Definition
Cutaneous tuberculosis (TB) can manifest as lupus vulgaris. This kind of cutaneous tuberculosis manifests in 1–2% of total tuberculosis cases. Cutaneous TB can present various symptoms based on the individual's immunological response. Lupus vulgaris has a prevalent appearance among the symptoms of cutaneous TB. Approximately 60% of people with cutaneous TB in Europe develop lupus vulgaris.
Causes
Lupus vulgaris is caused by a bacterium called Mycobacterium tuberculosis. This bacterium mostly targets the lungs but can possibly spread to other organs. TB infection can spread to several organs, including bones, lymph nodes, scrotum, skin, and brain. The virus can be transmitted through respiratory droplets released during breathing, coughing, or sneezing. Not all individuals exposed to the TB bacterium will manifest symptoms. Cutaneous tuberculosis can occur in the following ways:
- Inoculation of bacteria into the skin or direct entry of microorganisms through an open wound leads to exposure to germs and triggers an immunological response in the body
- Spread of infection to the skin via blood vessels
- Bacterial transmission to the skin occurs from other affected areas of the body, such as lymph nodes.
Lupus vulgaris can develop via the spread of germs to the skin via blood vessels or from the transfer of infection to the skin from other affected body organs.
Risk Factors
Risk factors for lupus vulgaris are immunodeficiency that could be caused by:
- Medical conditions, for example, HIV/AIDS infection
- Usage of medicine that could weaken the body’s immune system (e.g., in patients following organ transplants)
- Congenital defects
Various diseases that weaken the immune system in individuals infected with Mycobacterium tuberculosis might accelerate the growth and spread of the bacteria to different regions of the body, including the skin. Individuals previously infected with TB and treated successfully may develop lupus vulgaris if they develop immunodeficiency.
Symptoms
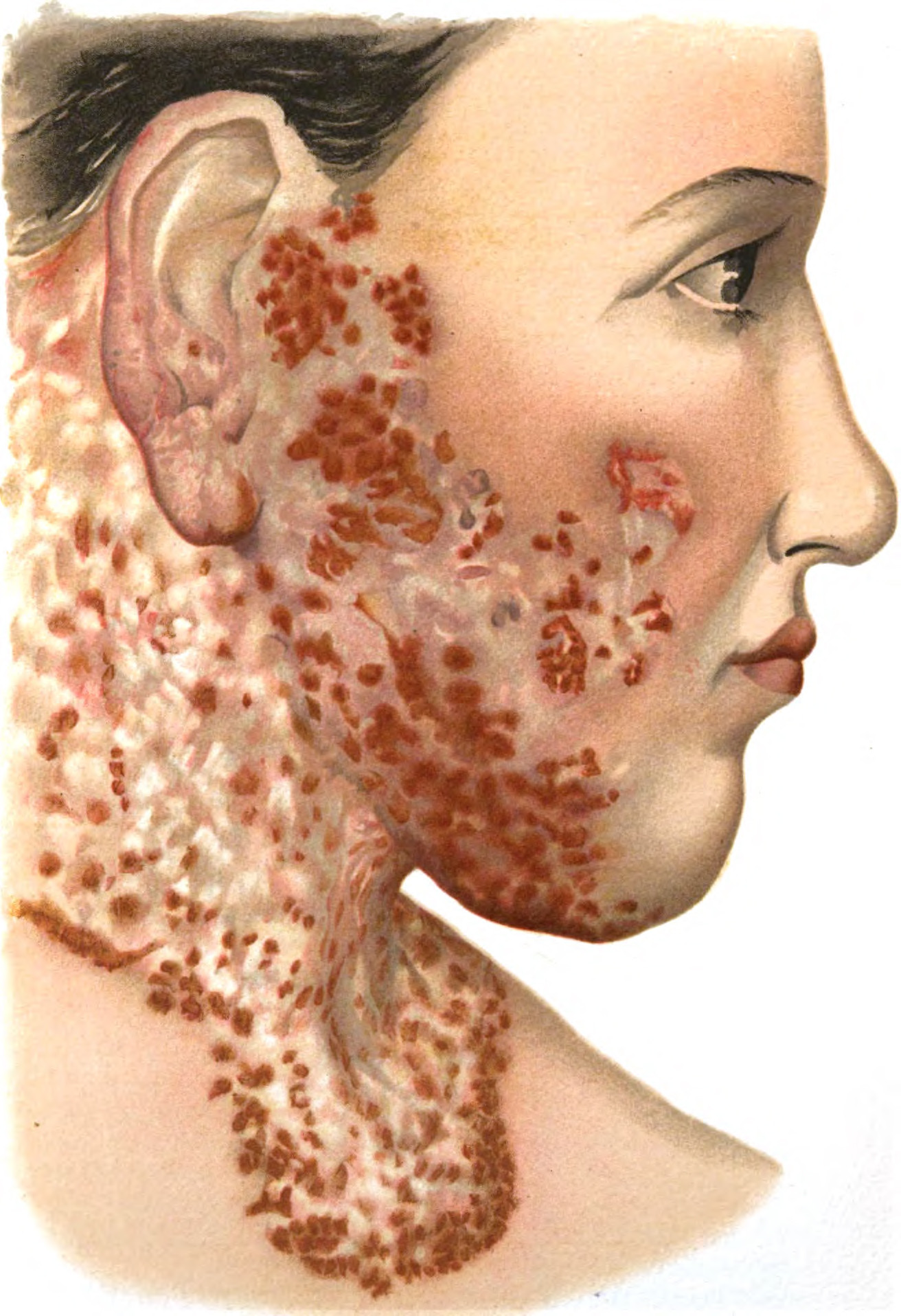
Lupus vulgaris is a chronic form of cutaneous TB that may worsen or spread. Lupus vulgaris can manifest on the skin of any body part, with the head and neck being the most often affected areas. Signs of lupus vulgaris may manifest as numerous tiny red-brown bumps that might coalesce to create plaques. These plaques have a soft texture, making them commonly known as apple jelly nodules. These symptoms may persist for an extended period, resulting in skin abnormalities and potentially skin cancer.
Diagnosis
Medical Interviews
Doctors can establish the diagnosis of lupus vulgaris by thoroughly evaluating the patient's medical history, symptoms, and physical examinations. Conditions such as HIV/AIDS, uncontrolled diabetes, cancer, and end-stage renal failure can cause immunodeficiency in individuals with lupus vulgaris. Patients may have a history of intravenous drug use or immunosuppressive medications.
Patients with lupus vulgaris may exhibit symptoms similar to those of tuberculosis, including:
- Chronic, productive cough lasting more than 2 weeks or hemoptysis
- Fever
- Excessive night sweats
- Weight loss
- Chest discomfort
- Tiredness
- Patients may report red-brown skin lesions that do not subside
Diagnostic Tests
Available tests for helping in establishing the diagnosis of lupus vulgaris include the tuberculin or Mantoux test, the AFB (Acid-Fast Bacillus) test, and a skin biopsy. Another diagnostic test that can be performed is a chest x-ray to detect the presence of a bacterial infection in the lungs.
The tuberculin or Mantoux test involves injecting proteins from the tuberculosis bacteria into the skin to observe the body's immune response to these proteins. This protein is not infectious for tuberculosis.
The AFB test detects the presence of bacteria in samples. The technique is named after the rod-shaped (bacillus) and acid-resistant characteristics of Mycobacterium tuberculosis. If an individual with lupus vulgaris experiences a productive cough, samples for this evaluation can be obtained from sputum. Next, the sputum will be examined using a microscope. Sputum samples can be tested again in a rapid molecular test to determine the susceptibility of tuberculosis germs to routinely prescribed antibiotics for TB.
A skin biopsy involves removing a skin tissue sample. Lupus vulgaris is characterized by the formation of nodules on skin tissue. Subsequently, the skin tissue sample will be examined using a microscope. This skin tissue can also be used for other tests, such as:
- AFB (Acid-Fast Bacillus) or Acid-Fast Stains Test
- Bacteria culture to see the growth of Mycobacterium tuberculosis
- Bacteria culture is a gold standard examination for cutaneous tuberculosis; this procedure could also be requested to detect bacterial resistance to certain antibiotics
Management
The treatment for lupus vulgaris is the same as the treatment for other types of TB. This treatment entails the simultaneous use of multiple antibiotics. Commonly used antibiotics include rifampicin, isoniazid, pyrazinamide, and ethambutol. Intravenous streptomycin may be used on occasion. If the rapid molecular test or bacterial culture indicates that the bacteria are resistant to specific antibiotics, the doctor may prescribe alternative medications.
Antibiotic treatment consists of two phases:
1. Intensive phase
During this phase, the goal is to rapidly reduce the levels of Mycobacterium tuberculosis bacteria in the body. The typical medications prescribed include rifampicin, isoniazid, pyrazinamide, ethambutol, and occasionally streptomycin. The medications are consumed daily for two consecutive months.
2. Continuation phase
During the continuation phase of therapy, the goal is to totally eliminate the germs from the body after two months of treatment. The typical medications prescribed include rifampicin and isoniazid. Patients can take the medications daily or three times a week for a duration of 4 months. The duration of the follow-up period may extend to 9–12 months, contingent upon how many bacteria are present in the body.
Patients must adhere to the doctor's prescribed medication schedule to treat lupus vulgaris. This necessitates a high level of dedication and adherence from the patients. Hence, the individual nearest to the patient might collaborate with healthcare providers to oversee the patients' medication intake. They will supervise patients to ensure they are taking proper medication, correct dosage, timely intake, and preventing regurgitation.
These medications may cause adverse effects, ranging from moderate ones like crimson urine and nausea to serious ones like hepatitis, allergies, and neurological problems. If you have any negative effects, you should seek advice from your doctor about taking these medications.
Complications
Lupus vulgaris can lead to irreversible skin abnormalities. Approximately 10% of individuals with lupus vulgaris are susceptible to acquiring squamous cell carcinoma skin cancer, often 25–30 years following the onset of lupus vulgaris.
Prevention
Preventing lupus vulgaris involves:
1. BCG (Bacillus Calmette-Guerrin) Vaccination
This vaccination can be given to newborns up to 2 months old. This vaccination aims to inject weakened TB bacteria under the skin so that the body's immune response will train itself to fight these bacteria. This vaccination is not effective if given to children over 2 months of age.
2. Tuberculosis screening
Screening for TB symptoms can aid in identifying, isolating, and treating TB patients. Screening could reduce the spread of the disease, especially for those with compromised immune systems.
3. Treating individuals with compromised immune systems
Individuals with HIV/AIDS or diabetes require consistent medical care to maintain an adequate immune system capable of combating bacterial infections. Effective management of blood glucose levels is crucial for diabetic patients to reduce the risk of infections like lupus vulgaris. If you are taking immunosuppressive medications, your doctor can prevent TB, including lupus vulgaris, by prescribing antibiotics.
When to See a Doctor?
If you see that your skin bumps are increasing in size, it is advisable to seek medical advice promptly. Skin bumps may be benign tumors, malignancies, or lupus vulgaris, particularly if your immune system is compromised. If you have persistent non-healing wounds, it is advisable to seek medical advice to identify the underlying reason and receive appropriate treatment.
Looking for more information about other diseases? Click here!
- dr. Alvidiani Agustina Damanik
Charifa, A., Mangat, R., & Oakley, A. (2021). Cutaneous Tuberculosis. Ncbi.nlm.nih.gov. Retrieved 7 June 2022, from https://www.ncbi.nlm.nih.gov/books/NBK482220/.
Granado, J., & Catarino, A. (2020). Cutaneous tuberculosis presenting as lupus vulgaris. International Journal Of Infectious Diseases, 96, 139-140. Available from: https://doi.org/10.1016/j.ijid.2020.03.069.
Ngan, V., & Oakley, A. (2021). Cutaneous tuberculosis (TB) | DermNet NZ. Dermnetnz.org. Retrieved 7 June 2022, from https://dermnetnz.org/topics/cutaneous-tuberculosis.