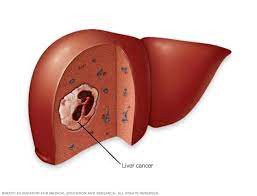
Definition
Hepatocellular Carcinoma (HCC) is a type of cancer originating from the parenchymal tissue of the liver (hepatocytes). It represents the most common liver cancer and ranks as the fourth leading cause of cancer-related deaths globally.
Over the last 20 years, the incidence of HCC has been on the rise. Projections suggest that by 2025, the number of HCC cases is expected to reach 1 million, with a continued increase until 2030 in some countries.
Notably, a high incidence is observed in Asia and Africa, where the prevalence of hepatitis B and C is also elevated. The correlation with these viral infections contributes to the development of chronic liver disease and the subsequent growth of HCC cases in these regions.
Causes
Hepatocellular Carcinoma (HCC) occurs when there is a mutation in the parenchymal tissue of the liver at the DNA level. The DNA of cells serves as the instruction manual for all chemical processes in the body. Mutations in the DNA result in changes to these instructions, leading to the uncontrolled growth of cells, the formation of tumors, and the development of cancerous cells.
Chronic hepatitis is a significant contributor to the development of HCC. However, HCC can also occur in individuals without a previous history of liver disease and can manifest without clear, identifiable causes.
Risk factor
Several factors can increase the risk of Hepatocellular Carcinoma (HCC), including:
- Liver Cirrhosis:
- Liver cirrhosis is a major risk factor for HCC, with approximately 80% of HCC cases having a history of cirrhosis. Causes of cirrhosis include fatty liver, alcohol abuse, and hepatitis B and C infections.
- Chronic Hepatitis B and C:
- Chronic hepatitis B and C infections elevate the risk of HCC. Concurrent infections, especially when combined with alcohol abuse, further increase the risk.
- Liver Carcinogens:
- Aflatoxin, a side product of fungal contamination in food, can act as a liver carcinogen. Exposure to this toxin through contaminated food can lead to DNA damage and genetic abnormalities.
- Hemochromatosis:
- Hemochromatosis, an excessive iron storage condition, can increase the risk of HCC, particularly when accompanied by liver cirrhosis.
- Diabetes:
- Individuals with diabetes have a higher risk of developing HCC compared to those without the condition.
- Excessive Alcohol Consumption:
- Prolonged and excessive alcohol consumption can damage the liver, significantly increasing the likelihood of developing liver cancer.
- Smoking:
- Smoking is associated with an increased risk of liver cancer. Individuals who quit smoking generally have a lower risk than those who continue smoking.
- Obesity:
- Obesity can lead to liver inflammation, especially non-alcoholic fatty liver disease, serving as a risk factor for HCC.
- Hereditary Liver Disease:
- Hereditary disorders like Wilson disease, which causes copper accumulation, can elevate the risk of liver cancer.
Symptoms
In the early stages of Hepatocellular Carcinoma (HCC), some individuals may not exhibit clear symptoms. However, as the disease progresses, the following symptoms may appear:
- Itchiness
- Yellowish Skin or Eyes (Jaundice)
- Blood Vomit
- Body Weight Loss
- Swelling or Bloating Abdomen
- Swelling in the Feet
- Hemorrhoids
- Low Appetite
- Weakness and Fatigue
- Upper Right Abdominal Pain (Rarely)
- Lump or Heavy Feeling in the Upper Abdomen
- Dark Urine or Pale Stool
- Fever
Diagnosis
To determine the diagnosis of Hepatocellular Carcinoma (HCC), the doctor will conduct a comprehensive assessment, including a medical interview, physical examination, and additional examinations.
During the medical interview, the doctor will inquire about the symptoms, their onset, as well as the patient's medical and family history. If there is suspicion of liver cancer or HCC, a focused physical examination will be performed to aid in the diagnosis.
If necessary, additional examinations may be conducted to confirm the diagnosis. These examinations include:
- Laboratory Exam: Complete blood tests and liver function tests are performed to assess the severity of HCC and identify any underlying causes.
- Imaging Examination: Ultrasonography is used to visualize abnormalities in the shape of the liver. CT scan or MRI scans provide detailed images of the liver, aiding in the diagnosis.
- Liver Biopsy: In some cases, a liver biopsy may be required. This involves taking a small sample of liver tissue for laboratory analysis to confirm the presence of cancer.
Management
The management of Hepatocellular Carcinoma (HCC) involves several therapeutic options, with the choice depending on factors such as the size and location of the tumor, liver damage, and overall health condition. The available therapies include:
- Surgery:
- Surgical excision of the cancer and surrounding healthy tissue is the preferred choice for early-stage HCC with good liver function.
- Liver Transplantation: Entire liver replacement with a donor's liver is a viable option for individuals who are generally healthy, and the cancer has not spread to other organs. However, the availability of high-quality donor organs is limited.
- Local Therapy:
- Heat Therapy or Ablation: Using electrical current, microwaves, or lasers to heat and destroy cancerous cells. The procedure is guided by imaging, and needles are inserted into the tumor to deliver heat.
- Cold Therapy or Cryoablation: Employing extreme cold temperatures, using a cryoprobe containing liquid nitrogen to freeze and destroy cancerous cells. Ultrasonography guides the procedure.
- Alcohol Injection: Injecting pure alcohol directly into the tumor, either through the skin or during surgery, to induce cell death.
- Guided Chemotherapy or Radiation: Delivering chemotherapy or radiation directly to cancerous cells through a catheter inserted into the liver's blood vessels. This includes chemoembolization and radioembolization.
- Radiotherapy: Using x-ray or proton energy to target cancerous cells, especially when surgery is not feasible. Stereotactic radiotherapy delivers multiple radiation beams simultaneously to a specific point.
- Targeted medication: Utilizing medications designed to target specific weaknesses in cancerous cells, inhibiting disease growth, particularly in advanced stages.
- Immunotherapy: Harnessing the body's immune system to attack cancerous cells. Immunotherapy is often employed in the late stages of cancer.
Complications
Complications associated with Hepatocellular Carcinoma (HCC) include:
- Hepatic Encephalopathy: A serious complication resulting from chronic liver disease or liver failure.
- Vena Porta Thrombosis: The blockage of veins in the liver.
- Ascites: The accumulation of fluid in the abdomen.
- Variceal Bleeding: Bleeding from enlarged veins (varices) in the esophagus or stomach.
- Bilirubin Increase: Elevated levels of bilirubin, a substance that gives color to stool and urine.
- Liver Abscess: A lump filled with pus within the liver.
- Internal Abdominal Bleeding: Potentially life-threatening bleeding within the abdomen.
- Metastasis: The spread of cancerous cells to other body parts, often affecting the lungs, lymph nodes in the abdomen, bones, and adrenal glands.
Prevention
Preventive measures to reduce the risk of Hepatocellular Carcinoma (HCC) include:
- Hepatitis B Vaccination: Getting vaccinated against hepatitis B helps prevent chronic infection, liver cirrhosis, and subsequent liver cancer caused by the hepatitis B virus.
- Antiviral Therapy for Hepatitis B or C: Chronic infections of hepatitis B or C are linked to liver cirrhosis and liver cancer. Antiviral therapy for these infections can significantly reduce the risk of developing HCC.
- Limit Alcohol Consumption
- Maintain Ideal Body Weight
When to see a doctor?
In the early stage of Hepatocellular Carcinoma (HCC), symptoms may not be apparent. If an individual has liver disease or risk factors associated with HCC, it is recommended to undergo routine check-ups, screenings, or monitoring to detect any signs of disease progression. In the presence of symptoms mentioned earlier, seeking immediate medical consultation is crucial.
Looking for more information about other diseases? Click here!
- dr Nadia Opmalina
Hepatocellular carcinoma - Overview - Mayo Clinic. (2022). Retrieved 11 July 2022, from https://www.mayoclinic.org/diseases-conditions/hepatocellular-carcinoma/cdc-20354552
Hepatocellular Carcinoma (HCC): Practice Essentials, Anatomy, Pathophysiology. (2022). Retrieved 11 July 2022, from https://emedicine.medscape.com/article/197319-overview#a1
Liver Cancer Risk Factors. (2022). Retrieved 11 July 2022, from https://www.cancer.org/cancer/liver-cancer/causes-risks-prevention/risk-factors.html
Hepatocellular Carcinoma (HCC): Causes, Symptoms, Treatments & Prognosis. (2022). Retrieved 11 July 2022, from https://my.clevelandclinic.org/health/diseases/21709-hepatocellular-carcinoma-hcc#outlook--prognosis
Asafo-Agyei, K., & Samant, H. (2022). Hepatocellular Carcinoma. Retrieved 11 July 2022, from https://www.ncbi.nlm.nih.gov/books/NBK559177/