Definition
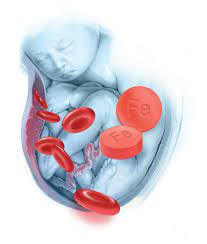
Anemia during pregnancy is characterized by a deficiency of red blood cells, which can impair the delivery of oxygen to tissues in both the mother's body and the developing fetus.
Pregnancy triggers numerous physiological changes in the mother's body to create an optimal environment for the growing fetus. For instance, blood volume increases by approximately 20-30% to accommodate the needs of the developing fetus. However, if the body lacks essential nutrients such as iron or vitamins, it may struggle to produce an adequate number of red blood cells to meet the demands of pregnancy.
Many women experience iron deficiency in the second and third trimesters, leading to mild anemia, which is common during pregnancy. However, severe anemia can pose risks during pregnancy and childbirth. It may increase the mother's likelihood of experiencing bleeding complications during childbirth.
Causes
Anemia in pregnancy can be caused by various factors, primarily due to a deficiency in essential nutrients required for the production of hemoglobin, the protein responsible for transporting oxygen in red blood cells. As the oxygen demand increases for both the mother and fetus during pregnancy, the need for nutrients like iron also rises. Here are some types of anemia commonly encountered during pregnancy:
- Iron deficiency anemia
This type occurs when the body lacks sufficient iron to produce hemoglobin adequately. If the increased demand for oxygen-carrying blood is not met by a corresponding increase in iron intake or reserves, anemia may develop. Iron deficiency anemia is the most prevalent form of anemia during pregnancy.
- Folate deficiency anemia
Folate, a vitamin found naturally in foods like leafy green vegetables, is essential for producing new cells, including healthy red blood cells. Pregnant women require additional folate intake beyond their daily dietary intake. Typically, doctors recommend folic acid supplements during pregnancy to ensure adequate folate levels. Insufficient folate levels can hinder the production of red blood cells, leading to anemia.
- Vitamin B12 deficiency anemia
Vitamin B12 is another crucial nutrient for forming healthy red blood cells. Deficiency in vitamin B12 occurs when pregnant women do not consume enough vitamin B12-rich foods like meat, poultry, dairy products, or eggs. Vegetarians and vegans who exclude these foods from their diet are particularly at risk of vitamin B12 deficiency anemia.
Risk factor
All pregnant women are susceptible to anemia due to the increased demand for iron and folic acid in their bodies compared to when they are not pregnant. However, the risk of anemia during pregnancy is heightened if you:
- Are pregnant with twins or multiple fetuses.
- Have short intervals between pregnancies.
- Experience frequent vomiting, which can lead to nutrient depletion.
- Are teenagers during pregnancy, as adolescents may have higher nutritional needs.
- Consume a few foods rich in iron.
- Have a history of anemia before pregnancy.
- Experience heavy bleeding during menstruation, which may indicate a predisposition to iron deficiency.
Symptoms
Symptoms of anemia may not manifest when the condition is mild. However, the following symptoms may occur with anemia:
- Pale skin, lips, and nails.
- Feeling tired or weak.
- Dizziness or lightheadedness.
- Headaches.
- Shortness of breath.
- Rapid heartbeat.
- Difficulty concentrating.
- Pica, a craving to eat non-food items such as ice, coffee grounds, or paper.
- Low blood pressure.
Diagnosis
Pregnant women typically undergo routine prenatal check-ups to monitor their health and the fetus. During these visits, doctors inquire about any pregnancy-related complaints and conduct a physical examination.
Anemia, characterized by a deficiency of red blood cells, is detected through blood tests. Doctors primarily assess hemoglobin levels to determine if they are within the normal range or decreased. Additionally, the hematocrit level, which measures the percentage of red blood cells in the blood sample, is also evaluated.
Further blood tests may be performed to ascertain whether anemia is due to iron deficiency or other factors.
Management
Typically, prenatal supplements already contain iron and folic acid. However, if you're diagnosed with iron deficiency anemia, your doctor may prescribe additional iron supplements.
Pregnant women are also encouraged to increase their intake of foods rich in iron and folic acid. Some sources of iron include:
- Red meat
- Poultry products
- Fish
- Green leafy vegetables
- Dried beans
To enhance iron absorption, pregnant women can also consume foods or drinks high in vitamin C, such as orange juice, tomato juice, strawberries, kiwi, or bell peppers.
Additionally, pregnant women will be advised to have regular prenatal check-ups and undergo blood tests after treatment. From the blood tests performed, it will be observed whether their hemoglobin and hematocrit levels increase or if the therapy being administered is still ineffective.
Complications
Severe iron deficiency anemia during pregnancy, if left untreated, can lead to serious complications, including:
- Premature birth (birth before 37 weeks of pregnancy).
- Low birth weight of the baby.
- Increased risk of significant bleeding requiring a blood transfusion.
- Postpartum depression.
- Anemic baby.
- Delayed child development.
- Infant death before or shortly after birth.
Similarly, untreated folate deficiency anemia can elevate the risk of premature birth or low birth weight in babies. Babies may also be born with congenital spinal cord defects, such as spina bifida, where parts of the brain or spinal cord protrude from the baby's back due to the failure of the neural tube to close. Neural tube defects can also arise as a complication of vitamin B12 deficiency anemia during pregnancy.
Prevention
To prevent anemia during pregnancy, pregnant women need to ensure they receive adequate nutrition, particularly iron and folate. If you are planning a pregnancy, you can start consuming foods rich in iron and folate.
It is advisable to include at least three servings of iron-rich foods in your daily diet, such as:
- Lean red meat, poultry, and fish.
- Leafy green vegetables like spinach or broccoli.
- Iron-fortified cereals and grains.
- Legumes, tofu, and eggs
Foods rich in vitamin C can enhance iron absorption in the body. For instance, pairing iron-rich foods with sources of vitamin C can be beneficial. For breakfast, consider having rice with fish, spinach, and eggs along with a glass of orange juice.
In addition to consuming vitamin C-rich foods, it's important to include folate-rich foods in your diet to prevent folate deficiency. These foods include:
- Leafy green vegetables.
- Fruits such as oranges or orange juice.
- Dried beans.
- Fortified bread and cereals with folate.
Furthermore, it's crucial to follow your doctor's advice regarding prenatal vitamin consumption, ensuring they contain adequate amounts of iron and folate. Vegetarian women should consult with their doctor about supplementing with vitamin B12 during pregnancy and breastfeeding.
When to see a doctor?
Anemia may not present noticeable symptoms at the onset. Therefore, it's crucial to undergo routine blood tests during your prenatal visits to check for anemia. These tests can detect anemia early, allowing for prompt intervention and management.
Looking for more information about other diseases? Click here!
- dr. Yuliana Inosensia
Anemia in Pregnancy: Causes, Symptoms, and Treatment. (2022). Retrieved 7 October 2022, from https://www.webmd.com/baby/guide/anemia-in-pregnancy.
Prevent iron deficiency anemia during pregnancy. (2022). Retrieved 7 October 2022, from https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/anemia-during-pregnancy/art-20114455.
Anemia and Pregnancy. (2022). Retrieved 7 October 2022, from https://www.hematology.org/education/patients/anemia/pregnancy.