Definition
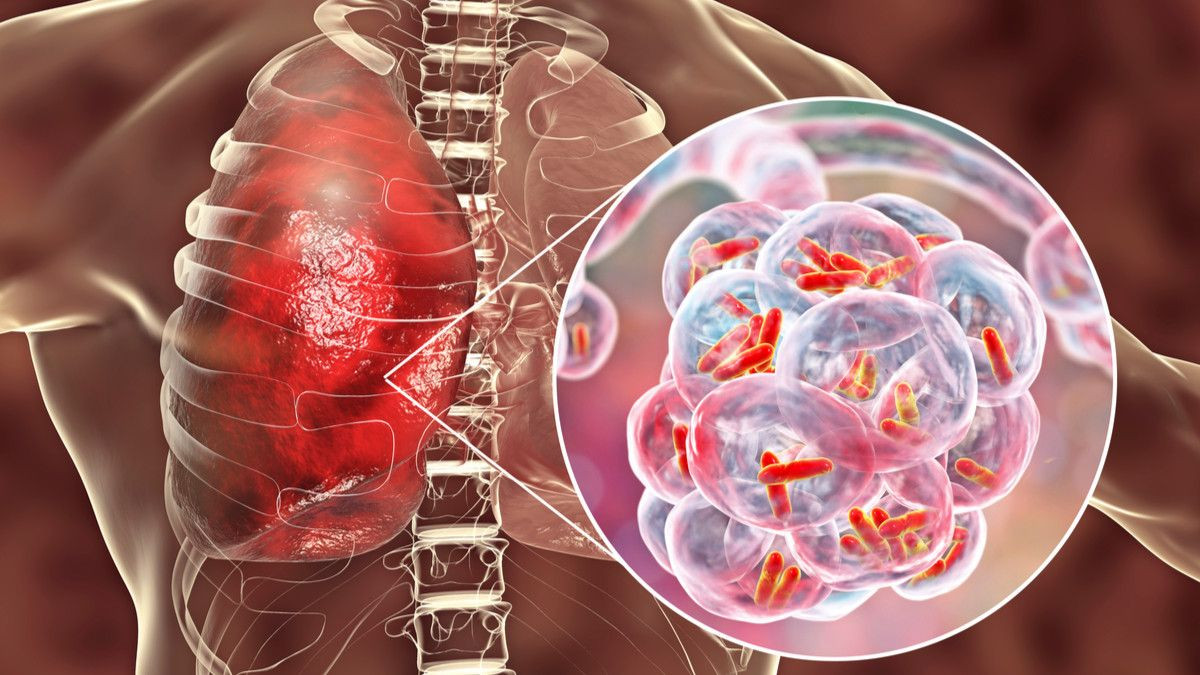
Pneumonia is an inflammation of the lungs, most commonly caused by bacterial infection. Meanwhile, community-acquired pneumonia (CAP) is a type of pneumonia found outside hospitals or other healthcare facilities. Someone is said to have community-acquired pneumonia if they are infected with pneumonia and do not have a history of hospitalization or treatment at other healthcare facilities within a recent period. Community-acquired pneumonia is the most common type of pneumonia.
Causes
Pneumonia is a common disease that infects millions of people each year. Microorganisms such as bacteria, viruses, and fungi can cause pneumonia. In adults, bacteria are the most common cause of pneumonia.
Some ways microorganisms can enter the lungs include:
- Bacteria and viruses that normally live in the nose, sinuses, or mouth can spread to the lungs.
- Inhaling microorganisms from the air directly into the lungs.
- Inhaling food, fluids, or vomit into the lungs (aspiration pneumonia).
Pneumonia can be caused by many types of microorganisms, including:
- Bacteria. The most common cause of bacterial pneumonia is Streptococcus pneumoniae (pneumococcus). Bacterial pneumonia can occur on its own or develop after a patient has a cold or the flu. Bacterial pneumonia can affect one part (lobe) of the lungs, called lobar pneumonia.
- Bacteria-like organisms. Mycoplasma pneumoniae can also cause pneumonia. This type of pneumonia usually causes milder symptoms than other types of pneumonia.
- Fungi. Fungal pneumonia most commonly occurs in people with chronic or long-term illnesses, patients with weakened immune systems, and in people who inhale large amounts of organisms. Fungal pneumonia-causing organisms can be found in soil or bird droppings and vary depending on geographical location. Examples of fungi that cause pneumonia include Pneumocystis jirovecii.
- Viruses, including SARS-CoV-2. Some viruses that cause colds and influenza can also cause pneumonia. Viruses are the most common cause of pneumonia in children under 5 years old. Viral pneumonia is usually mild. However, some cases can develop into serious conditions, such as pneumonia in Covid-19.
Risk factor
Pneumonia risk factors include:
- Chronic lung diseases, such as COPD, bronchiectasis, and cystic fibrosis.
- Smoking.
- Dementia or cognitive decline in the elderly, stroke, brain injury, cerebral palsy, or other brain disorders.
- Immune system problems, such as undergoing cancer treatment, HIV/AIDS, or organ transplantation.
- Other serious illnesses, such as heart disease, liver cirrhosis, or diabetes.
- Recent surgery or trauma.
- Surgery to treat mouth, throat, or neck cancer.
Symptoms
The most common symptoms of pneumonia are:
- Cough, sometimes with green or yellow mucus, or even bloody mucus.
- Fever, ranging from mild to high.
- Chills.
- Shortness of breath, usually occurring during activity.
Other symptoms include:
- Confusion, especially in older people.
- Excessive sweating and clammy skin.
- Headache.
- Loss of appetite, lack of energy, and fatigue.
- Malaise (feeling unwell).
- Sharp or stabbing chest pain that worsens when breathing in or coughing.
- White nail syndrome or leukonychia.
Diagnosis
In diagnosing pneumonia, doctors will inquire about symptoms and medical history, perform a physical examination, and conduct diagnostic tests. In a physical examination, the doctor will listen for abnormal breath sounds in the lungs using a stethoscope. In pneumonia, additional low-pitched breath sounds called rhonchi may be heard due to airway blockage by mucus. Rhonchi can be heard during inhalation and exhalation.
If pneumonia is suspected, the doctor will recommend a chest X-ray. Other tests that may also be performed include:
- Arterial blood gas test, to assess the amount of oxygen in the lungs that can enter the blood.
- Blood and sputum cultures, to look for microorganisms that may cause pneumonia.
- Complete blood count, to check the number of white blood cells. An increase in these cells and certain types of white blood cells may indicate bacterial infection.
- Chest CT scan.
- Bronchoscopy, which involves looking into the throat and lungs using a flexible tube with a camera at the end. Images will be displayed on a screen.
- Thoracentesis, which involves removing fluid from the space between the lung lining.
- Nasopharyngeal swab to assess viruses such as influenza and SARS-CoV-2.
Management
Doctors must determine whether patients need hospitalization or can be treated as outpatients. If hospitalization is required, patients will receive:
- Fluids and antibiotics through intravenous infusion.
- Oxygen therapy.
- Respiratory care as needed.
In bacterial pneumonia, patients should start antibiotic therapy immediately upon hospital admission. In contrast, for viral pneumonia, antibiotics will not be given because antibiotics do not kill viruses. You may be prescribed other medications, such as antivirals if you have influenza.
Most likely, patients will be hospitalized if they:
- Have other serious illnesses.
- Have severe symptoms.
- Are unable to care for themselves at home.
- Are unable to eat and drink.
- Are over 65 years old.
- Have used antibiotics at home but their condition has not improved.
Most cases can still be managed at home. If so, the doctor may prescribe medications including antibiotics in tablet form.
Things to note when taking antibiotics:
- Take antibiotics as directed by your doctor.
- Take antibiotics until they are finished, even when you start to feel better.
- Do not take cough medicine or cold medicine without a doctor's permission, as coughing can help remove mucus from the lungs.
Inhaling warm and moist air can help loosen mucus that may make your throat uncomfortable. The following can help reduce your symptoms:
- Place a warm, wet washcloth over your nose and mouth.
- Fill an air humidifier with warm water and breathe in the warm air slowly.
- Take deep breaths 2 or 3 times every hour. Deep breathing will help open your lungs.
- Tap your chest gently several times while lying down with your head lower than your chest. This action helps remove mucus from the lungs so you can cough it up.
Drink plenty of fluids, as long as your doctor does not limit them.
- Drink water, juice, or thin tea.
- Drink at least 6 to 10 glasses of water (1.5 to 2.5 liters) a day.
- Do not drink alcohol.
Get enough rest when you get home. If you have trouble sleeping at night, you can add a nap.
Complications
With treatment, most people will improve within 2 weeks. Older adults or seriously ill individuals may require longer treatment. Those who usually need longer treatment include:
- Elderly people.
- People whose immune systems do not function properly.
- People with other serious illnesses, such as diabetes or liver cirrhosis.
- In all of the above conditions, pneumonia can be fatal if severe.
In rare cases, more serious problems may develop as a result of pneumonia, including:
- Life-threatening lung changes that require breathing assistance.
- Formation of fluid between the lung membranes (pleural effusion).
- Formation of pus between the lung membranes (empyema).
- Lung abscess, a collection of pus in lung tissue.
Your doctor will perform another chest X-ray to ensure your lungs are clear. Generally, it takes several weeks for your chest X-ray to clear, and you usually start feeling better before your chest X-ray clears.
Prevention
You can prevent pneumonia by following these steps:
- Wash your hands frequently, especially:
- Before preparing and eating food.
- After blowing your nose.
- After using the toilet.
- After changing a baby's diaper.
- After contact with sick people.
- Avoid contact with sick people.
- Do not smoke. Tobacco damages the lungs' ability to fight infection.
- Vaccines can help prevent some types of pneumonia. Be sure to get the following vaccines:
- Flu vaccines can prevent pneumonia caused by the influenza virus.
- Pneumococcal vaccine reduces the likelihood of pneumonia caused by Streptococcus pneumoniae.
- Covid-19 vaccine.
Vaccines are especially important for older adults and people with diabetes, asthma, emphysema, HIV, cancer, organ transplant recipients, or other long-term illnesses.
When to see a doctor?
Consult with the doctor if you have:
- Cough that emits bleeding or carat-like mucus
- Symptoms of worsening respiratory symptoms
- Chest pain worsens while coughing or breathing
- Fast breathing or pain
- Unexplainable night sweat or weight loss
- Shortness of breath, chills of cold, or persistent fever
- Signs of pneumonia in the condition of the weakened immune system, for example, in people with HIV or chemotherapy patients
- Menyeburuknya gejata setelah perbaikan awal
- dr. Yuliana Inosensia
Community-acquired pneumonia in adults. (2020). Retrieved 28 February 2022, from https://medlineplus.gov/ency/article/000145.htm
Baer SL. (2022). Community-acquired pneumonia (CAP). Retrieved 28 February 2022, from https://emedicine.medscape.com/article/234240-overview
Ramirez JA. (2021). Overview of community-acquired pneumonia in adults. Retrieved 28 February 2022, from https://www.uptodate.com/contents/overview-of-community-acquired-pneumonia-in-adults#H3873548286
Pneumonia. (2020). Retrieved 28 February 2022, from https://www.mayoclinic.org/diseases-conditions/pneumonia/symptoms-causes/syc-20354204#:~:text=Community%2Dacquired%20pneumonia&text=It%20may%20be%20caused%20by,a%20cold%20or%20the%20flu.
Regunath H, Oba Y. (2021). Community-Acquired Pneumonia. Retrieved 28 February 2022, from https://www.ncbi.nlm.nih.gov/books/NBK430749/