Definisi
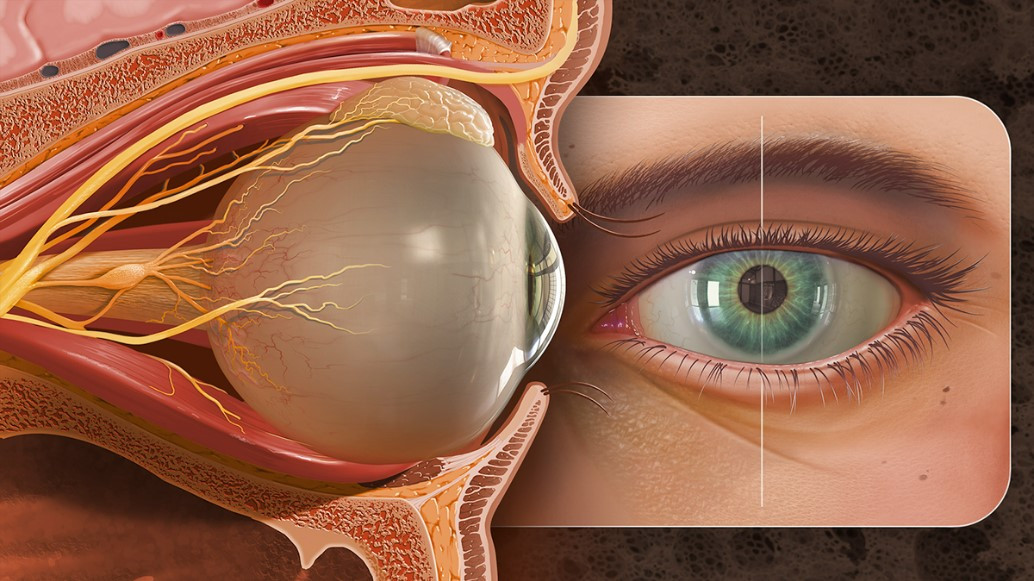
Area orbita adalah rongga pada tengkorak tempat bola mata dan jaringan sekitar mata. Jaringan-jaringan yang berada di rongga orbita antara lain otot mata, pembuluh darah, saraf mata, kelenjar air mata, dan jaringan lemak. Rongga orbita tersusun dari tulang tengkorak yang berfungsi untuk melindungi bola mata jaringan orbita lainnya yang mengelilingi mata.
Area orbita berbentuk menyerupai buah pir dengan bukaan terlebar pada bagian depan dan menyempit di bagian belakang. Karena rongga orbita adalah area yang relatif kecil, jika ada lesi atau pertumbuhan abnormal yang menempati ruang akan meningkatkan volume orbital dan menyebabkan proptosis atau penonjolan bola mata. Hal tersebut akan mempengaruhi fungsi otot mata dan mengganggu penglihatan.
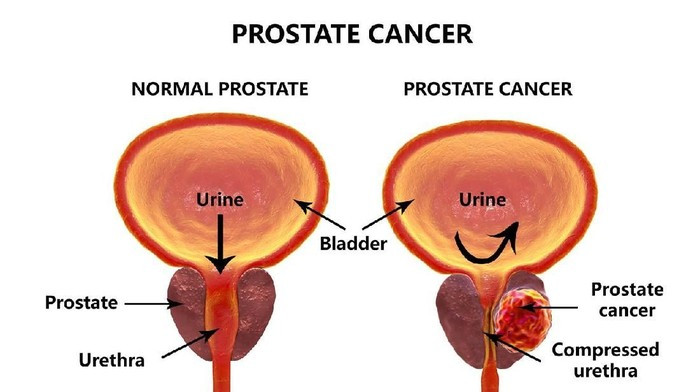
Tumor orbita adalah pertumbuhan abnormal pada jaringan-jaringan di dalam rongga orbita. Tumor dapat bersifat jinak ataupun ganas dan bisa berasal dari jaringan orbita itu sendiri atau merupakan penyebaran tumor dari bagian tubuh lain (metastasis).
Jenis tumor orbital sangat bervariasi, seperti kista, tumor vaskuler atau pembuluh darah, limfoma, tumor neurogenik dari saraf, dan tumor sekunder yang bermetastasis dari rongga sinus atau rongga kepala di sekitar mata.
Penyebab
Tumor orbital primer atau yang berasal dari jaringan orbital, meskipun cukup jarang, mencakup tumor jinak dan ganas. Semua struktur orbita dapat mengalami pertumbuhan abnormal. Penyebaran tumor secara langsung (metastasis) dari bagian tubuh yang berdekatan dapat menyebabkan desakan pada rongga orbital.
Hemangioma kapiler adalah tumor orbital yang paling umum ditemukan pada anak-anak. Tumor yang bersifat jinak dan dilapisi oleh lapisan pembuluh darah ini sering ditemukan saat lahir atau pada 3 bulan pertama kehidupan. Tumor ini dapat membesar. Tumor orbital jinak lainnya antara lain dermoid, limfangioma, dan tumor histiositik.
Rhabdomiosarkoma dan tumor mesenkimal adalah tumor orbita ganas paling umum pada anak-anak yang berasal dari rongga orbita. Tumor yang merusak ini biasanya terjadi pada anak-anak <2 tahun atau >6 tahun. Tumor ganas ini sering dijumpai pada area orbita yang dekat dengan hidung bagian belakang.
Neuroblastoma, sarkoma Ewing, tumor Wilms, dan leukemia adalah tumor orbital metastatik yang lebih sering menyerang anak-anak. Tumor ganas lainnya meliputi limfoma Burkitt dan sarkoma granulositik.
Pada orang dewasa, hemangioma kavernosa adalah tumor orbital yang paling umum ditemukan. Pada CT scan, tumor ini berbentuk bulat, berkapsul, dan berbatas tegas. Secara histologis atau pemeriksaan jaringan, terlihat ruang besar berisi darah dengan lapisan pembuluh darah dan otot polos. Tumor ini biasanya dapat diterapi dan ditoleransi dengan baik oleh pasien, kecuali jika ada gangguan ketajaman penglihatan atau lapang pandang.
Faktor Risiko
Beberapa faktor risiko tumor orbita antara lain:
- Perkembangan mata yang abnormal. Anak dapat tumbuh dengan ketidaknormalan pada salah satu bagian tubuhnya, termasuk mata
- Memiliki penyakit mata tiroid. Orang dengan penyakit Grave, yaitu sebuah penyakit autoimun, memiliki risiko mengalami tumor orbita
Gejala
Terkadang, tumor tidak menimbulkan gejala di awal dan gejala memberat perlahan dalam jangka waktu yang lama. Sementara pada pasien lainnya, gejala dapat timbul sangat cepat. Lokasi dan sifat gejala masing-masing tumor dapat menjadi petunjuk penting untuk menentukan apakah apakah tumor bersifat jinak atau ganas.
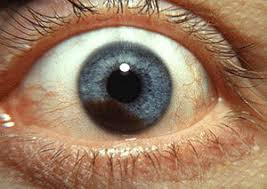
Banyak pasien mengalami penonjolan mata (proptosis atau exophthalmos) karena adanya penekanan pada bola mata. Karena bola mata menonjol, kelopak mata tidak dapat tertutup rapat. Kondisi ini dapat menimbulkan kekeringan dan iritasi pada selaput luar bola mata.
Beberapa tumor sebenarnya dapat terlihat atau teraba pada pemeriksaan. Beberapa tumor dapat menyebabkan penurunan penglihatan, kehilangan penglihatan sementara, atau penglihatan ganda.
Pemeriksaan pasien dengan dugaan tumor orbital dimulai dengan menggali riwayat gejala pada mata dan riwayat kesehatan menyeluruh. Durasi dan tingkat perkembangan tanda dan gejala pasien sangat penting. Nyeri, pandangan ganda, rasa berdenyut, dan gangguan ketajaman penglihatan adalah gejala yang harus diperiksa. Riwayat cedera dan riwayat keluarga dengan tumor orbita juga dapat membantu diagnosis.
Pada pemeriksaan mata, perubahan di sekitar orbita akan lebih terlihat jelas jika pemeriksaan dilakukan di ruangan dengan penerangan yang baik.
Hipertelorisme atau peningkatan jarak abnormal antara dua mata, proptosis atau penonjolan bola mata, pembengkakan dan memar kelopak mata, serta pelebaran pembuluh selaput bening mata adalah beberapa tanda yang ditemukan di sekitar orbita.
Blepharoptosis atau kelopak mata atas jatuh ke bawah secara tidak normal dan lagophthalmos atau penutupan kelopak mata yang tidak sempurna adalah tanda-tanda tambahan yang harus diperhatikan saat pemeriksaan.
Penonjolan mata merupakan tanda penting dari penyakit orbita. Penonjolan ini disebut sebagai proptosis atau exophthalmos.
Perabaan orbita bagian depan dapat menilai tingkat nyeri tekan, konsistensi, dan apakah tumor dapat digerakan atau terfiksasi. Nyeri tekan menunjukkan adanya proses peradangan atau penekanan saraf oleh tumor, seperti pada kanker kistik adenoid kelenjar air mata.
Perabaan juga harus dilakukan pada kelenjar getah bening dan pembuluh darah di sekitar orbita. Perabaan dapat menilai apakah ada pulsasi dari sambungan pembuluh arteri dan vena yang abnormal atau pulsasi dari organ rongga kepala yang keluar melalui celah pada tulang orbita, seperti yang terjadi pada ensefalokel atau tonjolan isi tengkorak.
Auskultasi atau pemeriksaan suara organ menggunakan alat stetoskop pada area orbita dapat mendeteksi adanya aliran darah abnormal pada rongga orbita atau di dalam tengkorak. Jika dicurigai adanya tumor dengan aliran darah yang meningkat, pemeriksaan arteriografi harus dilakukan untuk menilai tumor ini.
Penurunan ketajaman penglihatan, kelainan pupil, gangguan pergerakan bola mata, dan pandangan ganda harus dinilai dan dengan hati-hati. Tekanan bola mata dapat meningkat dan pemeriksaan slit lamp dapat menilai memar serta pembesaran pembuluh darah. Pemeriksaan funduskopi dapat menunjukan pembengkakan dan pucat pada cawan saraf optik, ablasio retina atau terlepasnya retina dari penempelan, adanya lipatan lapisan koroid, serta pembentukan jalur pembuluh darah baru yang abnormal.
Diagnosis
Pemeriksaan yang cermat oleh dokter mata sangat penting untuk diagnosis tumor orbital. Dokter akan menilai gejala dan melakukan pemeriksaan penglihatan, struktur, dan fungsi bagian-bagian orbita. Jika diperlukan, akan dilakukan pemeriksaan penunjang seperti USG, CT scan, dan MRI untuk menilai dengan lebih teliti.
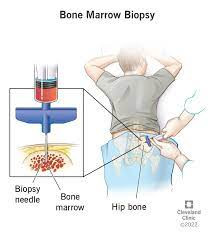
Karena kebanyakan tumor memiliki temuan yang khas pada pemeriksaan, biopsi tidak selalu diperlukan. Namun, pada keadaan tertentu biopsi diperlukan untuk menentukan jenis tumor.
Pemeriksaan Laboratorium
Pemeriksaan laboratorium dilakukan jika ada pemeriksaan fisik yang mengarah ke tumor orbita.
Pemeriksaan Radiologi
CT scan menjadi pemeriksaan utama tumor orbital. CT scan dapat menilai jaringan dan tulang dengan rinci, termasuk pada area orbital. CT scan dengan kontras dapat melihat proses peradangan dan tumor pembuluh darah.
Magnetic resonance imaging (MRI) sangat baik untuk menilai jaringan tubuh, termasuk area orbita. MRI memberikan resolusi jaringan lunak yang sangat baik, namun CT scan lebih unggul dalam menilai struktur tulang orbital.
USG okular atau USG mata dapat menilai lesi orbital bagian depan dan tengah. USG Doppler digunakan untuk evaluasi pembuluh darah orbital dan aliran darah.
Prosedur diagnostik biopsi aspirasi jarum halus (FNAB) adalah teknik diagnosis tumor orbital dengan mengambil sejumlah kecil sampel sel tumor menggunakan jarum yang sangat halus. FNAB dapat membedakan tumor jinak dan ganas dengan akurasi 95%. FNAB ditambah dengan pemeriksaan klinis dan radiologis dapat mengarahkan diagnosis yang tepat pada 80% kasus.
Biopsi terbuka adalah metode umum untuk mendapatkan sampel jaringan tumor orbita. Biopsi mungkin juga diperlukan jika FNAB tidak dapat memperoleh jaringan yang memadai untuk pemeriksaan mikroskopik. Kelebihan biopsi terbuka adalah penegakan diagnosis setingkat jaringan karena dapat memperoleh spesimen jaringan yang cukup besar. Kekurangan biopsi antara lain tingkat kesakitan dan biaya yang lebih besar.
Tes Lain
Analisis genetik tumor telah membantu dalam identifikasi tumor.
Pedoman pengelompokan stadium menggunakan komponen TNM yang dianjurkan oleh American Joint Committee on Cancer (AJCC) digunakan untuk menentukan stadium kanker orbita. "T" menunjukkan karakteristik dan ukuran tumor, "N" menunjukkan status kelenjar getah bening di area sekitarnya, dan "M" berarti metastasis. Komponen TNM ini membagi stadium tumor menjadi 4 stadium.
Tata Laksana
Pengobatan
Terapi medis disesuaikan dengan diagnosis yang diperoleh melalui biopsi atau pengangkatan tumor. Pada kondisi tertentu tidak memerlukan biopsi atau eksisi untuk memulai pengobatan. Kondisi seperti selulitis orbital sering diobati secara medis dengan berbagai agen antimikroba. Pembedahan diperlukan jika tidak ada respons terhadap pengobatan atau muncul perburukan klinis. Penyakit radang orbital (pseudotumor) biasanya diobati secara medis dengan obat golongan steroid. Hemangioma kapiler juga dapat diobati dengan terapi non-bedah, seperti suntikan steroid.
Pembedahan
Metode pembedahan atau operasi bergantung pada lokasi dan ukuran tumor. Pembedahan yang disebut orbitotomi bisa dilakukan melalui kulit di sekitar mata atau area lain pada wajah dan kulit kepala. Akses bedah lainnya antara lain melalui konjungtiva atau selaput bening mata dan intrakranial atau dari dalam rongga kepala.
Komplikasi
Komplikasi tumor orbita antara lain kekeringan dan iritasi pada mata akibat kelopak mata tidak dapat tertutup rapat pada pasien yang mengalami penonjolan mata (proptosis atau exophthalmos).
Sedangkan komplikasi operasi yang paling ditakuti adalah kehilangan penglihatan. Hal ini dapat disebabkan karena tekanan berlebih pada bola mata dan penekanan pembuluh arteri retina pusat. Perdarahan dapat terjadi saat operasi dan pasca operasi, juga penekanan pada saraf optik dan sumbatan pembuluh arteri retina pusat.
Diplopia atau pandangan ganda akibat gangguan otot mata dapat disebabkan oleh cedera saraf atau otot secara langsung. Parestesia atau kelumpuhan otot mata dapat timbul jika ada cedera pada saraf mata.
Pencegahan
Sampai saat ini belum ditemukan cara pasti untuk mencegah tumor orbita. Diagnosis dan pengobatan yang cepat serta tepat dapat mencegah perburukan gejala hingga bisa mencegah komplikasi.
Kapan Harus ke Dokter?
Segera konsultasi ke dokter mata jika Anda mengalami tanda dan gejala tumor orbita seperti yang disebutkan di atas untuk mendapatkan penanganan yang tepat.
Mau tahu informasi seputar penyakit lainnya? Cek di sini,ya!
- dr Anita Larasati Priyono
Mercandetti M. (2019). Orbital tumors. Retrieved 3 April 2022, from https://emedicine.medscape.com/article/1218892-overview#showall
Orbital tumors. (2022). Retrieved 3 April 2022, from https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/orbital-tumors
Yen MT. (2021). Orbital masses. Retrieved 8 April 2022, from https://eyewiki.aao.org/Orbital_Masses