Definition
Brain tumors can be classified into two types: primary brain tumors and secondary brain tumors. Primary brain tumors originate from brain cells, while secondary brain tumors are cancers from other organs that spread to the brain (metastasis). Tumors that metastasize are malignant and are also known as cancers.
Secondary brain tumors can be singular or multiple in the brain. When brain metastasis occurs, the tumor exerts pressure on the brain and disrupts the function of surrounding brain tissue. This leads to symptoms such as headaches, personality changes, memory loss, or seizures.
Cancer treatment that has spread to the brain includes surgical procedures, radiation, chemotherapy, immunotherapy, or a combination of therapies. Other treatments may also be recommended in certain situations. The focus of treatment is to alleviate pain and other symptoms caused by cancer.
Causes
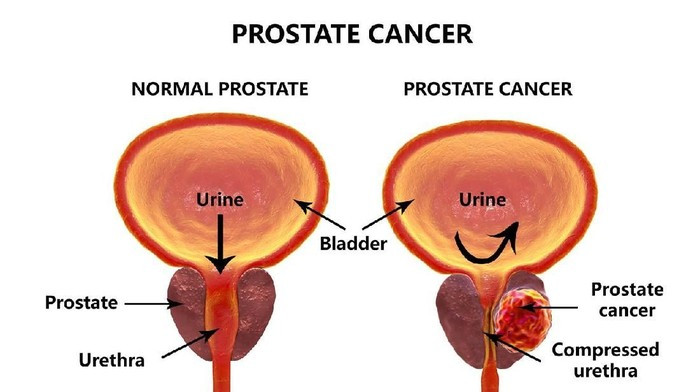
Secondary brain tumors occur when malignant tumors from other organs spread to the brain. Cancer cells spread through the bloodstream or the lymphatic system. Cancers in any organ can spread to the brain, but the malignancies most commonly metastasizing to the brain include breast cancer, lung cancer, colorectal cancer, kidney cancer, and melanoma. Secondary brain tumors are a frequent complication of cancer and are the most commonly found type of brain tumor.
Risk factor
All types of cancer can spread to the brain, but some are more likely to cause brain metastases, including:
- Lung cancer
- Breast cancer
- Colorectal cancer
- Kidney cancer
- Melanoma
Secondary brain tumors typically develop in people aged 45-65, with most cases occurring in those older than 65.
Symptoms
The signs and symptoms caused by brain metastases vary depending on the location, size, and growth rate of the tumor. These symptoms include:
- Headache, sometimes accompanied by nausea and vomiting
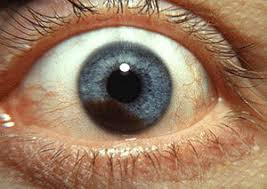
- Blurred vision
- Mental changes, such as worsening memory problems
- Seizures
- Weakness or numbness in one side of the body
Diagnosis
If brain metastasis is suspected, the doctor may perform several examinations, including neurological tests, imaging, and tissue biopsy.
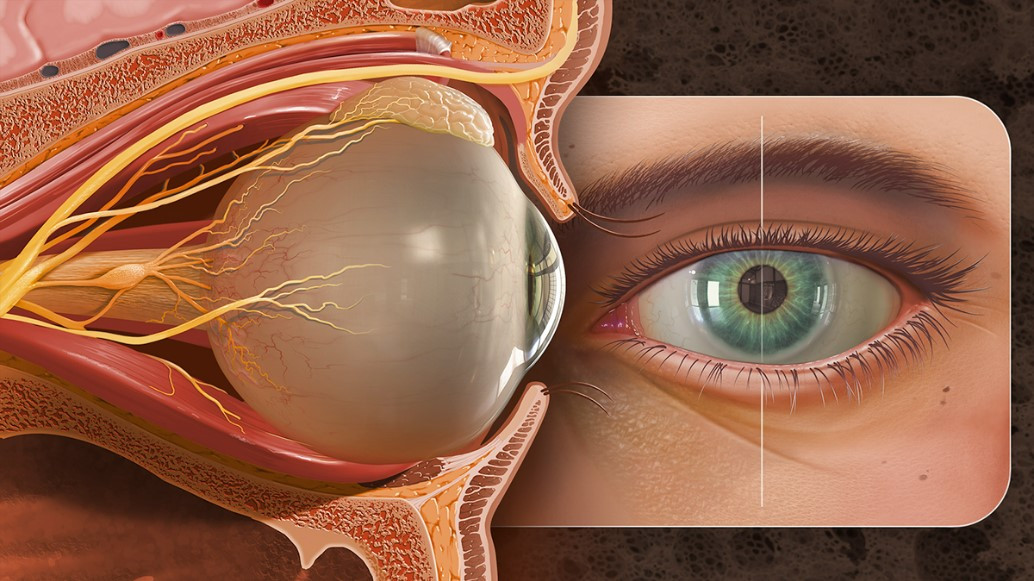
Neurological examination includes tests of vision, hearing, balance, coordination, strength, and reflexes. Any abnormalities can indicate the tumor's location in the brain.
Imaging tests such as Magnetic Resonance Imaging (MRI) are commonly used to help diagnose brain metastases. Specific MRI tests, including functional MRI, perfusion MRI, and magnetic resonance spectroscopy, help doctors evaluate the tumor and plan treatment. Other imaging tests, like Computerized Tomography (CT) scans and Positron Emission Tomography (PET), can also aid in diagnosis. For instance, if the primary tumor causing brain metastasis is unknown, a chest CT scan might be done to check for lung cancer.
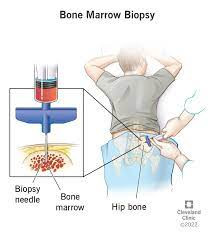
In a biopsy, a small tissue sample suspected to be a tumor is examined under a microscope to determine if it is malignant or benign. The biopsy can be done during surgery to remove the tumor or with a needle. This analysis helps diagnose the tumor, estimate prognosis, and evaluate treatment options.
Management
Treatment for secondary brain tumors aims to relieve symptoms, slow tumor growth, and prolong life. Even with successful treatment, brain metastases often recur, necessitating close monitoring after treatment.
Treatment options for brain metastases include medications, surgery, stereotactic radiosurgery, radiation therapy, or a combination of these therapies. The best treatment choice for each patient depends on the tumor type, size, number, location, symptoms, overall health, and patient preference. Discuss treatment options with your doctor.
Medications to control symptoms
- Steroids: High-dose corticosteroids can reduce brain tissue swelling around the tumor, alleviating symptoms. These drugs require a doctor's prescription.
- Anti-seizure medications: If seizures occur, doctors may prescribe medications to prevent additional seizures, also requiring a prescription.
Surgery
If surgery is a treatment option and the tumor is accessible, a surgeon will remove as much of the tumor as possible. Even partial removal can reduce symptoms. Surgery carries risks such as nerve function impairment, infection, and bleeding, as well as potential functional impairments depending on the tumor's brain location.
Radiation therapy
Radiation therapy uses high-energy beams, like X-rays and protons, to kill tumor cells. For secondary brain tumors, radiation may involve one or both of the following methods:
- Whole-brain radiation
This treats the entire brain to kill tumor cells, typically requiring 10-15 sessions over 2-3 weeks. Side effects include fatigue, nausea, and hair loss, with long-term use linked to cognitive decline.
- Stereotactic radiosurgery (SRS)
This delivers highly focused radiation to the tumor. SRS is usually done in a single session, and multiple tumors can be treated simultaneously. Side effects include nausea, headache, seizures, or dizziness, with a lower risk of long-term cognitive decline compared to whole-brain radiation.
Medications
Certain cases require medications to control the tumor. The effectiveness depends on the cancer's origin and the patient's health. These options include:
- Chemotherapy: Uses drugs to kill rapidly growing cells, including cancer cells.
- Targeted therapy drugs: These drugs target specific abnormalities in cancer cells, stopping their growth.
- Immunotherapy: Utilizes the body's immune system to fight cancer by disrupting the cancer cells' ability to hide from immune detection.
Post-treatment rehabilitation
Since brain tumors can affect motor skills, speech, vision, and thinking, rehabilitation is necessary during recovery. Doctors may refer patients to the following therapists:
- Physical therapists: Help regain motor skills and muscle strength.
- Occupational therapists: Assist in returning to daily activities and work.
- Speech therapists: Help with speech difficulties.
Supportive (Palliative) Care
Palliative care focuses on relieving pain and symptoms of serious illness. Palliative care specialists work with patients, families, and doctors to provide additional support during treatment. This care, involving medical, psychological, spiritual, and social work professionals, aims to improve the quality of life for cancer patients and their families.
Complications
Secondary brain tumors can cause serious complications such as:
- Brain herniation (shifting of brain tissue)
- Increased intracranial pressure
- Seizures
- Stroke
- Hydrocephalus (fluid buildup in the brain)
- Spread to surrounding tissues
- Neurological deficits
- Brain swelling
- Cognitive dysfunction
- Intracranial bleeding
- Spinal cord compression
- Death
Prevention
There is no known way to prevent brain cancer, but you can reduce your risk by avoiding exposure to pesticides, insecticides, carcinogenic chemicals, smoking, and unnecessary radiation. Since most secondary brain tumors originate from lung, breast, and melanoma cancers, treating these cancers is the first step in reducing the risk of brain metastasis. Discuss your risk of secondary brain tumors with your doctor.
When to see a doctor?
Seek medical attention if you or someone you know experiences warning signs such as limb weakness, mental changes, severe headaches, and seizures. Inform your doctor of any past cancer or tumor treatment if these symptoms occur.
Looking for more information about other diseases? Click here!
- dr Hanifa Rahma
Mayo Clinic Staff (2020). Brain metastases. Retrieved 23 Desember 2021, from https://www.mayoclinic.org/diseases-conditions/brain-metastases/symptoms-causes/syc-20350136
Amsbaugh, M. Kim, C. (2020). Brain Metastasis. Retrieved 23 Desember 2021, from https://www.ncbi.nlm.nih.gov/books/NBK470246/
Cleveland Clinic (2020). Metastatic brain tumors. Retrieved 23 Desember 2021, from https://my.clevelandclinic.org/health/diseases/17225-metastatic-brain-tumors#prevention
Roth, P., Pace, A., and Rhun, E. (2020). Neurological and vascular complications of primary and secondary brain tumours: Eano-ESMO clinical practice treatment and follow-up. Annals of oncology. Vol. 32, Issue 2, P171-182.