Definition
Venous thromboembolism (VTE) occurs when a blood clot forms in the vein. Thromboembolism is derived from two words, they are thrombo and embolism. "Thrombo" means blood clot, whereas "embolism" means a specific particle that causes the blockage. Vein thromboembolism means a blood clot that forms in a vein causing a blockage of blood flow.
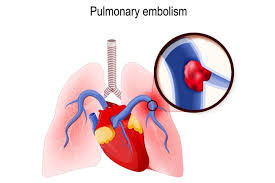
Venous embolism is a combination of two diseases, namely deep vein thrombosis (DVT) and pulmonary embolism (PE). A blood clot in the leg is known as deep vein thrombosis (DVT), whereas a blood clot that flows to block a blood vessel in the lung is known as pulmonary embolism (PE).
The veins carry carbon dioxide-rich blood from other organs to the heart. If the veins are blocked, the blood cannot flow smoothly and the flow is obstructed. This restricted blood flow can lead to inflammation and cell death as the organs do not get the oxygen and nutrients they need.
In the United States, venous embolism is the third most common vascular disease. Every year, approximately one in every 1000 Americans suffers from a venous embolism. Half of these patients develop a pulmonary embolism. About 25% of pulmonary embolism patients die from the condition. From the age of 40, your risk of developing venous embolism doubles every decade.
Causes
Venous embolism is caused by impaired blood flow. Blood clots can form as a result of slow blood circulation. This can be caused by various factors, including certain illnesses, medications, lack of movements (immobilization), and prolonged flights where your legs cannot move freely.
Other causes of venous embolism include:
- Infection
- Medical treatment. Some medical treatments, such as chemotherapy or major surgery (knee or pelvis), may increase the risk of venous thromboembolism
- Medical conditions. Venous embolism is more common in cancer, lupus, and other immune-compromised patients
- Medications. Hormonal therapy and birth control pills may increase the risk of venous embolism
Risk Factor
Factors that can increase the risk of venous embolism include:
- Venous injuries caused by fracture or surgery
- Infection
- Slow blood flow due to limited movement
- Family history of venous thromboembolism
- High estrogen due to pregnancy, taking certain birth control, or hormonal therapy
- Having a blood clotting disorder, such as Factor V Leiden disease, polycythemia vera, or sickle cell disease
- Having other chronic diseases, including cancer, heart disease, and inflammatory bowel disease (IBD)
- Unhealthy lifestyle, such as smoking, obesity, and lack of physical activities
- Old age
Symptoms
The symptoms of venous embolism will depend on the type of venous embolism that occurs, be it DVT or pulmonary embolism.
Symptoms from DVT include:
- Swelling of the leg or arm
- Redness
- Warmer skin
- Leg or arm pain
Symptoms of pulmonary embolism may occur with or without symptoms of DVT. These symptoms include:
- Chest pain
- Shortness of breath
- Rapid pulse
- Rapid breathing
- Dizziness or headache
- Loss of consciousness
- Cold, sweaty hands
- Coughing up blood
Diagnosis
Other conditions may cause symptoms similar to a venous embolism. To establish a diagnosis, your doctor will need to know about your overall medical history. This is necessary to identify any risk factors for venous embolism that you may have.
Other diagnostic tests that can be done are:
- Oximetry. If you have symptoms of a pulmonary embolism, your doctor will immediately check your oxygen levels with oximetry. Oximetry can show the oxygen levels in the blood. Low oxygen levels may indicate lung or heart problems
- Blood test. Blood tests look for D-dimer, which is one of the indicators of blood clots. A high level of D-dimer in the blood indicates that blood is clotting. Blood tests can also show oxygen levels and any clotting disorders you might have
- Ultrasound. Ultrasound examination is a non-invasive procedure that looks directly at blood flow inside blood vessels. This examination allows the doctor to identify the presence of a blood clot
Management
Management and treatments for venous embolism may vary depending on the size of the blood clot. While oral medications can be used to treat DVT in some cases, a venous embolism must be removed and treated immediately. The doctor will use a catheter to remove the blood clot from a vein. They may also administer clot-busting medication. However, both of these actions may result in complications, such as bleeding. Therefore, the procedure needs to be done under close supervision.
If the condition is not life-threatening, the treatment will focus on preventing blood clots from growing larger and new blood clots from developing. Medications used to prevent this include blood thinners (anticoagulants) and compression stockings, which are special stockings that can help increase blood flow to the heart.
If you have had a venous embolism, you can do the following to prevent recurrence, among other things:
- Have regular check-ups. Your doctor will need to monitor your overall health and determine when you should stop treatment
- Take your medications as instructed. Even if you have no symptoms, you should take your medications on a regular basis. Inform your doctor if you experience side effects like bleeding gums, black stools, etc
- Check for signs of venous embolism, like shortness of breath and calf pain
- Change your lifestyle. Drink 7-8 glasses of water per day and quit smoking
Complications
Complications that can occur due to venous embolism include:
- Venous vessel damage or chronic vein insufficiency
- A blood clot enters an artery and causes arterial blockage in the brain (stroke)
- Renal vein thrombosis, which is blocked blood flow in the kidney
- Death
Prevention
Venous embolism can be caused by various factors, some of which cannot be controlled. However, the simplest preventive measure is to be active as frequently as possible. Because DVT most commonly occurs in the legs and feet, you can reduce your risk of developing a venous embolism by ensuring that your limbs have adequate blood flow.
If you are more sedentary or travel frequently, make sure you make time to walk every day. This activity helps your leg muscles pump blood to your heart.
If you have recently had surgery or have been sick for a long time, moving your legs even slightly can help prevent blood clots from forming.
When to See a Doctor?
If you have symptoms of a venous embolism, such as DVT or pulmonary embolism, see a doctor immediately. The symptoms you experience may not always be the cause, but prompt and appropriate treatment can prevent further complications. If you have risk factors for venous embolism, discuss it with your doctor.
Looking for more information about other diseases? Click here!
- dr Hanifa Rahma
Cleveland clinic. (2022). Venous Thromboembolism. Available from: https://my.clevelandclinic.org/health/diseases/22614-venous-thromboembolism
Griffin RM. (2020). Venous Thromboembolism (VTE). WebMD. Available from: https://www.webmd.com/dvt/what-is-venous-thromboembolism
National Heart, Lung, and Blood Institute (NIH). (2022). What is Venous Thromboembolism? Available from: https://www.nhlbi.nih.gov/health/venous-thromboembolism
Winter MP, Schernthaner GH, Lang IM. Chronic complications of venous thromboembolism. J Thromb Haemost. 2017 Aug;15(8):1531-1540. doi: 10.1111/jth.13741. PMID: 28762624.