Definition
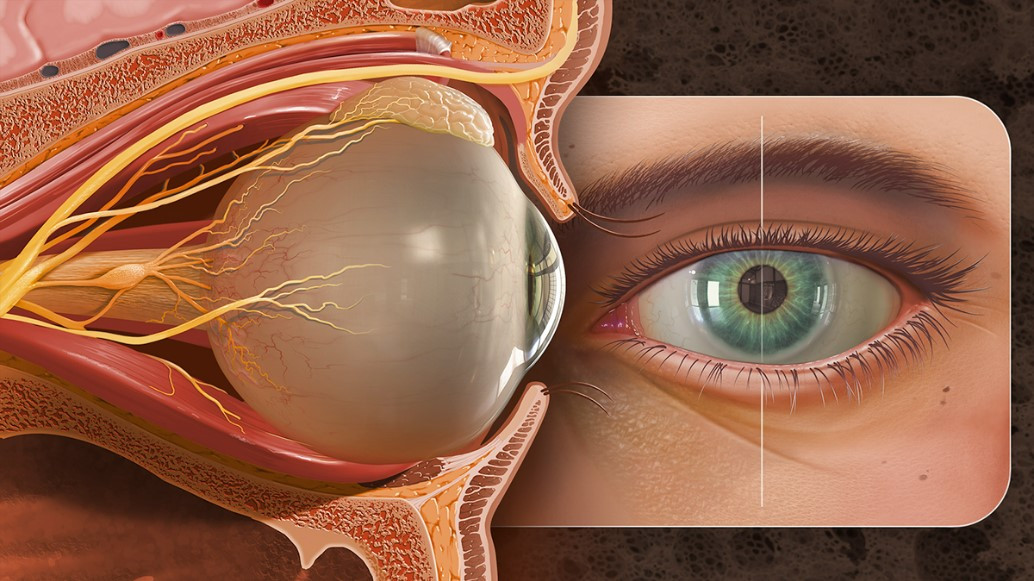
Eyelid malignancy refers to a malignant tumor developing on the eyelid skin. Among all skin malignancies, 5-10% occur on the eyelid. These tumors are classified based on their origin, with 90% being basal cell carcinomas, around 7% squamous cell carcinomas, approximately 3% sebaceous gland carcinomas, and less than 1% other malignancies.
Causes
Eyelid malignancies develop when cells lose the ability to control their division. This disruption usually occurs due to mutations or damage to the genes responsible for regulating cell growth. Such mutations can be triggered by various factors, including exposure to radiation (such as ultraviolet B rays from the sun), aging, smoking, contact with toxic substances, and viral infections. These genetic mutations can affect different types of body cells, including those in the skin. The cells most commonly involved in eyelid malignancies are basal cells, which are located in the skin’s outer layer. Basal cells play a crucial role in skin regeneration, as they divide to create new skin cells. In addition to basal cells, squamous cells, which are flat cells that form protective layers over various parts of the body, including the skin, are also often implicated in the development of eyelid malignancies. Furthermore, malignancies can arise from the sebaceous (oil) glands in the eyes.
Risk Factor
Several common risk factors contribute to the development of eyelid malignancies. These include advancing age, prolonged exposure to ultraviolet radiation from sunlight, smoking, frequent exposure to toxic chemicals, poorly healing scars, and a suppressed immune system. For example, people who have recently undergone organ transplants may experience immune suppression as part of their treatment regimen, which increases their risk. Viral infections, such as those caused by Human Papillomavirus (HPV) or Human Immunodeficiency Virus (HIV), can also elevate the risk of developing eyelid malignancies. Certain conditions increase the likelihood of skin cell mutations, such as xeroderma pigmentosum, a rare genetic disorder that causes extreme sensitivity to sunlight. Another condition is actinic keratosis, which leads to dry, cracked, and scaly skin due to prolonged sun exposure. Albinism is another risk factor because people with this condition lack melanin, the pigment that helps protect skin cells from the harmful effects of UV radiation. Those with lighter skin are at a higher risk of developing eyelid malignancies compared to individuals with darker skin.
Symptoms
The symptoms of eyelid malignancy commonly include lumps on the eyelids that are prone to bleeding, non-healing sores, scaly skin, pain or numbness in the affected skin area, and the loss of eyelashes (known as madarosis). The lumps or lesions may spread rapidly. They are more frequently found on the lower eyelids, as these are more exposed to sunlight. In cases of malignancy originating from the oil glands, the skin of the eyelid may become thickened and take on a yellowish appearance. Additional symptoms can include persistent swelling of the eyelids, which may be accompanied by inflammation of the conjunctiva (the thin membrane that covers the white part of the eye) and the inner eyelid.
Diagnosis
The diagnosis of eyelid malignancy involves an eye examination assessing eyelid and eyeball movement to detect the spread of malignancy into the orbital cavity. The external eye is inspected for eyelash loss (madarosis) and surface blood vessel dilation (telangiectasis). The eyelid is everted to check for conjunctival spread, and lymph nodes are examined to determine the malignancy's extent.
The primary diagnostic tool is a biopsy, where a sample of tissue is removed from the suspected malignant area of the eyelid. Biopsy of the eyelid skin tissue is the gold standard for confirming malignancy, as it allows for microscopic examination of the malignant cells. An immunohistochemical examination may also be conducted to identify cell types within the malignancy, influencing treatment decisions.
The tumor size, spread to surrounding tissues and lymph nodes, and biopsy results are used to stage the malignancy. This staging informs therapy choices and provides an estimate of recovery and recurrence.
Management
The primary goal in managing eyelid malignancy is to control the proliferation of abnormal cells to prevent spread to adjacent tissues. The treatment approach depends significantly on the type of malignancy, though it generally involves medication or surgery. In basal cell carcinoma, topical medications may be employed to eradicate the tumor, although surgery is often more effective. Surgical procedures aim to excise the tumor completely. For sebaceous carcinoma, surgical removal of the tumor tissue is the main therapeutic approach.
Squamous cell carcinoma therapy is more varied. Cryotherapy, which uses liquid nitrogen to freeze tumor cells, can be an option for less aggressive malignancies. Photodynamic therapy, involving drugs that make the tumor cells more light-sensitive followed by light exposure to destroy them, can be another alternative. Radiation therapy is an option for patients at high surgical risk. Surgical intervention can include skin grafts to promote normal skin growth in the affected area. Topical medications may be prescribed in some cases. If the malignancy has metastasized, chemotherapy, which uses systemic drugs, remains the primary treatment option.
Complications
All eyelid malignancies carry a risk of recurrence. The larger the initial tumor size and the greater the malignancy's spread, the worse the prognosis and higher the recurrence risk. In advanced stages, sebaceous carcinoma can be fatal. Conversely, basal cell carcinoma and squamous cell carcinoma have more predictable outcomes.
Prevention
Preventive measures for eyelid malignancy include using skin protection during outdoor activities, such as sunglasses or sunscreen on the eyelids. Avoiding smoking and alcohol consumption can also reduce the risk of malignancy.
When to See a Doctor?
Seek medical advice if you notice a persistent lump, swelling, or stye on your eye. Immediate consultation is recommended if the lump bleeds easily or is accompanied by symptoms such as red eyes, drooping eyelids, and difficulty moving the eyeballs.
Looking for more information about other diseases? Click here!
- dr Hanifa Rahma
de Freitas, A., Marcet, M., Frasson, P., Kozak, A., Burkat, C., & Sundar, G. (2021). Squamous Carcinoma of the Eyelid - EyeWiki. Retrieved 22 November 2021, from https://eyewiki.aao.org/Squamous_Carcinoma_of_the_Eyelid
Marcet, M., Phelps, P., Plumb, R., Kozak, A., Goel, S., & Stewart, K. (2021). Basal Cell Carcinoma - EyeWiki. Retrieved 22 November 2021, from https://eyewiki.aao.org/Basal_Cell_Carcinoma
Silverstein, E., Marcet, M., Phelps, P., Yen, M., Silkiss, R., & Burkat, C. (2021). Sebaceous Carcinoma - EyeWiki. Retrieved 22 November 2021, from https://eyewiki.aao.org/Sebaceous_Carcinoma