Definition
Microcornea is an abnormality in the cornea size (the thin, clear layer at the front of the eyeball), defined as less than 9.5-10 mm in horizontal diameter in newborns and less than 10-11 mm in adults. The term microcornea is used for small corneas with normal-sized eyeballs. However, some use the term to describe small corneas accompanied by nanophthalmos or microphthalmos. Nanophthalmos refers to an abnormally small eyeball with a regular structure, while microphthalmos is a small, irregular eyeball.
Microcornea is a rare disorder, often without a specific inheritance pattern. However, certain inheritance patterns, especially those associated with syndromes (disorders with multiple characteristics), have been identified. For instance, an autosomal dominant inheritance pattern is found in families with congenital cataract-microcornea syndrome (an inherited disorder involving cataracts and microcornea).
Causes
Microcornea is a congenital disorder that may be related to impaired growth of the fetal cornea in the fifth month of pregnancy, or excessive growth of the forepart of the optic cup during eye development. This can limit the space for the cornea to develop.
There are rare cases where microcornea associated with microphthalmia is caused by congenital cytomegalovirus infection (in utero). In microcornea associated with syndromes, gene mutations have been found.
Risk Factor
There has been limited research on risk factors for microcornea. However, similar to other congenital disorders, potential risk factors include:
- Genetic factors
- Environmental factors, such as exposure to chemicals, drugs, alcohol, cigarettes, and radiation during pregnancy
- Infections during pregnancy
- Maternal malnutrition during pregnancy
Symptoms
Size abnormalities in the cornea can occur by itself (isolated microcornea) or in conjunction with abnormalities in other parts of the eye, with or without any structural ocular disorders. Eyes with microcornea tend to be hyperopia (farsighted) due to the relatively flat cornea, although other refractive disorders are also possible to occur.
Approximately 20% of patients with microcornea develop open-angle glaucoma later in life, while the remainder may be predisposed to angle-closure glaucoma due to the relatively shallow anterior chambers in microcornea patients. Additionally, eye abnormalities or disorders in other body parts can be related to microcornea.
Diagnosis
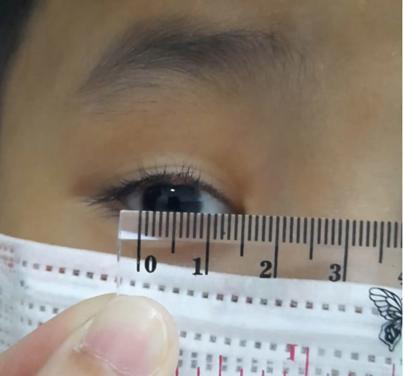
The diagnosis of microcornea involves measuring the horizontal diameter of the cornea using tools such as a ruler, caliper, topography machine, or biometry. Slit-lamp examination, gonioscopy, and ocular ultrasound are used to differentiate simple microcornea from nanophthalmos and microphthalmos.
In cases where microcornea is part of a syndrome, examinations are conducted on other body parts to detect or rule out other congenital abnormalities.
Management
Therapy for microcornea is supportive and aims to prevent complications. These therapies include refractive correction and glaucoma treatment. Corneal transplantation may be considered if both corneas are cloudy; however, the surgical process and postoperative period are challenging due to potential complications such as glaucoma.
If the patient has one normal, clear cornea, corneal surgeons often avoid transplantation due to high risks of complications and amblyopia (lazy eye). Pediatric ophthalmologists and cornea specialists collaborate to decide on the appropriate course of action, assessing the risk of amblyopia and other ocular disorders associated with microcornea. Covering the healthy eye with an eye patch can be an option to train and strengthen the eye with microcornea.
Complications
In microcornea, the smaller diameter of the cornea, coupled with a normally sized lens, causes the iris to push forward, closing the angle of the anterior chamber. This can impair the development of the anterior chamber angle and may lead to angle-closure glaucoma as the anterior chamber is obstructed by the iris. Glaucoma can also be a complication after cataract surgery in patients with microcornea accompanied by cataracts.
Prevention
Steps to prevent congenital abnormalities, including microcornea, involve:
- Ensuring good and balanced nutrition for mothers and teenage girls.
- Adequate intake of vitamins and minerals, especially folic acid, for mothers and adolescent girls.
- Avoiding hazardous exposures during pregnancy, such as chemicals, certain drugs, alcohol, cigarettes, and radiation.
- Pregnant women should avoid traveling to areas experiencing outbreaks of infectious diseases related to congenital abnormalities.
- Diabetic pregnant women should regularly control their sugar levels, maintain an ideal body weight, and follow an appropriate diet.
- Vaccination, particularly the rubella vaccine, for children and women.
- Screening for infections during pregnancy, such as rubella, varicella, and syphilis.
When to See a Doctor?
If you notice that one of your newborn's eyes looks different from the other eye or from the normal eye of another baby, consult an eye doctor immediately.
Looking for more information about other diseases? Click here!
- dr Ayu Munawaroh, MKK
Yanoff M, Duker JS. 2014 Ophthalmology: Congenital Corneal Anomalies. 4th ed. US: Saunders Elsevier. p. 173.
Microcornea. Eye Rounds.Org. Retrieved 22 November 2021, from https://webeye.ophth.uiowa.edu/eyeforum/atlas/pages/microcornea/index.htm.
Lee H. 2014. Microcornea. Encyclopedia of Ophthalmology (pp.1-3). doi: 10.1007/978-3-642-35951-4_823-1
Lee WB. 2014. Can microcornea be treated?. American Academy of Ophthalmology. Retrieved 22 November 2021, from https://www.aao.org/eye-health/ask-ophthalmologist-q/can-microcornea-be-treated.