Definisi
Dorsal root syndrome (sindrom radiks posterior) adalah kumpulan gejala yang disebabkan oleh adanya kerusakan pada radiks posterior. Radiks posterior adalah struktur dari sel saraf yang berfungsi untuk menghantarkan sensasi sensorik dari reseptor sensori pada indera manusia ke otak. Jika terjadi gangguan pada radiks posterior, seseorang akan mengalami gangguan dalam merasakan nyeri, mengetahui posisi tubuh, dan merasakan panas atau dingin secara sebagian atau keseluruhan. Kondisi ini dapat disebabkan oleh berbagai hal mulai dari genetik, infeksi, gangguan imun, intoksikasi obat dan lainnya.
Penyebab
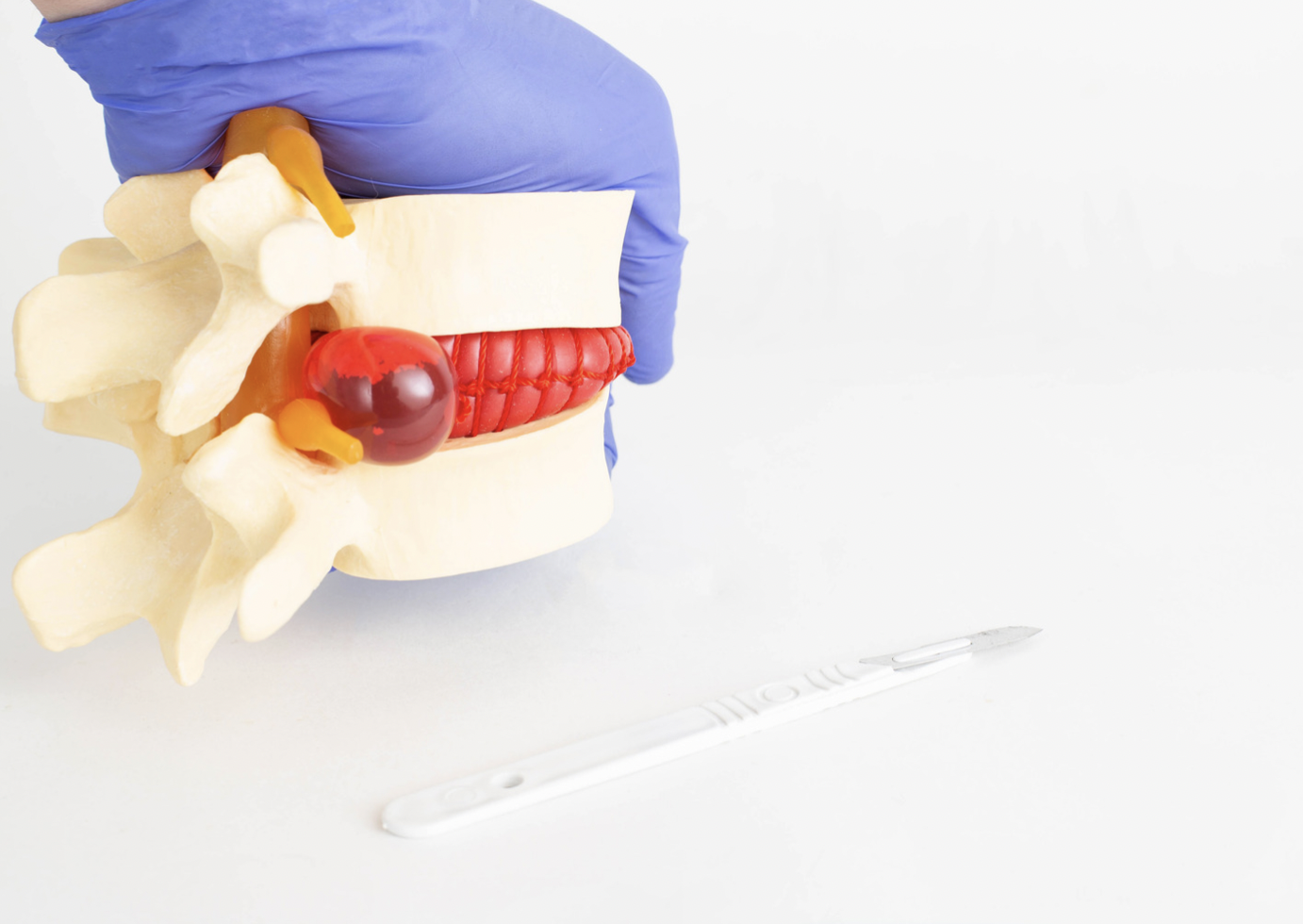
Untuk dapat menghantarkan dan memproses informasi, tubuh kita memiliki dua struktur penting, yaitu radiks anterior dan radiks posterior. Kedua struktur ini berhubungan langsung dengan sumsum tulang belakang. Kedua struktur ini memiliki fungsi yang berbeda. Radiks anterior berfungsi untuk menghantarkan sinyal dari otak ke organ target, sedangkan radiks posterior berfungsi untuk menghantarkan sinyal dari indera tubuh ke otak. Stimulus sensori akan ditangkap oleh reseptor pada indera manusia dan dihantarkan melalui saraf. Saraf tersebut akan berkumpul menjadi radiks posterior. Setelah dihantarkan melalui radiks posterior, informasi akan sampai di sumsum tulang belakang, diklasifikasikan berdasarkan jenisnya, dan dikirim ke otak melalui jalur yang berbeda. Informasi tersebut akan diproses oleh otak sehingga manusia dapat merasakan sensasi nyeri, dingin, panas, dan sentuhan. Selain itu, radiks posterior juga bertanggung jawab untuk menghantarkan informasi berkaitan dengan posisi tubuh, regangan otot, dan getaran.
Radiks posterior lebih sensitif terhadap kerusakan karena struktur barrier atau batasan yang lebih tipis, sehingga lebih mudah terpapar toksin, proses peradangan, dan infeksi. Jika terjadi infeksi atau keganasan pada tubuh, sel imun akan berusaha untuk mengatasi kondisi tersebut melalui proses peradangan. Dampak dari peradangan, selain dapat meredakan infeksi, juga dapat merusak organ pada tubuh, termasuk radiks posterior. Sel imun seperti sel limfosit T, limfosit B, dan makrofag akan merusak lapisan myelin pada radiks posterior sehingga menyebabkan kerusakan. Hal lain seperti proses penuaan, penekanan mekanis pada radiks posterior, kondisi autoimun, dan berkurangnya suplai darah ke radiks posterior juga dapat menyebabkan kerusakan pada struktur ini. Jika terjadi kerusakan, seseorang akan mengalami kumpulan gejala yang disebut dorsal root syndrome.
Gangguan pada radiks posterior disebabkan oleh:
- Kondisi autoimun, seperti sarkoidosis, sindrom Sjörgen, systemic lupus erythematosus (SLE)
- Proses degeneratif (penuaan)
- Cedera tulang belakang
- Penekanan pada saraf dan pembuluh darah yang menyebabkan penurunan suplai darah
- Infeksi seperti sifilis, lepra, hepatitis C
- Penyakit metabolik seperti diabetes, hiperlipidemia
- Zat toksin seperti alkohol
- Kanker. Salah satu antibodi yang berperan dalam kerusakan radiks posterior adalah Antibodi anti-Hu yang ditemukan pada penderita kanker paru, prostat, ovarium, dan payudara
Faktor Risiko
Faktor yang meningkatkan risiko seseorang mengalami dorsal root syndrome, antara lain:
- Usia tua, proses degeneratif dapat merusak radiks posterior
- Mengalami cedera tulang belakang
- Memiliki kondisi autoimun
- Mengalami kanker
- Mengidap HIV/AIDS
- Dalam terapi kanker (cisplatin)
- Defisiensi/kekurangan vitamin B6
- Mengonsumsi alkohol
Gejala
Gejala dari dorsal root syndrome antara lain:
- Tidak dapat atau berkurangnya kemampuan untuk merasakan stimulus sensori, seperti nyeri, suhu, posisi tubuh, dan getaran
- Kesulitan untuk mempertahankan posisi (ataksia)
- Penurunan refleks tubuh
- Tanda otonom, seperti hipotensi ortostatik, gangguan pencernaan, dan gangguan ereksi
- Rasa kesemutan dan sensasi tersengat listrik (kesetrum)
- Rasa baal, terutama pada pasien diabetes
Diagnosis
Dokter akan menanyakan mengenai keluhan Anda dan riwayat penyakit sebelumnya yang merupakan faktor risiko dari dorsal root syndrome.
Diagnosis dari kondisi ini dapat dilakukan dengan pemeriksaan neurologis (saraf). Uji sensibilitas kulit dapat dilakukan untuk menilai kemampuan merasakan sensasi raba, getar, nyeri, dan proprioseptif (posisi tubuh). Uji sensibilitas dapat digunakan untuk memperkirakan letak kerusakan terjadi. Uji dilakukan dengan membandingkan antara sisi kanan dan kiri tubuh. Jika terdapat kerusakan pada kedua sisi, uji sensibilitas lebih sulit untuk dilakukan. Pada pemeriksaan motorik umumnya tidak ditemukan adanya kelemahan pada anggota gerak, namun relfeks tubuh dapat berkurang.
Terdapat beberapa modalitas pemeriksaan penunjang yang dapat digunakan untuk menegakkan diagnosis, antara lain:
- Elektromiografi (EMG). Pada pemeriksaan EMG, kondisi neuropati dapat menunjukkan berkurangnya aksi potensial pada saraf sensori. Namun, pemeriksaan ini juga dapat memberikan hasil normal.
- Biopsi kulit. Pemeriksaan ini merupakan baku emas dalam penegakan dorsal root syndrome. Sensitivitas dan spesifisitas pemeriksaan ini untuk menegakkan diagnosis adalah 90% dan 97%. Lokasi pengambilan sampel adalah kaki, sekitar 10 cm dari mata kaki. Pada dorsal root syndrome, didapatkan berkurangnya jumlah sel saraf, kumpulan sel imun (nodule of nageotte), dan degenerasi sel ganglion.
- Pemeriksaan radiologi. Pemeriksaan radiologi seperti MRI dapat dilakukan untuk mengevaluasi anatomi dari sumsum tulang belakang, terutama pada individu dengan keluhan yang sudah lama.
Tata laksana
Secara umum, belum ada panduan khusus untuk menangani kondisi ini. Beberapa studi menunjukkan obat-obatan seperti anti-kejang, antidepresan serotonin-norepinephrine reuptake inhibitor (SNRI), antidepresan trisiklik, opioid, dan injeksi botox dapat membantu mengurangi gejala dibandingkan plasebo. Namun, hal ini masih membutuhkan penelitian lebih lanjut.
Pengobatan dari dorsal root syndrome lebih berfokus pada pengobatan gejala. Jika terdapat nyeri, dokter Anda akan memberikan antinyeri seperti parasetamol dan obat anti-inflamasi non-steroid (OAINS) seperti ibuprofen. Antidepresan dan anti-kejang (antikonvulsan) dapat membantu pasien untuk menoleransi nyeri.
Pengobatan lainnya yang dapat digunakan adalah dengan akupuntur, teknik relaksasi, dan terapi panas atau dingin. Fisioterapi dapat membantu mengatasi kondisi ataksia.
Komplikasi
Komplikasi dari dorsal root syndrome yang tidak ditangani dengan baik, antara lain:
- Luka. Kurangnya sensasi dan kemampuan tubuh untuk mendeteksi stimulus berbahaya, seperti suhu panas atau tajam, dapat menyebabkan seseorang terluka.
- Infeksi. Karena individu dengan dorsal root syndrome tidak menyadari bahwa dirinya memiliki luka, luka tersebut dapat dibiarkan dan mengalami infeksi lebih lanjut. Infeksi ini dapat menyebabkan gangren (jaringan tubuh mengalami nekrosis/mati) yang menyebabkan amputasi hingga sepsis (komplikasi akibat infeksi) yang mengancam nyawa.
- Jatuh. Pasien dorsal root syndrome dapat mengalami gangguan dalam memproses posisi tubuhnya (fungsi proprioseptif) sehingga lebih mudah terjatuh, terutama untuk lansia.
Luaran dari dorsal root syndrome bervariasi bergantung pada derajat kerusakan saraf dan penyebab dari kondisi ini. Contohnya, pasien yang mengalami dorsal root syndrome karena gula darah tidak terkontrol dapat mengalami perbaikan jika gula darahnya kembali dikontrol. Umumnya, sensasi yang pertama kali kembali adalah nyeri dan temperatur.
Pencegahan
- Kontrol kondisi medis Anda. Dengan menjaga gula darah tetap dalam batas normal dan mengonsumsi obat-obatan untuk autoimun, Anda dapat mengurangi risiko mengalami dorsal root syndrome.
- Gunakan pelindung kaki dan sarung tangan. Untuk mencegah komplikasi dari dorsal root syndrome, Anda dapat menghindari luka dengan menggunakan pelindung. Anda juga dapat memeriksa kaki serta tangan Anda setiap hari untuk memastikan tidak ada luka.
- Memperbaiki gaya hidup. Dengan mengonsumsi makanan gizi seimbang dan melakukan aktivitas fisik, Anda dapat menjaga kesehatan saraf Anda dan mencegah kondisi yang dapat menyebabkan dorsal root syndrome, seperti diabetes dan defisiensi/kekurangan vitamin B6.
- Kurangi konsumsi alkohol. Alkohol merupakan salah satu faktor risiko dari dorsal root syndrome. Mengurangi atau menghentikan konsumsi alkohol dapat mencegah kondisi ini.
Kapan Harus Ke Dokter?
Jika Anda mengalami gejala kehilangan kemampuan untuk merasakan stimulus sensoris dan memiliki kondisi medis lain yang dapat menyebabkan dorsal root syndrome atau memiliki riwayat keluarga dengan dorsal root syndrome, lakukan pemeriksaan ke fasilitas kesehatan terdekat.
- dr Nadia Opmalina
Gomatos EL, Rehman A. Sensory Neuropathy. [Updated 2021 Jul 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559020/
Ahimsadasan N, Reddy V, Kumar A. Neuroanatomy, Dorsal Root Ganglion. [Updated 2021 Sep 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532291/
Tamasse J. (2016). Dorsal Root Syndrome. Available from: https://med.unhas.ac.id/kedokteran/wp-content/uploads/2016/09/Bahan-Ajar-10_Dorsal-Root-Syndrome.pdf
Gwathmey KG, Pearson KT. Diagnosis and management of sensory polyneuropathy. BMJ. 2019 May 8;365:l1108. doi: 10.1136/bmj.l1108. PMID: 31068323.



/62d24491836c4.jpg)
/630206d67d517.jpg)
/6302127e4476f.jpg)





