Definisi
Selulitis orbita adalah infeksi serius pada jaringan lemak dan otot mata yang terletak di belakang septum orbita. Septum orbita adalah membran tipis yang memisahkan kelopak mata dengan rongga mata. Berdasarkan letak organ yang terinfeksi, selulitis orbita juga sering disebut dengan selulitis post-septum.
Selulitis orbita adalah infeksi berbahaya dan dapat menyebabkan masalah yang berkepanjangan. Selulitis orbita dapat mengenai salah satu atau kedua mata. Gejalanya dapat muncul tiba-tiba atau akibat penyakit infeksi mata lain yang meluas ke jaringan sekitar mata. Semua usia dapat mengalami selulitis orbita. Namun, penyakit ini lebih sering ditemukan pada kelompok anak. Jika tidak ditangani dengan tepat, dapat mengakibatkan kebutaan.
Penyebab
Hampir 98% kasus selulitis orbita diawali oleh infeksi rongga sinus (sinusitis) yang tidak diobati dan menyebar ke area belakang septum orbita. Kuman penyebab infeksi ini dapat berupa bakteri normal kulit atau bakteri lain. Dahulu, penyebab terseringnya adalah sinusitis oleh bakteri Haemophilus influenza. Infeksi ini sering ditemukan pada anak kecil di bawah usia 7 tahun. Namun, sekarang sudah jarang terjadi karena adanya vaksin HiB yang membantu mencegah infeksi bakteri tersebut.
Bakteri yang masih sering ditemukan adalah Staphylococcus aureus, Streptococcus pneumoniae, dan Streptokokus beta-hemolitikus. Pada anak <9 tahun, biasanya disebabkan oleh satu bakteri. Sementara pada anak >9 tahun dan orang dewasa, dapat disebabkan oleh beberapa jenis bakteri sekaligus, sehingga lebih sulit diobati. Pada kasus yang lebih jarang, dapat disebabkan oleh bakteri aerob, anaerob, atau bahkan jamur. Pada orang dengan sistem imun yang rendah seperti pasien HIV/AIDS, diabetes, atau yang mengkonsumsi obat-obat sistem imun tertentu, kuman jamur dapat dipikirkan sebagai penyebab selulitis orbita. Pikirkan infeksi bakteri Gonorrhoea dan Chlamydia sebagai penyebab pada bayi baru lahir.
Penyakit ini juga berhubungan dengan penyebaran infeksi dari gigi atau infeksi bakteri pada area tubuh lainnya yang menyebar melalui pembuluh darah. Luka atau gigitan serangga di sekitar mata juga dapat menjadi penyebab selulitis orbita.
Infeksi selulitis orbita pada anak-anak dapat memburuk dengan sangat cepat dan dapat menyebabkan kebutaan. Terapi medis diperlukan segera pada kasus ini.
Faktor Risiko
Beberapa kondisi dapat meningkatkan risiko terjadinya selulitis orbita sebagai berikut:
- Infeksi saluran napas atas, termasuk sinusitis
- Infeksi pada gigi, telinga tengah, atau wajah
- Dakriosistitis, yaitu infeksi pada kelenjar air mata
- Cedera mata dengan patah tulang atau serpihan benda asing
- Tindakan operasi mata
- Pembiusan di sekitar bola mata
- Imunodefiensi (sistem imun rendah), misal pada pasien HIV/AIDS atau diabetes
Gejala
Gejala pada selulitis orbita meliputi:
- Pembengkakan yang nyeri pada kelopak mata, alis, atau pipi
- Kemerahan pada mata
- Sulit membuka mata
- Nyeri saat menggerakkan mata
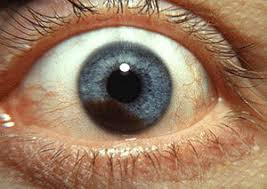
- Mata menonjol
- Penglihatan ganda
- Pergerakan mata terganggu
- Penglihatan menurun hingga kehilangan penglihatan
- Demam, biasanya >38.8'C atau lebih
- Lemas
- Nyeri kepala
Diagnosis
Diagnosis ditegakkan melalui wawancara mengenai gejala yang timbul, pemeriksaan fisik, hingga pemeriksaan penunjang. Untuk mengetahui apakah Anda menderita selulitis, dokter akan menanyakan apakah Anda baru saja menjalani operasi atau perawatan gigi. Dokter juga akan menanyakan apakah Anda baru saja mengalami luka pada wajah, kulit, atau sinusitis.
Dokter juga akan memeriksa mata Anda melalui pemeriksaan:
- Gerak mata termasuk adanya nyeri pada pergerakan mata
- Ketajaman penglihatan dan penglihatan warna. Jika mengalami penurunan, curiga ada gangguan pada saraf mata
- Kondisi proptosis (yaitu penonjolan mata ke depan)
- Lapang pandang melalui tes konfrontasi
- Refleks pupil. Jika mengalami gangguan, curiga ada gangguan saraf mata
- Tekanan bola mata. Jika mengalami peningkatan, curiga ada sumbatan pada pembuluh vena mata
- Biomikroskopi slit-lamp untuk memeriksa kondisi segmen depan bola mata
- Oftalmoskopi untuk memeriksa kondisi retina dan saraf mata
Pemeriksaan penunjang dipilih pada pemeriksaan pasien anak atau kasus yang tidak berespon baik terhadap terapi antibiotik dengan gejala yang memberat. Pemeriksaan penunjang juga dapat mendeteksi komplikasi lebih awal. Pemeriksaan penunjang yang mungkin dilakukan antara lain:
- Cek darah tepi lengkap, akan tampak peningkatan sel darah putih (tanda infeksi bakteri)
- Kultur darah untuk mengetahui jenis kuman penyebab
- Kultur cairan mata, telinga, atau tenggorokan
- Pungsi lumbal pada anak dengan kondisi para
- X-ray sinus dan area sekitarnya
- CT scan sinus, mata, atau kepala. CT scan dapat membedakan selulitis orbita dengan selulitis preseptal dan mendeteksi komplikasi lebih awal
- MRI sinus, mata, atau kepala. MRI dapat melihat jaringan lunak dengan baik
Tata Laksana
Pada kebanyakan kasus, diperlukan rawat inap di rumah sakit. Pada kasus ringan hingga sedang tanpa ada komplikasi pada saraf mata, terapi awal yang diberikan adalah antibiotik dan obat-obatan suportif melalui jalur pembuluh darah. Pembedahan mungkin diperlukan untuk mengeluarkan nanah yang terbentuk karena infeksi atau mengurangi tekanan di ruang sekitar mata. Infeksi selulitis orbita dapat memburuk dengan sangat cepat. Oleh karena itu, pasien dengan kondisi ini harus diperiksa setiap beberapa jam. Dengan pengobatan segera, pasien selulitis orbita dapat pulih sepenuhnya.
Dokter mata dan dokter THT akan bekerja sama untuk menentukan terapi yang tepat. Dalam beberapa kasus, operasi mungkin diperlukan, terutama pada pasien dengan infeksi yang meluas ke otak. Pasien lain yang memerlukan operasi adalah pasien yang tidak berespon dengan terapi antibiotik, adanya keterlibatan saraf mata ditandai dengan perburukan penglihatan atau perubahan pupil, abses (kumpulan nanah) yang besar dengan diameter >10 mm, penurunan kondisi klinis, atau komplikasi abses berulang. Tindakan operasi akan membantu menghentikan proses infeksi dengan mengalirkan cairan infeksi dari organ yang terinfeksi seperti sinus atau gigi. Tanpa diagnosis dan terapi yang tepat, infeksi dapat meluas ke jaringan lain dan menyebabkan komplikasi yang serius.
Dalam perawatan di rumah sakit, pasien harus dipantau apakah terdapat perburukan ke arah komplikasi infeksi otak yang dapat mengancam nyawa. Jika kondisi telah membaik dalam 48 jam pasca pemberian antibiotik infus, terapi akan diganti dengan antibiotik oral. Obati juga penyakit penyerta seperti sinusitis. Dengan pengobatan yang cepat dan tepat, selulitits orbita dapat disembuhkan.
Komplikasi
Komplikasi dari selulitis orbita antara lain:
- Kerusakan pada kornea
- Glaukoma
- Uveitis atau retinitis
- Ablasi retina (retina terlepas dari tempat penempelannya)
- Panoftalmitis (infeksi meluas pada bola mata dan seluruh jaringannya)
- Penyumbatan pembuluh darah retina
- Abses (kumpulan nanah) pada pembungkus tulang, bola mata, atau otak
- Kehilangan pendengaran
- Septikemia, yaitu infeksi meluas di dalam darah
- Meningitis, yaitu peradangan pada lapisan pembungkus otak
- Penurunan ketajaman penglihatan
- Trombosis sinus kavernosus, yaitu pembentukan bekuan darah di rongga dasar otak. Dapat mengancam penglihatan
- Kerusakan saraf optik dan kehilangan penglihatan (11% kasus)
- Infeksi pada otak
- Kerusakan saraf otak
Pencegahan
Pemberian vaksin HiB dapat mencegah infeksi ini pada sebagian besar anak. Anak-anak yang memiliki anggota keluarga serumah sedang mengalami infeksi ini, mungkin memerlukan konsumsi antibiotik untuk pencegahan. Dengan catatan, pemberian antibiotik harus sesuai saran dokter. Penanganan yang cepat pada infeksi sinus atau gigi dapat mencegah penyebaran infeksi menjadi selulitis orbita.
Jika Anda pernah mengalami selulitis orbita tidak berarti Anda pasti akan mengalaminya lagi. Namun, jika Anda rentan mengalami sinusitis berulang, Anda harus lebih menjaga kesehatan dan segera berobat jika mengalami gejala sinusitis agar mencegah penyebaran infeksi dan kekambuhan di kemudian hari. Hal ini penting dilakukan terutama bagi orang dengan sistem imun yang rendah.
Kapan Harus ke Dokter?
Selulitis orbita adalah kondisi darurat medis yang perlu segera diobati karena infeksi dapat menyebar dengan cepat. Segera konsultasi dengan dokter jika Anda mengalami sinusitis atau salah satu gejala selulitis orbita di atas.
Ingin tahu informasi seputar penyakit lainnya? Anda bisa mengunjungi tautan ini ya!
- dr Ayu Munawaroh, MKK
Vyas JM. 2020. Orbital cellulitis. MedlinePlus. Retrieved 22 November 2021, from https://medlineplus.gov/ency/article/001012.htm.
Danishyar A, Sergent SR. 2021. Orbital cellulitis. StatPearls Publisihing LLC. Retrieved 22 November 2021, from https://www.ncbi.nlm.nih.gov/books/NBK507901/
Whelan C. 2019. What to know about orbital cellulitis. Healthline. Retrieved 22 November 2021, from https://www.healthline.com/health/orbital-cellulitis
Yen MT. 2021. Orbital cellulitis. EyeWiki. Retrieved 22 November 2021, from https://eyewiki.aao.org/Orbital_Cellulitis
Boyd K. 2019. Cellulitis. American Academy of Ophthalmology. Retrieved 22 November 2021, from https://www.aao.org/eye-health/diseases/what-is-cellulitis
Gappy C, Archer SM. 2021. Orbital cellulitis. UpToDate. Retrieved form 22 November 2021, from https://www.uptodate.com/contents/orbital-cellulitis#H459379483
Periorbital and orbital cellulitis. 2019. The Royal Children’s Hospital Melbourne. Retrieved 26 November 2021, from https://www.rch.org.au/clinicalguide/guideline_index/Periorbital_and_orbital_cellulitis/
Balu I, Melendez E. 2020. Periorbital and orbital cellulitis. American Medical Association, 323(2).