Definition
The field of view refers to the total area that can be seen when the eyes are focused on a central point without moving the eyes or head. A normal visual field extends approximately 50 degrees upward, 60 degrees inward, 70 degrees downward, and 90 degrees outward. Visual field defects occur when there is a loss of vision in one or more areas within this range.
The process of seeing involves the eyes capturing light reflected from an object, converting it into a signal, and sending it to the brain via the optic nerves. The brain then interprets this signal as the image of the object. Any disruption in this process—whether in the eyes, brain, or nerves—can lead to visual field defects.
Causes
Visual field defects can result from various conditions, including:
- Glaucoma: Damage to the optic nerve due to disturbances in the eye fluid flow system (aqueous humor). This can increase intraocular pressure, lead to visual field loss.
- Optic Nerve Disorders: The optic nerve transmits visual signals from the eye to the brain. Any disorder affecting the optic nerve can impair the field of vision.
- Eye Tumors: Tumors can obstruct light from entering the eye, preventing the eye from sending visual signals to the brain.
- Ocular Blood Vessel Disorders: Ruptured or bleeding blood vessels in the eye can hinder its ability to capture light, leading to visual field impairment.
- Eye Infections: Conditions such as congenital toxoplasmosis (infection with Toxoplasma gondii acquired from the mother during pregnancy) can cause visual field defects.
- Age-Related Macular Degeneration: The macula, located at the center of the retina, is crucial for capturing light. Its function may decline with age, leading to vision loss.
- Autoimmune Diseases: Conditions like multiple sclerosis can damage nerves, including those involved in vision.
- Metabolic Diseases: Disorders such as hyperthyroidism can contribute to visual field defects.
- Stroke and Brain Disorders: Strokes and other brain conditions can disrupt the pathways responsible for processing visual information.
Risk Factor
Individuals with certain predispositions or conditions are at greater risk for developing visual field defects, especially if their underlying diseases are uncontrolled or inadequately managed.
Risk factors include family history of glaucoma, prolonged use of steroid anti-inflammatory drugs, individuals with a shallow anterior chamber, nearsightedness or farsightedness with large lens size, people over 40 years old, patients of chronic diseases (such as diabetes, hypertension, and cardiovascular problems have increased risks of glaucoma, in turn in increased risks of visual field defects.
In glaucoma patients, high intraocular pressure can also cause visual field defects.
The incidence of new cases of visual field defects increase fivefold between the ages of 55 to 80. Glaucoma is the most common cause, followed by stroke in individuals under 75, macular degeneration, and retinal artery occlusion.
Symptoms
Symptoms of visual field defects include:
- Difficulty in driving
- Frequent stumbling or tripping
- Blurred vision, making it hard to watch TV or read
- Blocked or darker areas in the visual field
- Inability to see from one side (either left or right)
Diagnosis
To diagnose visual field defects, the doctor will first conduct an interview to gather information on the patient’s symptoms and medical history. A physical examination will follow, along with diagnostic tests.
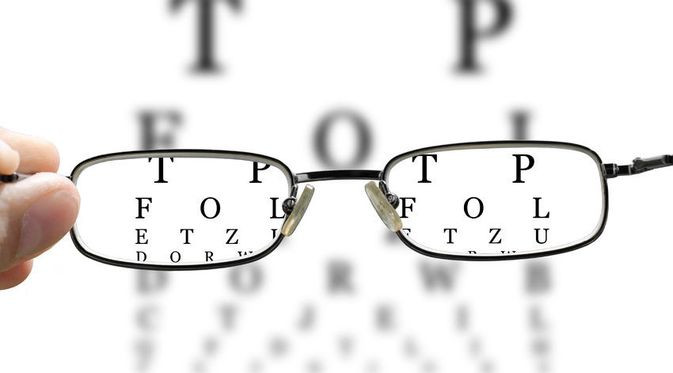
Visual field examinations assess the function of the brain, nerves, and eyes to pinpoint the cause of the visual field defects. Treatments will be given according to the suspected cause after the tests are conducted. Visual field tests can also be conducted without any devices, may include a confrontation test.
Confrontation test is a basic test where the patient and doctor, both closing one eye, focus on a central point while the doctor moves a finger in different directions. The patient indicates whether they can see the finger. This test requires the doctor to have normal eyes with no visual field defects.
If a visual field defect is suspected, further testing with specialized tools may be conducted, such as, Goldmann Perimeter, Tangent Screen, Amsler Grid and Computerized Automated Perimeter.
There are types of visual field defects, such as:
- Central/Peripheral: Visual field loss can occur centrally (due to central nervous system issues) or peripherally (related to peripheral nervous system problems).
- Scotoma: A condition characterized by a reduction in some parts of the visual field.
- Hemianopia: Loss of vision in one part of the visual field.
Management
Treatments for visual field defects are tailored to the underlying cause. For instance, if visual field defects are caused by glaucoma with elevated intraocular pressure, treatment will focus on reducing eye pressure. Early intervention can prevent the progression of visual field loss.
For eye tumors, surgery may be necessary, while stroke-related visual field defects are generally managed with stroke-specific medications.
In cases of degenerative retinal diseases, such as macular degeneration and diabetic retinopathy, laser therapy might be an option. However, retinal damage may not be fully reversible. Treatment for degenerative diseases typically targets the underlying risk factors.
Complications
Complications from visual field defects can affect both the eyes and other parts of the body, especially due to difficulties in daily activities. Patients may experience injuries from accidents, such as driving difficulty or frequent falls, leading to anything from minor injuries like muscle strains to severe, life-threatening injuries such as head trauma. The most severe ocular complication is permanent blindness.
Prevention
Preventing visual field defects involves addressing the underlying conditions that cause them. General preventive measures include maintaining a balanced diet, getting sufficient rest, and managing stress effectively. These practices are particularly important for those with risk factors for diseases that can cause visual field defects. Early detection of these conditions can prevent them from progressing to blindness.
For glaucoma prevention, regular eye screenings are crucial, especially for those with risk factors. Glaucoma can be detected early through routine screenings, which are recommended every 2-4 years for individuals under 40, every 2 years for those over 40, and annually for those with a family history of glaucoma.
For individuals already diagnosed with diseases that may cause visual field defects, routine eye exams are essential for early detection. Proper management and treatment following these screenings can prevent or slow the progression of visual field loss.
For instance, controlling intraocular pressure in glaucoma patients can prevent visual field defects, thereby improving quality of life.
Additionally, regular eye examinations can prevent optic nerve damage from medications like Ethambutol, used to treat tuberculosis, which may have side effects affecting vision.
When to See a Doctor?
If you have risk factors for visual field defects, it is advisable to consult an ophthalmologist for regular screenings. Early detection through routine exams can prevent the progression of visual field defects and avert permanent blindness.
Looking for more information about other diseases? Click here!
- dr Nadia Opmalina
Boyd, K. 2021. Visual field test. American Academy of Ophthalmology. Retrieved 21 November 2021, from https://www.aao.org/eye-health/tips-prevention/visual-field-testing
Knott, L. 2021. Visual field defects. Patient. Retrieved 21 November 2021, from https://patient.info/doctor/visual-field-defects
MedlinePlus. 2021. Visual field. MedlinePLus. Retrieved 21 November 2021, from https://medlineplus.gov/ency/article/003879.htm
Situasi Glaukoma di Indonesia. 2019. Jakarta: Kemenkes RI.