Definisi
Trauma pada bola mata dibagi menjadi dua jenis, yaitu tumpul dan tajam. Kondisi ini dikelompokkan berdasarkan jenis benda yang menyebabkan trauma tersebut. Trauma ini dapat terjadi pada semua orang, tanpa peduli usia, jenis kelamin, dan ras. Namun, faktor risiko dan penyebab tersering akan berbeda-beda tergantung negara, lingkungan, serta kelas ekonomi. Biasanya, trauma ini hanya terjadi pada satu mata saja, sehingga gejala hingga komplikasi kondisi ini terpusat pada mata yang terdampak.
Penyebab
Benda tumpul yang dapat menjadi penyebab trauma dapat berupa tonjokan tangan, bola, meja, dan sebagainya. Sementara itu, benda tajam dapat berupa pisau, gunting, kuku, sekrup, peluru, dan sebagainya. Pengaruh trauma tergantung dari tumpul atau tajamnya benda, kecepatan benturan, titik pusat benturan, bahan dasar benda yang membentur, serta hal-hal lainnya yang mempengaruhi besar energi saat terjadinya benturan. Biasanya, trauma terjadi di rumah atau tempat kerja.
Di Amerika Serikat, terdapat daftar benda yang sering menyebabkan trauma pada mata. Pada orang dewasa, benda yang sering menyebabkan trauma pada mata adalah batu, tonjokan, bola bisbol, kayu, dan alat pemancing ikan. Pada remaja, penyebab tersering adalah peluru mainan dan paintball. Sementara itu, pada lansia, trauma pada bola mata pada umumnya terjadi akibat terjatuh atau terpeleset, ditambah dengan faktor risiko lemahnya struktur bola mata seiring dengan penuaan.
Faktor Risiko
Berdasarkan kemungkinan pekerjaan, situasi, dan benda yang berisiko menyebabkan trauma pada mata, pria lebih sering mengalami trauma pada bola mata daripada wanita. Selain itu, usia puncak terjadinya trauma pada bola mata adalah 30-40 tahun. Hal ini disebabkan ketidakpatuhan dalam menggunakan alat pelindung diri saat bermain bisbol, basket, sert membetulkan alat-alat listrik di rumah. Tidak hanya itu, faktor risiko lainnya adalah penyalahgunaan zat terlarang, termasuk mabuk akibat alkohol dan ganja.
Gejala
Gejala yang dapat terjadi akibat trauma tergantung dari benda penyebab dan besar dampaknya. Pada trauma tajam, keluhan yang biasa muncul berupa nyeri dan pandangan ganda. Jika benda penyebab kecil, keluhan seperti sensasi benda asing dapat juga muncul. Jika luka menembus ke dalam bola mata, keluhan seperti mata merah dan sensitif terhadap cahaya juga dapat muncul. Sementara itu, pada trauma tumpul, keluhan-keluhan seperti di atas dapat terjadi, ditambah dengan beberapa gejala pada kelopak dan kulit di sekitar mata, seperti bengkak atau memar dan luka gores pada kelopak atau kulit sekitar mata. Jika trauma cukup parah hingga tulang-tulang kecil di belakang bola mata patah, mata dapat terlihat seperti melesak ke dalam, kesulitan menatap ke atas, serta rasa baal di pipi persis di bawah mata.
Diagnosis
Sebelum memeriksa mata, biasanya dokter akan melakukan pemantauan terhadap tanda vital seperti denyut nadi dan tekanan darah, karena keduanya dapat dipengaruhi oleh cedera yang terjadi pada mata.
Diagnosis trauma pada bola mata dapat ditegakkan lewat pemeriksaan secara langsung. Dokter biasanya akan memeriksa fungsi mata seperti tajam penglihatan, refleks mata terhadap cahaya, serta lapang pandang. Namun, pemeriksaan tekanan bola mata biasanya dihindari karena dapat menekan bola mata sehingga memperparah trauma, terutama pada trauma tajam. Tekanan bola mata dapat diperiksa pada trauma tumpul, karena dapat memperkirakan adanya kemungkinan perdarahan dalam. Pemberian obat tetes mata juga perlu dihindari jika luka terbuka atau tembus.
Setelah itu, dokter biasanya akan melakukan pemeriksaan jaringan sekitar mata dengan menyentuh secara lembut. Untuk mengetahui kondisi tulang dan jaringan sekitar, pencitraan seperti foto rontgen dan CT scan dapat pula dilakukan. MRI juga dapat menjadi pilihan, kecuali jika benda yang terlibat merupakan logam. Selain itu, pergerakan bola mata juga akan diperiksa untuk mengetahui adanya kerusakan pada otot bola mata.
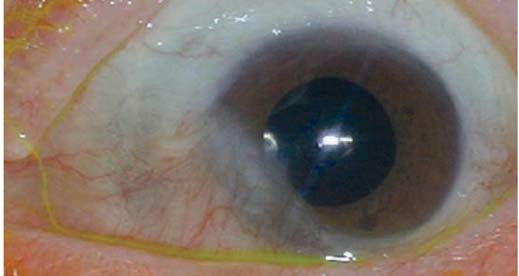
Pemeriksaan slit lamp dapat pula dilakukan jika ada kecurigaan keterlibatan struktur di dalam mata seperti katarak pada lensa, lepasnya lapisan penerima cahaya (retina) di bola mata, serta adanya benda yang tembus ke dalam bola mata.
Tata Laksana
Tata laksana trauma pada bola mata akan tergantung kepada jenis luka dan keparahannya. Jika trauma tumpul ringan, tata laksana dapat berupa mendinginkan mata untuk menghentikan perdarahan dan mengecilkan bengkak. Anda juga dapat diresepkan obat antinyeri dan diminta untuk tirah baring agar trauma tidak semakin parah. Jika pemeriksaan menunjukkan adanya kekeruhan pada mata, Anda dapat dioperasi karena risiko glaukoma (kenaikan tekanan pada bola mata) cukup tinggi. Dokter dapat pula memberikan obat penurun tekanan bola mata terutama jika tekanan bola mata meningkat. Katarak yang terjadi setelah trauma juga menjadi indikasi operasi.
Sementara itu, pada trauma tajam, obat yang perlu diberikan utamanya adalah antibiotik untuk mencegah infeksi. Obat-obatan seperti anti nyeri dan penurun tekanan bola mata, serta obat-obatan untuk mengecilkan pupil dapat pula diberikan untuk menurunkan radang dan nyeri. Pembedahan dapat pula dilakukan jika terjadi katarak atau glaukoma, serta jika benda penyebab tembus ke dalam bola mata.
Jika bola mata rusak, pemberian obat pencahar dan penurun batuk dapat diberikan. Hal ini dilakukan karena mengejan dan batuk dapat menaikkan tekanan bola mata secara tiba-tiba, yang selanjutnya dapat memperparah kerusakan bola mata.
Komplikasi
Komplikasi trauma pada bola mata bermacam-macam. Pertama adalah katarak, yang merupakan kekeruhan lensa mata. Katarak dapat terjadi setelah trauma akibat kerusakan pada lensa. Selain itu, glaukoma atau peningkatan tekanan bola mata dapat pula terjadi. Glaukoma pada trauma dapat disebabkan oleh kerusakan lensa atau kerusakan struktur lainnya pada bola mata bagian depan. Jika otot mata terlibat dalam trauma, denyut nadi dapat menurun hingga terjadi syok atau kegagalan fungsi peredaran darah. Jika trauma bersifat tajam atau tembus, risiko infeksi pada bola mata meningkat. Terlepas dari keberadaan infeksi, komplikasi yang dapat terjadi adalah kebutaan.
Pencegahan
Trauma pada bola mata dapat dicegah dengan menangani faktor risiko yang ada, seperti berikut:
- Gunakan kacamata pelindung atau pelindung mata lainnya saat bekerja, pelindung ini dapat menurunkan risiko mata terkena partikel yang dapat menembus bola mata, atau mencegah benturan secara langsung ke mata
- Gunakan helm dengan penutup wajah saat berkendara dengan sepeda motor, jika terjadi kecelakaan, benturan tidak langsung mengenai bola mata
- Gunakan pelindung mata saat berolahraga, olahraga yang melibatkan bola atau kok bulutangkis dapat menyebabkan trauma tumpul ataupun tajam ke bola mata
Kapan Harus ke Dokter?
Jika mata Anda kemasukan partikel benda yang cukup kecil atau terbentur, Anda dapat mempertimbangkan untuk pergi ke dokter. Jika benda cukup kecil, Anda mungkin akan membutuhkan bantuan orang lain untuk memeriksa apakah benda tersebut tampak menancap atau tidak. Jika benda tampak menancap, Anda perlu untuk segera ke dokter. Sementara itu, jika mata Anda terbentur benda tumpul, Anda harus memeriksakan ke dokter jika kulit di sekitar bola mata tampak memar atau bengkak, atau jika pandangan Anda menjadi blur atau ganda.
Mau tahu lebih lanjut seputar penyakit-penyakit lainnya? Cek di sini, ya!
- dr Ayu Munawaroh, MKK
Garg, A., Patel, A., Al-Aswad, L., Moore, D., Shah, M., & Houser, K. (2021). Ocular Trauma: Acute Evaluation, Cataract, Glaucoma - EyeWiki. Retrieved 19 October 2021, from https://eyewiki.aao.org/Ocular_Trauma:_Acute_Evaluation,_Cataract,_Glaucoma.
Patel, S., Feldman, B., Shah, V., Murchison, A., Parker, P., & Hsu, J. (2021). Ocular Penetrating and Perforating Injuries - EyeWiki. Retrieved 19 October 2021, from https://eyewiki.aao.org/Ocular_Penetrating_and_Perforating_Injuries.
Quick Facts: Blunt Eye Injuries - MSD Manual Consumer Version. (2020). Retrieved 19 October 2021, from https://www.msdmanuals.com/home/quick-facts-injuries-and-poisoning/injuries-to-the-eye/blunt-eye-injuries.