Definition
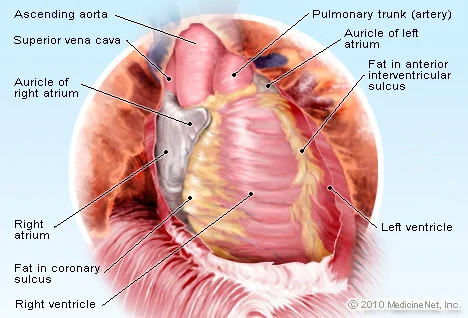
The heart's wall is generally composed of three layers: the innermost layer or endocardium, the middle layer or myocardium, and the outermost layer or pericardium.
The endocardium is the thinnest layer. The myocardium, located in the middle of the heart wall, is the thickest layer and consists of specialized muscles found only in the heart.
In addition to the endocardium and myocardium, there is the pericardium, the outermost layer that covers the entire surface of the heart. This layer is very thin and contains fluid that reduces friction during the heart's contractions.
The heart wall can become inflamed. If the infection affects the innermost layer or endocardium, the condition is known as endocarditis. Inflammation of the middle layer of the myocardium is called myocarditis. If the outermost layer is inflamed, the condition is termed pericarditis.
Causes
Several pathogens can cause inflammation of the heart wall, with viruses and bacteria being the most common culprits. Viruses frequently responsible for inflammation include COVID-19, hepatitis B and C, and herpes simplex virus. Bacteria that can lead to heart wall inflammation include Staphylococcus, Streptococcus, and bacteria responsible for diphtheria.
In addition to viruses and bacteria, heart wall inflammation may also result from parasitic infections, fungi, and exposure to certain chemicals or radiation.
Risk factor
Factors that can increase the risk of heart wall inflammation include:
- History of drug abuse involving needle use
- Poor dental health
- Age over 60
- Certain medical conditions, such as immune system disorders, viral and bacterial infections, or side effects from medications like antiepileptics
- Accidents causing injury
Symptoms
Symptoms can vary depending on the location of the inflammation. Generally, inflammation of the heart wall will cause chest pain, which can occur both at rest and during activity. The pain may feel like a sharp stabbing and can worsen with coughing or lying down.
Other symptoms include muscle and joint pain, fatigue, shortness of breath, and swelling in the abdomen, ankles, and legs due to fluid accumulation.
Further symptoms vary based on the affected layer of the heart wall. If the endocardium is inflamed, symptoms may appear suddenly or gradually and include:
- Night sweats
- Red spots on the palms or soles
- Unexplained weight loss
If the myocardium is inflamed, symptoms include:
- Rapid or irregular heartbeat
- Fluid accumulation in the legs and ankles
- Easy fatigue
Additional symptoms may depend on the underlying cause, such as headaches, body aches, joint pain, fever, sore throat, or diarrhea.
If the pericardium is inflamed, symptoms may include:
- Pain in the neck, back, and shoulders
- Dry cough
- Easy fatigue or anxiety
Often, symptoms are accompanied by signs of an underlying infection causing the inflammation, such as fever, chills, joint pain, and headaches.
Diagnosis
To diagnose the condition, the doctor will ask about your symptoms and medical history and perform a physical examination to detect abnormalities related to heart wall inflammation. Additional diagnostic tests may be required, including:
- Blood culture: Identifies specific pathogens causing the inflammation so appropriate treatment can be prescribed.
- Complete blood count: Determines the number of blood cells. An increase in white blood cells may indicate infection.
- Echocardiogram: Uses sound waves to produce images of the heart, helping to identify abnormalities.
- Electrocardiogram (EKG): Measures electrical activity of the heart to detect irregularities.
- Chest X-ray: Helps visualize the condition of the lungs and heart using X-ray radiation.
- Cardiac MRI: Provides detailed images of the heart's size, shape, and structure and detects inflammation, particularly in pericarditis and myocarditis.
- Cardiac catheterization: Involves inserting a catheter through blood vessels to the heart to detect abnormalities.
Management
Treatment aims to eliminate the underlying infection and alleviate symptoms. If inflammation is caused by bacterial infection, antibiotics specific to the bacteria will be prescribed.
Pain relief medications will address discomfort from inflammation and anti-inflammatory drugs will be used to reduce inflammation in the heart. Heart medications will be prescribed according to the symptoms experienced.
For fluid accumulation in the abdomen, legs, or ankles, diuretics will be administered. If medication is insufficient, drainage procedures or surgery may be necessary.
Complications
Heart wall inflammation generally resolves without permanent complications, but in some cases, permanent heart muscle damage can occur, leading to heart failure. If untreated, this condition can result in ineffective blood pumping.
Ineffective blood pumping can cause blood clots, which may block blood vessels and lead to heart attacks or strokes. Additionally, heart muscle damage can result in arrhythmias.
The most severe risk is sudden death, typically due to severe arrhythmias causing the heart to stop.
Prevention
Currently, there are no specific preventive measures. However, general infection prevention practices, such as maintaining personal and environmental hygiene, hand washing, wearing masks, and vaccinations, are recommended.
When to see a doctor?
Symptoms of heart wall inflammation can resemble those of a heart attack. If you experience unexplained chest pain and shortness of breath, seek emergency medical care immediately.
Looking for more information about other diseases? Click here!
- dr Nadia Opmalina
(MayoClinic, 2021) Myocarditis diakses tanggal 10 April 2022, dari https://www.mayoclinic.org/diseases-conditions/myocarditis/symptoms-causes/syc-20352539
(MayoClinic, 2021) Endocarditis diakses tanggal 10 April 2022, dari https://www.mayoclinic.org/diseases-conditions/endocarditis/symptoms-causes/syc-20352576
(ClevelandClinic, 2021) Pericarditis diakses tanggal 10 April 2022, dari https://my.clevelandclinic.org/health/diseases/17353-pericarditis
(MayoClinic, 2021) Pericarditis diakses tanggal 10 April 2022, dari https://www.mayoclinic.org/diseases-conditions/pericarditis/diagnosis-treatment/drc-20352514