Definition
Rheumatic fever is an acute condition that can cause inflammation or swelling in the heart, joints, brain, and skin. It is a rare complication that occurs after a bacterial infection in the throat. While rheumatic fever most often affects children, it can also occur in teens and adults. Most patients can be completely cured, but the disease can recur.
Causes
Rheumatic fever is a rare disease that can develop if strep throat or scarlet fever infections are not properly treated. It can also occur after skin infections caused by bacteria such as impetigo, though this is less common. Initially, these bacterial infections are caused by Streptococcus group A bacteria.
Not everyone who experiences bacterial infections will develop rheumatic fever. Interestingly, this condition is not directly caused by the bacteria themselves. Instead, the immune system becomes activated in response to the bacteria invading the body, but at some point, it also begins to attack healthy body tissues.
Therefore, it's important to understand that rheumatic fever arises not from the bacterial infection directly, but from an abnormal immune response. The exact reason why the immune system malfunctions in this way is not precisely known, but it results in inflammation (swelling). In rheumatic fever, inflammation primarily affects the heart, joints, skin, and central nervous system. It typically takes about 1-5 weeks after a bacterial infection for rheumatic fever to develop.
Prompt treatment of bacterial infections with antibiotics, as prescribed by a doctor, can significantly reduce the likelihood of developing rheumatic fever.
Risk factor
Anyone exposed to bacterial infections like strep throat or scarlet fever is at risk of developing rheumatic fever. Several factors can increase this risk:
- Age: Rheumatic fever is more common among school-age children (5-15 years old). It's very rare in children under 3 years old and adults.
- Group settings: Bacterial infections, especially Streptococcus group A, tend to spread in places where people gather in groups. If not properly managed, crowded conditions can trigger an abnormal immune response, leading to rheumatic fever. Such settings include schools, daycare centers, or military training facilities.
- Other health factors: Individuals who have previously had rheumatic fever are more prone to recurrent episodes later in life. Additionally, repeated infections with Streptococcus group A bacteria can heighten the risk of rheumatic fever.
- Genetic factors: Some individuals have genetic predispositions that increase susceptibility to rheumatic fever when infected with Streptococcus group A. Instances of rheumatic fever occurring in family members or twins support this notion.
- Environmental factors: Crowded conditions, poor sanitation, low socioeconomic status, and others can facilitate the easy spread of Streptococcus bacteria among many people, elevating the risk of rheumatic fever.
Symptoms
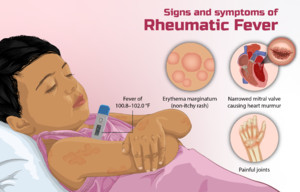
The symptoms of rheumatic fever result from inflammation affecting the heart, joints, skin, or central nervous system. Typically, rheumatic fever manifests within a few weeks, usually around 1-5 weeks after bacterial infection. These symptoms may evolve as the disease progresses.
Common symptoms of rheumatic fever include:
- Fever
- Fatigue
- Joint pain, which may migrate from one joint to another
- Redness or swelling in the joints, often affecting the knees, ankles, elbows, and wrists
- Involuntary, jerky movements of the body, particularly in the hands, feet, and face
- Painless, pale red rash on the arms or abdomen
- Small lumps under the skin, usually near the joints
Additionally, individuals with rheumatic fever may experience:
- Chest pain
- Shortness of breath
- Rapid heartbeat
- New abnormal heart murmurs
- Enlargement of the heart
- Fluid buildup around the heart
Diagnosis
The diagnosis of the disease is established through a medical interview, physical examination, and diagnostic tests if necessary. The doctor may inquire about the patient's complaints, medical history, and previous treatments. The patient's vital signs and body will be thoroughly examined to identify possible diseases causing the patient's condition.
If rheumatic fever is suspected, the doctor may recommend the following tests:
- Blood tests to look for signs of inflammation in the blood, or the presence of Streptococcus group A bacteria antibodies in the body.
- A throat swab was used to determine the possibility of Streptococcus group A bacterial infection.
- An electrocardiogram (EKG) or heart recording to determine the heart's electrical activity.
- Echocardiography is a test that provides images of blood flow in the heart and heart valves.
Management
The primary goals of treating rheumatic fever are eradicating the underlying Streptococcus group A bacterial infection, alleviating patient symptoms, managing inflammation, and preventing disease recurrence.
Treatment typically involves a combination of medications, including antipyretics (to reduce fever), pain relievers, anti-inflammatory drugs, and antibiotics. Initially, antibiotics are prescribed to target the Streptococcus group A bacterial infection. Following this, patients may receive prophylactic antibiotic therapy every 3-4 weeks for an extended period, often years, to prevent recurrence and disease exacerbation.
In cases where patients experience involuntary jerking movements and uncontrolled body movements, anticonvulsant medications may be prescribed.
For individuals with rheumatic heart disease, characterized by permanent heart valve damage resulting from rheumatic fever, symptomatic management may include heart medications to alleviate symptoms of heart failure until surgical intervention can be undertaken.
Complications
In some individuals, inflammation caused by rheumatic fever can lead to long-term complications. One such complication is permanent damage to the heart, known as rheumatic heart disease. Rheumatic heart disease typically occurs several years or decades after the initial illness.
Rheumatic heart disease can damage heart valves, and in severe cases, patients may require surgery to treat their condition.
Rheumatic fever can cause heart damage such as:
- Valve narrowing can reduce blood flow in the heart because blood has difficulty passing through the valve.
- Valve regurgitation: This condition causes some blood to flow back into the heart chamber instead of passing through the valve.
- Damage to the heart muscle, can affect the heart muscle's ability to pump blood.
- Irregular heartbeats.
- Heart failure in later stages.
Prevention
Having previously experienced a Streptococcus group A bacterial infection does not confer immunity against future recurrences of the infection. Maintaining personal hygiene practices, such as regular handwashing, can help prevent the spread of infection. Additionally, if you or your child experience persistent throat discomfort that does not improve after several days, it is advisable to consult a doctor. This consultation can help determine whether the symptoms indicate an infection or another condition.
To prevent rheumatic fever, treating Streptococcus group A bacterial infections with antibiotics until fully cured is crucial. The doctor will determine the duration of preventive antibiotic therapy based on individual circumstances.
When to see a doctor?
If any of the following signs or symptoms are present, please schedule an appointment with your child's doctor:
- Sudden throat pain
- Difficulty or pain when swallowing
- Fever
- Headache
- Abdominal pain
- Nausea or vomiting
Looking for more information about other diseases? Click here!
- dr. Yuliana Inosensia
Rheumatic fever: All you need to know (2022) Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/groupastrep/diseases-public/rheumatic-fever.html (Accessed: March 8, 2023).
Rheumatic fever (2022) Mayo Clinic. Mayo Foundation for Medical Education and Research. Available at: https://www.mayoclinic.org/diseases-conditions/rheumatic-fever/symptoms-causes/syc-20354588 (Accessed: March 8, 2023).
Rheumatic fever (2021) NHS choices. NHS. Available at: https://www.nhs.uk/conditions/rheumatic-fever/ (Accessed: March 8, 2023).