan. Pemantauan ini dapat dilakukan untuk mencegah cairan dalam bola mata mengalir kembali keluar, serta untuk memantau respon Anda terhadap pemberian antibiotik.
Komplikasi
Komplikasi lanjutan dari perforasi kornea terkait dengan sifatnya yang memaparkan bola mata terhadap dunia luar yaitu endoftalmitis, infeksi pada lapisan dalam bola mata. Selain itu, kerusakan kornea dapat mempengaruhi jaringan yang diperlukan untuk sistem aliran cairan pada bola mata, sehingga dapat menyebabkan glaukoma atau peningkatan tekanan pada bola mata. Selain itu, komplikasi lainnya perdarahan pada lapisan koroid (lapisan yang menyuplai darah di bola mata). Komplikasi ini masing-masing dapat berujung pada kebutaan.
Pencegahan
Pencegahan perforasi kornea akibat trauma sulit untuk dilakukan karena sifat trauma yang seringkali terjadi tanpa disengaja. Sementara itu, jika Anda mengetahui bahwa Anda memiliki keratitis atau luka pada kornea, segeralah ke dokter sebelum kerusakan kornea menjadi lebih parah hingga menyebabkan perforasi. Jika Anda memiliki kondisi penyakit autoimun atau degeneratif, Anda dapat dirujuk oleh dokter untuk melakukan pemeriksaan mata. Selanjutnya, jika diketahui terdapat penipisan pada kornea, Anda dapat menjalani prosedur untuk menempelkan kornea.
Kapan Harus ke Dokter?
Jika Anda mengalami gejala seperti gangguan penglihatan disertai mata berair terus-menerus (umumnya tidak disertai dengan mata merah) setelah terbentur suatu benda, atau disertai dengan mata bernanah, atau memiliki kondisi autoimun, segeralah ke dokter. Perforasi kornea memiliki komplikasi yang dapat menyebabkan kebutaan jika tidak ditangani dengan cepat, sehingga sebaiknya Anda tidak menunda untuk ke dokter.
Mau tahu lebih lanjut seputar penyakit-penyakit lainnya? Cek di sini, ya!
- dr Ayu Munawaroh, MKK
Corneal Perforation | Columbia Ophthalmology. (2021). Retrieved 24 October 2021, from https://www.columbiaeye.org/education/digital-reference-of-ophthalmology/cornea-external-diseases/surgery-complications/corneal-perforation.
Deshmukh, R., Stevenson, L., & Vajpayee, R. (2020). Management of corneal perforations: An update. Indian Journal Of Ophthalmology, 68(1), 7. doi: 10.4103/ijo.ijo_1151_19.
Weiner, G. (2016). Corneal Perforations. Retrieved 24 October 2021, from https://www.aao.org/eyenet/article/corneal-perforations.