Definition
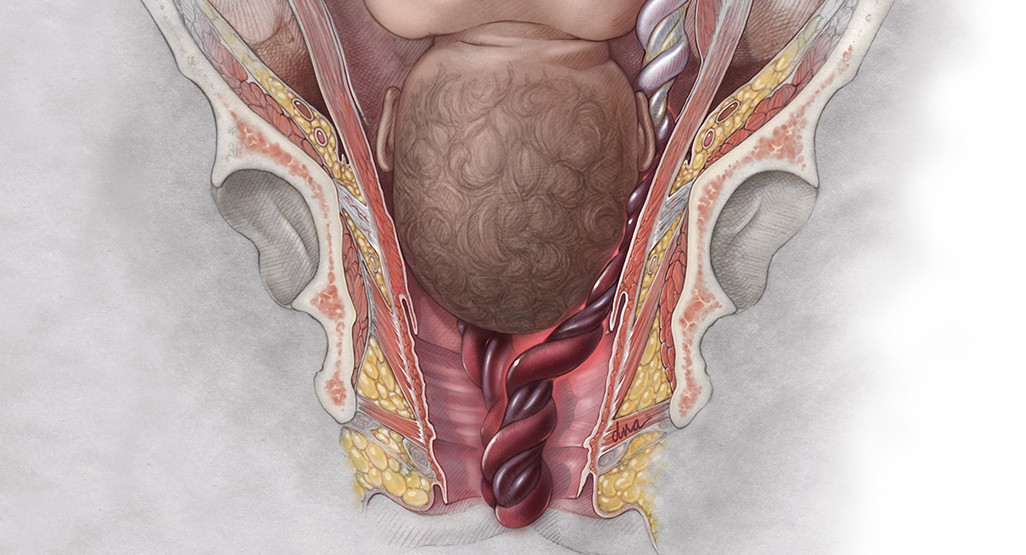
Umbilical cord prolapse is the descent of the umbilical cord through the open cervix so that it passes through the lowest part of the fetus. This condition can occur before or during delivery. This condition needs to be treated immediately. If left untreated, the fetus can press on the umbilical cord and inhibit oxygen flow.
During labor, the baby should be born first, followed by the birth of the umbilical cord and the placenta. However, in rare cases, the umbilical cord descends before the fetus.
The general incidence of umbilical cord prolapse is around 0.1 to 0.6%, or around one in every 1000 births. A study of 307 cases of umbilical cord prolapse showed that 7% of babies died from this condition.
Causes
The umbilical cord is a flexible tube that connects the fetus to the mother. It is the source of life for the fetus because it functions as a connection between the fetus and the mother's placenta. The umbilical cord consists of three blood vessels: two arteries and one vein. These blood vessels deliver oxygen and nutrients to the baby and carry waste products from the baby's metabolism.
Common causes of umbilical cord prolapse include:
- Premature rupture of the amniotic membrane
- Premature or premature labor
- Multiple pregnancy (twins, triplets)
- Abnormalities in the position of the fetus, for example a breech fetus
- Very active fetus
There are three types of umbilical cord prolapse, namely:
- Umbilical cord prolapse. The umbilical cord descends through the cervix to the vagina after the amniotic membranes rupture and before the baby enters the birth canal.
- Umbilical cord presentation. Part of the umbilical cord moves into the space between the baby and the amniotic membranes that are still intact.
- Hidden umbilical cord prolapse. The umbilical cord is located next to the baby in the birth canal but is not detected during the doctor's examination.
Risk Factor
Several factors increase the risk of umbilical cord prolapse, namely:
- Pregnancy with a breech fetus, with the lowest part of the fetus being the legs or buttocks
- Gender of baby boy
- Multiple pregnancy
- Premature birth
- Babies with low birth weight
- Rupture of the amniotic membranes before 37 weeks of gestation
- History of amniotic sac rupture or aminotomy procedure
- Use of a cervical ripening balloon to open the cervix
- History of fetal blood sampling, which is usually done to check for congenital defects
Symptoms
Most umbilical cord prolapse occurs shortly after the membranes rupture. One study estimated that 57% of prolapses occurred within 5 minutes of the membranes rupture and 67% occurred within 1 hour of the rupture.
If you are at home, the most common symptom of umbilical cord prolapse is that you feel the umbilical cord in your vagina after your water breaks.
If you are in the hospital, a doctor or midwife can detect umbilical cord prolapse when performing a pelvic examination and feeling for the umbilical cord. In addition, umbilical cord prolapse can be recognized if the fetus has an abnormal heartbeat.
Diagnosis
Umbilical cord prolapse can be diagnosed by looking or feeling the prolapsed umbilical cord during a pelvic examination. You may also be able to feel the umbilical cord in your vagina.
In some women, the only sign of umbilical cord prolapse is a decrease in fetal heart rate (bradycardia), which is less than 120 beats per minute. This occurs in 67% of cases of umbilical cord prolapse. The umbilical cord is compressed and stretched, slowing blood flow to the baby and causing a sudden decrease or change in the fetal heart rate.
Management
Umbilical cord prolapse is an emergency in obstetrics. If the umbilical cord has come out of the vagina, the baby needs to be born as soon as possible. The time between diagnosis and the baby's birth should be less than 30 minutes. Meanwhile, if the mother is still in the first or early second stage of labor, a cesarean section will be recommended. However, in some women, depending on the situation, normal delivery will be quicker and an option.
While waiting for surgery, the mother will be positioned so that her knees meet her chest to reduce pressure on the umbilical cord. The doctor can also insert a hand or finger into the vagina and gently lift the part of the baby that is pressing on the umbilical cord. This will reduce the risk of decreasing fetal oxygen.
If it is still some time before delivery, the doctor may fill your bladder with an IV solution to help relieve pressure on the umbilical cord.
Complications
Umbilical cord prolapse is a rare condition but is a potentially fatal emergency in obstetrics. During labor, the descending umbilical cord can be compressed between the fetus and the cervix. This will result in cutting off oxygen flow to the fetus, which can lead to:
- Premature birth
- Congenital malformations or birth defects
- Newborn respiratory problems
- Brain damage due to lack of oxygen (encephalopathy) and cerebral palsy
- Newborn death or stillbirth
Delays in transport to the hospital are a significant factor contributing to these complications. When umbilical cord prolapse occurs outside the hospital, the risk of infant death is 18 times higher than umbilical cord prolapse that occurs inside the hospital.
Prevention
Umbilical cord prolapse cannot be prevented or predicted. The umbilical cord will experience a lot of movement during pregnancy, so ultrasound cannot predict the presence of umbilical cord prolapse. This condition can also occur in women without certain risk factors.
However, your doctor may recommend being hospitalized if you are at high risk. The team of doctors can respond quickly when you start labor.
When to See a Doctor?
If you experience signs or symptoms of umbilical cord prolapse and you are not in the hospital, call the emergency number immediately. While you wait for the ambulance, you may be instructed to maintain a position in which you rest on your hands and knees, place your head on the floor, and lift your pelvis. This will reduce pressure on the umbilical cord.
Looking for more information about other diseases? Click here!
- dr. Alvidiani Agustina Damanik
Umbilical Cord Prolapse: Causes, Diagnosis & Management. (2022). Retrieved 4 October 2022, from https://my.clevelandclinic.org/health/diseases/12345-umbilical-cord-prolapse
What Is Umbilical Cord Prolapse?. (2022). Retrieved 4 October 2022, from https://www.webmd.com/baby/what-is-umbilical-cord-prolapse
Umbilical Cord Prolapse: Causes, Symptoms, Diagnosis, and Treatment. (2022). Retrieved 4 October 2022, from https://www.healthline.com/health/pregnancy/umbilical-cord-prolapse#bottom-line