Definition
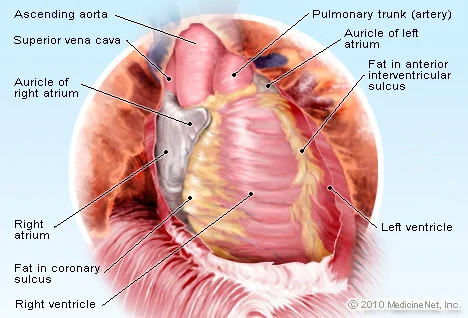
Pericarditis is the inflammation of the pericardium. The pericardium is a thin, fluid-filled sac that covers the outer surface of the heart, lubricates it, protects it from infection and malignancy, and holds the heart to the chest wall. The pericardium also prevents the heart from expanding too much when blood volume rises, allowing the heart to function properly. The pericardium consists of several layers, including:
- Visceral pericardium is the inner layer that covers the entire surface of the heart
- The middle fluid layer prevents friction between the visceral pericardium and the parietal pericardium
- The parietal pericardium is the outer layer made of fibrous connective tissue
Pericarditis often causes a sharp onset of chest pain. Chest pain occurs when the irritated layers of the pericardium rub against each other. Pericarditis is usually acute, meaning it develops suddenly and can last up to several months. The condition usually resolves after 3 months, but sometimes symptoms may persist for years.
When you have pericarditis, the lining around your heart will become red and swollen. Sometimes there can be additional fluid in the space between the layers of the pericardium, called pericardial effusion. Pericarditis can affect anyone, but it is most common in men aged 16 to 65 years.
Causes
The cause of pericarditis is frequently difficult to determine, and in some cases, no cause can be found, resulting in idiopathic pericarditis. Some causes of pericarditis may include:
- An immune system response following heart damage from a heart attack or heart surgery (Dressler's syndrome, also known as post-heart attack syndrome or post-heart injury syndrome)
- Viral infections, such as COVID-19, gastrointestinal viruses, HIV
- Bacterial infections, such as Tuberculosis
- Fungal infections
- Parasitic infections
- Inflammatory diseases, including lupus, scleroderma, ankylosing spondylitis, inflammatory bowel disease, and rheumatoid arthritis
- Injury to the heart or chest
- Other chronic health conditions, including kidney failure and cancer
- Genetic diseases such as Familial Mediterranean Fever (FMF)
- Medications that can suppress the immune system
- Effects of radiation treatment
- Metabolic disorders, such as gout and hypothyroidism (low thyroid hormone levels)
Risk factor
Pericarditis is more likely to develop following a heart attack, heart surgery (post-cardiotomy syndrome), radiation therapy, or percutaneous procedures such as cardiac catheterization or radiofrequency ablation (RFA). In these cases, pericardial inflammation is most likely caused by an error in the body's response to the procedure or condition. Pericarditis symptoms may not appear for several weeks after bypass surgery.
Symptoms
The most common symptom of pericarditis is chest pain. Chest pain symptoms are typically sharp or stabbing. However, in some cases, the chest pain may manifest as a dull ache, aching sensation, or pressure. Pericarditis pain is usually felt behind the breastbone or on the left side of the chest. Characteristics of pericarditis chest pain may include pain that:
- Spreads to the left shoulder and neck
- Gets worse when coughing, lying down, or taking a deep breath
- Gets better when sitting or leaning forward
Other signs and symptoms of pericarditis may include:
- Dry cough
- Fatigue or a general feeling of weakness or pain
- Swelling in the feet, legs, and ankles
- Mild fever
- Rapid heartbeat (heart palpitations)
- Shortness of breath when lying down
- Swelling of the abdomen
Specific symptoms may vary depending on the type of pericarditis. Pericarditis can be divided into several categories based on the pattern of symptoms and the duration of the symptoms, including:
- Acute pericarditis occurs suddenly but does not last more than three weeks. There is a possibility of recurring episodes. It can be difficult to distinguish acute pericarditis from pain caused by a heart attack
- Recurrent pericarditis occurs about four to six weeks after an episode of acute pericarditis with no symptoms in between
- Incessant pericarditis lasts about four to six weeks but less than three months. Symptoms occur continuously
- Chronic constrictive pericarditis usually develops slowly and lasts more than three months
Diagnosis
When diagnosing pericarditis, the doctor will first interview with you, asking you about your symptoms, how long they have been present, the characteristics of your chest pain, and any risk factors that may contribute to the onset of pericarditis.
Next, the doctor will perform a physical examination. The doctor will use a stethoscope to listen to your heartbeat. Pericarditis is characterized by a sound known as pericardial friction rub, which occurs when the two layers of the sac surrounding the heart (pericardium) rub against each other.
Blood tests are also usually done to check for signs of heart attack, inflammation and infection. Other supporting tests used to diagnose pericarditis may include:
- An electrocardiogram (ECG) is an examination that can be done quickly and painlessly to record electrical signals in the heart
- A chest X-ray can show changes in the size and shape of the heart to help detect an enlarged heart
- A sound wave-assisted echocardiogram (ultrasound) creates images of the heart in motion to show how well the heart is pumping blood and if there is fluid buildup in the tissues around the heart
- A CT scan of the heart can be used to look for thickening of the heart which may be a sign of constrictive pericarditis
- A cardiac MRI uses magnetic fields and radio waves to create cross-sectional images of the heart to look for thickening, inflammation, or other changes in the thin tissue around the heart
Management
Treatment and therapy for pericarditis will depend on the cause and severity of the symptoms. Mild pericarditis may resolve without treatment. Some of the management options for pericarditis include:
- Medications, to reduce inflammation and swelling, include:
- Pain medications, such as aspirin or ibuprofen
- Colchicine. This medication can reduce inflammation in the body and is used to treat acute pericarditis or if symptoms tend to recur
- Corticosteroids, which include drugs to fight inflammation. Corticosteroids such as prednisone may be prescribed if symptoms of pericarditis do not improve with other medications, or if symptoms keep returning
- If the pericarditis is caused by a bacterial infection, treatment may include antibiotics and drainage if necessary
- Surgery or other procedures
If pericarditis causes fluid buildup around the heart, surgery or other procedures may be needed to drain the fluid, such as:
- Pericardiocentesis is a procedure when a sterile needle or small tube (catheter) is used to remove and drain excess fluid from the pericardial cavity
- Removal of the pericardium (pericardiectomy). The entire pericardium may need to be removed if the sac surrounding the heart is permanently stiff due to constrictive pericarditis
Complications
If pericarditis is left untreated, the condition may worsen and lead to complications, such as:
- Cardiac tamponade: When too much fluid accumulates in the pericardium, it can increase pressure on the heart and prevent it from filling with blood. This condition can lead to a fatal drop in blood pressure if left untreated
- Constrictive pericarditis: will involve permanent thickening and scarring of the pericardium. This hardens the tissue and prevents the heart from functioning properly, potentially resulting in swelling of the feet and legs as well as shortness of breath.
Prevention
There is no specific prevention against pericarditis. However, taking the following steps to prevent infection can help reduce the risk of heart inflammation:
- Avoid people suffering from viral or flu-like illnesses until they recover
- Maintain a good hygiene lifestyle. Washing your hands regularly can help prevent the spread of disease
- Get recommended vaccines, such as against COVID-19, rubella and influenza
When to see a doctor?
Consult with a doctor if you experience symptoms that point to pericarditis.
Looking for more information about other diseases? Click here!
- dr Anita Larasati Priyono
Beckerman, James. Heart Disease and Pericarditis. (2020). Retrieved 30 Mei 2022, from https://www.webmd.com/heart-disease/guide/heart-disease-pericardial-disease-percarditis
Hecht, Marjorie. All About Pericarditis. (2022). Retrieved 30 Mei 2022, from https://www.healthline.com/health/pericarditis
Newman, Tim. Everything You Need to Know About Pericarditis. (2018). Retrieved 30 Mei 2022, from https://www.medicalnewstoday.com/articles/193320
Pericarditis. (2022). Retrieved 30 Mei 2022, from https://www.mayoclinic.org/diseases-conditions/pericarditis/symptoms-causes/syc-20352510
Pericarditis. (2019). Retrieved 30 Mei 2022, from https://my.clevelandclinic.org/health/diseases/17353-pericarditis
Pericarditis. (2021). Retrieved 30 Mei 2022, from https://www.healthdirect.gov.au/pericarditis
Wedro, Benjamin. Pericarditis. Retrieved 30 Mei 2022, from https://www.medicinenet.com/pericarditis/article.htm
What is Pericarditis?. (2021). Retrieved 30 Mei 2022, from https://www.heart.org/en/health-topics/pericarditis/what-is-pericarditis