Definisi
Benda asing di kornea merupakan trauma mata yang tersering kedua, selain terjadinya kerusakan pada permukaan kornea. Biasanya, benda asing di kornea ini sifatnya ringan dan tidak membahayakan penglihatan secara keseluruhan. Namun, kondisi ini dapat menimbulkan sensasi tidak nyaman yang akhirnya membawa pasien untuk berobat. Angka kejadiannya berbeda-beda tergantung populasi yang diamati, namun sebuah studi di Swedia menyatakan angka kejadiannya adalah 8 kejadian pada setiap 1.000 orang.
Penyebab
Kondisi ini disebabkan oleh berbagai macam keadaan, tetapi pada umumnya berupa kombinasi dari ketidakpatuhan menggunakan alat pelindung mata dan pekerjaan yang berisiko tinggi. Namun, benda asing di kornea dapat menempel pada saat-saat yang tidak terduga, misalnya pada saat berkendara dengan sepeda motor atau berjalan kaki. Benda-benda yang dapat menempel di kornea pun bermacam-macam, tergantung pekerjaan orang yang bersangkutan.
Faktor Risiko
Pekerjaan yang berisiko tinggi terhadap paparan benda asing di kornea adalah pekerjaan yang melibatkan mengasah logam atau kayu, memalu paku, mengebor (dapat mengebor aspal, logam, kayu, dan sejenisnya), serta mengelas logam. Biasanya, pada pekerjaan seperti ini, orang yang bersangkutan sedang tidak menggunakan alat pelindung mata dan partikel benda kecil seperti logam, kayu, atau aspal terpapar ke kornea. Berkaitan dengan pekerjaan yang mungkin menjadi faktor risiko, pria lebih sering terpapar dengan benda asing di kornea daripada wanita, terutama pria berusia di bawah 40 tahun.
Gejala
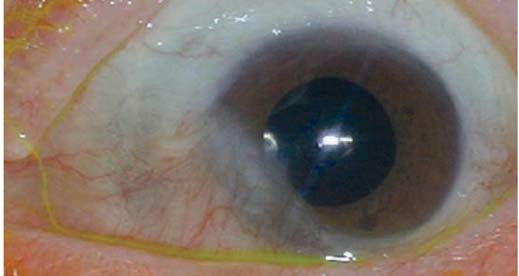
Jika terdapat benda asing di kornea, keluhan sensasi benda asing merupakan keluhan yang sering muncul sehingga membawa pasien ke dokter. Keluhan gangguan penglihatan bisa muncul, namun bisa pula tidak, tetapi yang sering muncul adalah sensitivitas terhadap cahaya. Selain itu, keluhan yang sering muncul adalah mata merah dan berair, terutama di dekat selaput pelangi pada mata. Benda asing dapat terlihat dengan jelas, namun dapat pula tidak. Keluhan nyeri juga sering muncul karena kornea memiliki ujung saraf nyeri yang aktif ketika terdapat benda asing.
Diagnosis
Sebelum melakukan pemeriksaan pada mata, dokter akan menanyakan kronologi kejadian untuk mengetahui kemungkinan benda yang menempel pada kornea, dan bagaimana hal tersebut terjadi. Setelah itu, dokter dapat melakukan pemeriksaan fungsi mata seperti tajam penglihatan dan refleks mata terhadap cahaya. Pemeriksaan kelopak mata bagian dalam juga dapat dilakukan untuk mengetahui jika ada benda asing lainnya yang menempel di sana.
Jika dicurigai adanya benda asing pada kornea, dokter biasanya akan memberikan zat pewarna pada mata untuk mengetahui bagian kornea yang terpapar serta memperjelas keberadaan dan posisi benda asing tersebut. Dokter juga dapat melakukan pemeriksaan bola mata bagian dalam menggunakan funduskopi atau slit lamp untuk menyingkirkan kemungkinan adanya benda asing yang tembus ke dalam bola mata.
Jika mata sudah sampai bernanah, dokter dapat melakukan pemeriksaan laboratorium untuk mengetahui adanya kemungkinan infeksi. Pemeriksaan laboratorium tersebut dapat berupa pemeriksaan darah lengkap, hitung jenis sel darah putih, serta kultur bakteri. Dokter juga dapat melakukan pencitraan seperti USG mata jika ada kecurigaan benda asing yang tembus ke dalam bola mata. Pilihan lainnya adalah pemeriksaan dengan sinar biru dan zat pewarna untuk mengeksklusi perforasi kornea (perlubangan pada kornea).
Tata Laksana
Sebelum dibawa ke dokter, terdapat beberapa hal yang perlu diperhatikan:
1. Jangan mengucek mata
Meskipun sensasi benda asing terasa sangat tidak nyaman, Anda sebaiknya tidak mengucek mata karena benda asing tersebut dapat menggores kornea. Sebaiknya, Anda juga tidak mengucek mata saat bekerja dengan kayu ataupun logam.
2. Jangan berusaha mengeluarkan benda asing sendiri
Kornea merupakan struktur yang sangat sensitif terhadap goresan, sehingga pengeluaran benda asing di kornea membutuhkan kewaspadaan tinggi. Oleh karena itu, benda asing hanya boleh dikeluarkan oleh dokter.
Sampai di dokter, Anda dapat diberikan obat-obatan. Obat yang diberikan dapat berupa anti nyeri, yang dapat dikonsumsi dengan diminum, lewat infus, atau diteteskan ke mata. Pemberian obat-obatan untuk melemaskan otot mata dapat pula menurunkan nyeri, serta penutup mata untuk mata yang tidak terkena. Mata yang tidak terkena mungkin akan perlu ditutup agar mata tidak menangkap cahaya berlebih, yang selanjutnya meringankan kerja otot penglihatan.
Benda asing di kornea akan diambil dalam waktu kurang dari 24 jam untuk mencegah tertanamnya benda asing tersebut di dalam kornea. Biasanya, prosedur ini langsung dilakukan oleh dokter mata. Pada prosedur ini, mata Anda akan dialiri dengan air bersih diikuti dengan penggunaan usap kapas lembab untuk mengambil benda asing tersebut. Jika tidak berhasil, dokter dapat menggunakan jarum untuk mengambil benda asing tersebut.
Setelah benda asing diambil, Anda akan diberikan beberapa obat. Obat anti nyeri akan diberikan karena biasanya nyeri masih akan ada hingga beberapa hari. Obat pelemas otot dapat pula diberikan, namun biasanya hanya beberapa hari saja. Antibiotik juga perlu diberikan untuk mencegah terjadinya infeksi pada kornea.
Selain pemberian obat, biasanya Anda akan diminta untuk kontrol setelah 24 jam, dilanjutkan dalam beberapa hari hingga 2 minggu. Kontrol ini bertujuan untuk memantau penyembuhan kornea, apakah terjadi secara sempurna atau memerlukan terapi lanjutan. Selain itu, kontrol juga bertujuan untuk memantau fungsi penglihatan serta adanya kemungkinan infeksi.
Komplikasi
Komplikasi yang dapat terjadi akibat benda asing di kornea bermacam-macam. Jika paparan terjadi dengan kecepatan tinggi atau Anda mengucek mata sebelum benda asing dikeluarkan, kornea dapat mengalami goresan yang disebut sebagai abrasi kornea. Jika benda asing tidak dikeluarkan dalam waktu 24 jam, benda asing tersebut dapat tertanam di kornea dan dapat mengganggu penglihatan, terutama jika benda asing tersebut terletak di bagian tengah kornea.
Selain itu, benda asing dapat menjadi sumber infeksi kornea (keratitis), yang perlu ditangani lebih lanjut menggunakan antibiotik. Perlubangan pada bola mata juga dapat terjadi terutama jika paparan benda asing terjadi dengan kecepatan tinggi, atau jika luka pada kornea tidak segera ditangani. Perlubangan ini hanya dapat ditangani dengan pembedahan.
Pencegahan
Masuknya benda asing di kornea dapat dicegah dengan menangani faktor risiko yang ada, seperti berikut:
- Gunakan kacamata pelindung saat bekerja. Faktor risiko tersering adalah ketidakpatuhan penggunaan alat pelindung diri saat bekerja dengan risiko tinggi paparan terhadap partikel-partikel kecil yang dapat menempel di kornea.
- Gunakan helm dengan penutup wajah saat berkendara dengan sepeda motor. Dengan penggunaan helm seperti ini, partikel debu atau daun tidak mudah mengenai kornea.
Kapan Harus ke Dokter?
Jika mata Anda tiba-tiba kemasukan benda asing, cobalah untuk melihat lokasi benda asing tersebut sendiri atau dengan bantuan orang lain. Jika benda asing tersebut terletak tepat di atas selaput pelangi atau pupil mata, segeralah ke dokter dalam 24 jam, agar benda asing tersebut dapat dikeluarkan sebelum tertanam di dalam kornea. Pada anak, biasanya keluhan yang terjadi adalah mata merah, berair, dan nyeri, dan biasanya terjadi setelah mengucek mata atau bermain. Sama seperti orang dewasa, jika benda asing terletak di atas selaput pelangi atau pupil mata, segeralah bawa anak Anda ke dokter.
Mau tahu lebih lanjut seputar penyakit-penyakit lainnya? Cek di sini, ya!
- dr Ayu Munawaroh, MKK
- dr Hanifa Rahma
Bashour, M. (2018). Corneal Foreign Body: Background, Pathophysiology, Epidemiology. Retrieved 24 October 2021, from https://emedicine.medscape.com/article/1195581-overview#showall.
Camodeca, A., & Anderson, E. (2021). Corneal Foreign Body. Retrieved 24 October 2021, from https://www.ncbi.nlm.nih.gov/books/NBK536977/.
Mendelsohn, A., Bunya, V., Pokeza, N., Murchison, A., & Syed, Z. (2021). Removal of Corneal Foreign Bodies - EyeWiki. Retrieved 24 October 2021, from https://eyewiki.org/Removal_of_Corneal_Foreign_Bodies.