Definisi
Pembuluh balik (vena) adalah pembuluh darah yang membawa darah miskin oksigen dari seluruh tubuh untuk kembali ke jantung. Pembuluh balik ada yang terletak dekat dengan permukaan kulit dan ada yang jauh di dalam otot. Pembuluh balik memiliki dinding yang lebih tipis dibandingkan dengan pembuluh nadi. Vena juga memiliki katup yang membantu darah untuk mengalir maju dan mencegah darah mengalir kembali ke tempat semula.
Darah miskin oksigen dari seluruh tubuh akan dibawa oleh vena kembali ke jantung. Lalu melalui pembuluh nadi paru, darah miskin oksigen dikirim ke paru untuk dibersihkan dan diganti dengan darah kaya oksigen. Darah beroksigen lalu dikirimkan paru ke jantung melalui pembuluh balik paru.
Sumbatan pada pembuluh balik akan menghambat aliran darah balik ke jantung, sehingga juga mengganggu keseluruhan sirkulasi darah di dalam tubuh. Apa pun yang menghambat aliran darah pada tubuh akan mengakibatkan organ tidak mendapatkan asupan oksigen dan nutrisi yang cukup.
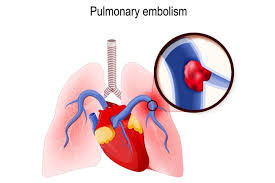
Selain itu, jika aliran darah pembuluh balik terhambat, darah dapat menumpuk dan terbentuk gumpalan darah. Gumpalan darah yang terlepas (emboli) dapat menyumbat pembuluh darah organ lain, termasuk paru. Sumbatan pada pembuluh darah paru merupakan kondisi gawat darurat dan mengancam nyawa. Sumbatan pada pembuluh darah otak dapat menyebabkan stroke.
Penyebab
Penyebab tersumbatnya aliran darah balik (vena) meliputi:
- Varises, yaitu pembuluh balik yang tampak melebar dan berkelok. Kondisi ini disebabkan karena rusaknya katup vena sehingga darah tidak dapat mengalir maju dan justru mengalir kembali ke tempat sebelumnya. Darah yang menumpuk menyebabkan vena melebar
- Spider veins, mirip dengan varises, namun lebih tipis
- Insufisiensi vena, yaitu rusaknya katup vena sehingga darah tidak bisa mengalir maju dan menumpuk di pembuluh balik. Biasanya terjadi pada vena yang terletak lebih dalam
- Penggumpalan darah (trombosis), karena adanya kerusakan dinding pembuluh darah akibat plak kolesterol atau cedera pembuluh darah
- Tromboflebitis, peradangan vena yang menyebabkan terbentuknya gumpalan darah
- Trombosis vena dalam (deep vein thrombosis/DVT), yaitu gumpalan darah yang terbentuk di vena dalam
- Emboli paru, yaitu bekuan darah yang terlepas dan menyumbat pembuluh darah organ lain
Penyebab tersumbatnya aliran darah balik vena lainnya adalah tumor/kanker dan pembengkakan jaringan yang menghimpit vena, tension pneumotoraks, serta cardiac tamponade. Selain menekan vena, kanker juga meningkatkan substansi tertentu dalam tubuh yang membuat darah mudah menggumpal.
Faktor Risiko
- Usia lanjut
- Obesitas
- Merokok
- Menderita tumor atau kanker
- Cedera atau kelemahan otot kaki
- Riwayat keluarga dengan masalah pembekuan darah
- Perubahan hormon selama menopause atau hamil
- Riwayat cedera, operasi, atau tirah baring untuk waktu yang lama
- Tidak aktif dalam jangka yang cukup lama, baik karena harus berbaring di tempat tidur atau bepergian dengan mobil dan pesawat untuk waktu yang lama
- Terpasang pacemaker 'alat pacu jantung' atau selang pembuluh darah (kateter) pada vena pusat
Gejala
Obstruksi atau sumbatan vena paling sering terlihat dalam bentuk DVT. Pasien datang dengan pembengkakan kaki setelah tidak aktif bergerak dalam waktu yang lama. Gejala lainnya adalah nyeri kaki yang memberat jika mengangkat pergelangan kaki. Pembengkakan adalah salah satu gejala DVT yang paling spesifik.
Gejala trombosis vena hepatika meliputi nyeri perut kanan atas, mual, dan/atau demam. Vena hepatika adalah vena yang membawa darah kotor dari hati ke vena kava inferior untuk dikembalikan ke jantung. Pasien juga dapat mengalami asites dan iskemia usus karena adanya gumpalan darah kecil pada pembuluh darah. Asites adalah penumpukan cairan di rongga perut, sedangkan iskemia adalah kondisi kekurangan oksigen pada jaringan.
Pada emboli paru, dapat timbul nyeri dada dan sesak napas. Kondisi ini dapat mengancam nyawa.
Diagnosis
Diagnosis ditegakkan berdasarkan gejala, riwayat kesehatan pasien, pemeriksaan fisik, dan pemeriksaan penunjang. Pemeriksaan dilakukan berdasarkan penyebab sumbatan yang terjadi.
Pemeriksaan DVT meliputi pemeriksaan darah untuk membantu menggolongkan risiko pasien. Pemeriksaan tersebut antara lain pemeriksaan D-dimer, kadar antithrombin lll (ATlll), NT-proBNP, CRP, dan laju endap darah (LED). Penelitian menunjukkan bahwa semua pasien dengan D-dimer positif dan pembengkakan kaki telah terkonfirmasi mengalami DVT. Pemeriksaan radiologi meliputi ultrasound (USG) pada kaki dan panggul yang terkena. Beberapa pasien mungkin memerlukan pemeriksaan CT scan atau MRI.
Untuk pemeriksaan insufisiensi vena, dapat menggunakan venogram dan USG. Pada venogram, dokter akan memasukkan pewarna kontras ke dalam pembuluh darah. Lalu diambil gambar pembuluh darah menggunakan sinar X. Pewarna kontras membantu dokter untuk melihat gambar pembuluh darah dengan lebih jelas.
Sementara, USG digunakan untuk menilai kecepatan dan arah aliran darah di dalam pembuluh darah. Gambar ditangkap melalui pantulan gelombang suara alat USG lalu ditampilkan di layar.
Pemeriksaan penunjang untuk trombosis vena hepatika meliputi uji laboratorium berupa pemeriksaan penggumpalan darah (koagulasi) untuk menyingkirkan kelainan koagulasi bawaan, uji fungsi hati, dan radiografi. USG adalah modalitas utama dan dapat dilakukan dengan endoskopi.
Tata Laksana
Terapi bergantung pada penyebab obstruksi vena. Pada sumbatan vena karena gumpalan darah (VTE), terapi bertujuan untuk mencegah perluasan DVT dan timbulnya emboli paru. Pengobatan dibagi menjadi fase pengobatan aktif awal selama 3 bulan dan dilanjutkan dengan fase sekunder. Pengobatan awal terdiri dari pemberian obat anti penggumpalan darah (antikoagulan) untuk menurunkan risiko emboli pada pasien DVT dan mengurangi risiko kematian pada pasien emboli paru. Trombektomi, atau menghilangkan gumpalan darah pada obstruksi vena termasuk jarang dilakukan.
Pengobatan untuk obstruksi vena hepatika meliputi pemecahan gumpalan darah (trombolisis) menggunakan tPA diikuti dengan terapi antikoagulasi jangka panjang minimal 3 bulan.
Komplikasi
Komplikasi VTE adalah emboli paru pada nadi paru yang dapat menyebabkan kematian karena darah tidak mengalir ke paru dengan normal. Komplikasi trombosis vena hepatika antara lain splenomegali (limpa membengkak), varises kerongkongan dan lambung dengan atau tanpa pendarahan, portal hypertensive gastropathy, dan asites.
Sementara, komplikasi insufisiensi vena antara lain:
- Deep vein thrombosis
- Emboli paru
- Ulserasi vena
- Limfedema sekunder
- Ulkus kaki
- Perubahan warna kulit
- Thrombophlebitis
- Pendarahan
- Nyeri kronis
Nyeri kronis, pembengkakan, selulitis berulang, dan ulkus kaki jangka panjang yang sulit sembuh adalah gejala sisa yang paling umum dari insufisiensi vena, namun bukan yang paling parah.
Pencegahan
Untuk menghindari pembekuan darah dan masalah pembuluh darah lainnya, lakukan pola hidup sehat berikut:
- Olahraga 3-5 kali dalam seminggu
- Berhenti merokok
- Kurangi asupan alkohol
- Menjaga berat badan ideal
- Makan makanan rendah lemak jenuh
- Hindari duduk dalam waktu lama. Jika sedang dalam perjalanan panjang, berdiri dan berjalanlah sesekali untuk menghindari penggumpalan darah
- Pemeriksaan kesehatan rutin ke dokter, terutama jika Anda memiliki faktor risiko
Kapan Harus ke Dokter?
Segera kunjungi unit gawat darurat jika:
- Sesak nafas tiba-tiba
- Nyeri dada
- Pingsan
- Tiba-tiba sakit kepala berat
- Mual dan muntah
- Tiba-tiba kabur atau penglihatan ganda
- Tiba-tiba lemas atau mati rasa di wajah atau bagian tubuh lain
- Kesulitan berbicara atau memahami orang lain
- Kejang
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Anita Larasati Priyono
Packer CF, Bickel S, Dattilo JB. (2021). Vein obstruction. Retrieved 25 April 2022, from https://www.ncbi.nlm.nih.gov/books/NBK537255/
A visual guide to vein and artery problems. (2021). Retrieved 25 April 2022, from https://www.webmd.com/dvt/ss/slideshow-visual-guide-to-vein-and-artery-problems
Nicola S. (2021). What's the difference between arteries, veins, and capillaries?. Retrieved 25 April 2022, from https://www.webmd.com/heart/difference-between-arteries-veins-capillaries#:~:text=Arteries%20carry%20blood%20away%20from,to%20keep%20your%20blood%20flowing.
The difference between arteries and veins. (2021). Retrieved 25 April 2022, from https://www.webmd.com/heart/difference-between-arteries-and-veins#091e9c5e821a0ff3-2-9