Definisi
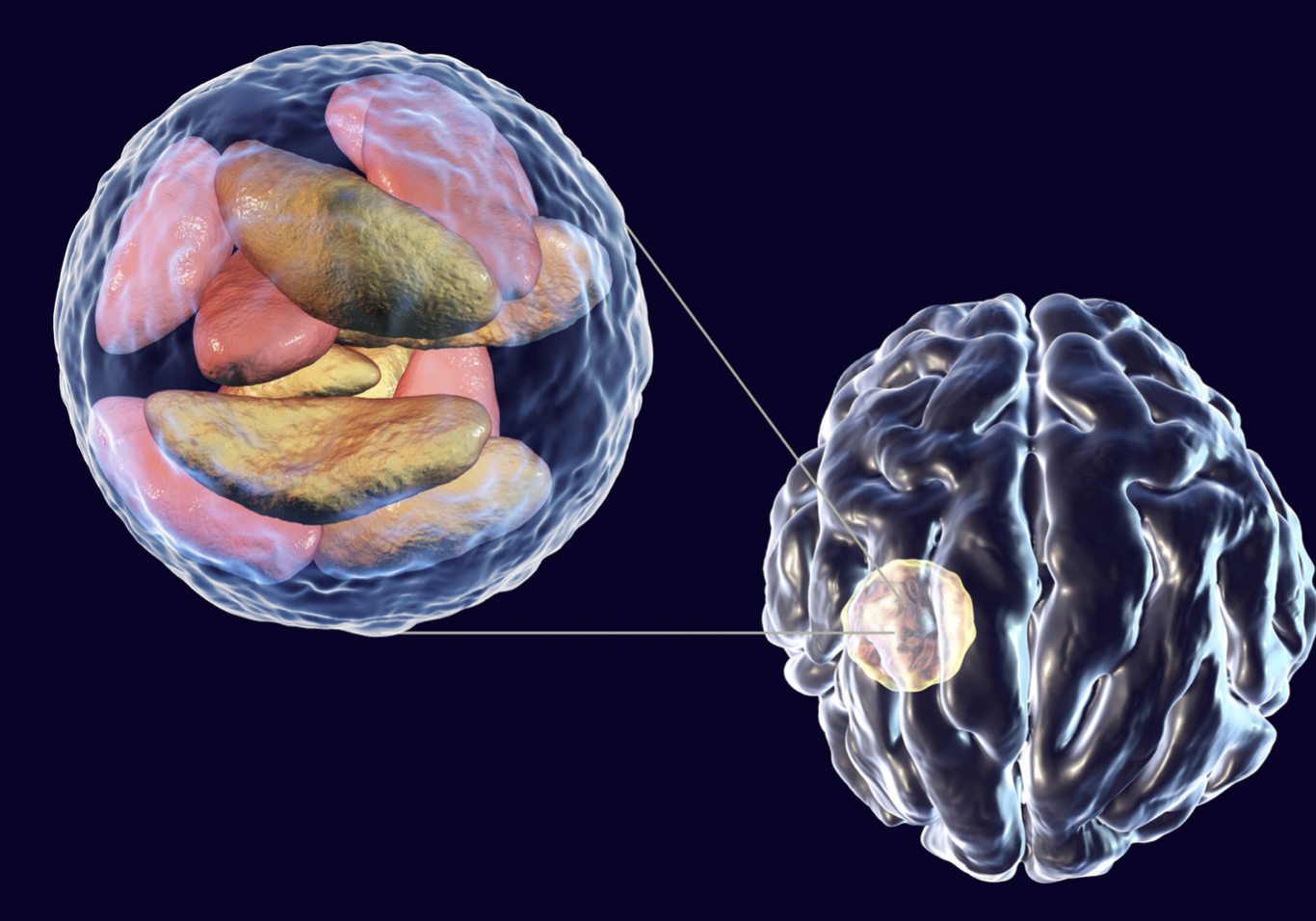
Toxoplasmosis serebri atau disebut dengan neurotoxoplasmosis adalah infeksi otak yang disebabkan oleh parasit Toxoplasma gondii. Infeksi toksoplasma disebabkan oleh konsumsi daging yang kurang matang, terpapar kotoran kucing yang mengandung parasit, dan penularan dari ibu ke anak selama kehamilan. Toksoplasmosis umumnya hanya menyebabkan gejala ringan pada populasi dengan imunitas baik. Namun, pada populasi rentan, seperti penyandang HIV/AIDS atau dalam kemoterapi, infeksi toksoplasma dapat menyebabkan toksoplasmosis serebri.
Kejadian toksoplasmosis di Indonesia pada tahun 1982–1994 antara lain adalah 36,7% dan 8,4% di antaranya dialami oleh penyandang HIV/AIDS di Jakarta. Pada tahun 2011, data di Rumah Sakit Cipto Mangunkusumo (RSCM) Jakarta menunjukkan bahwa infeksi toksoplasma mencakup 48,5% infeksi oportunis pada penyandang HIV/AIDS.
Penyebab
Toksoplasmosis serebri disebabkan oleh parasit Toxoplasma gondii. T. gondii dapat menginfeksi berbagai hewan, namun host utama dari parasit ini adalah kucing. Parasit ini masuk ke tubuh manusia dalam bentuk kista yang akan berubah bentuk dan menetap di saraf dan otot. Keberadaan kista ini akan memicu respon peradangan tubuh dan menyebabkan gejala.
Infeksi ini tidak ditularkan dari manusia ke manusia, melainkan dari hewan ke manusia. Paparan terhadap kotoran kucing merupakan jalur yang utama. Kucing, baik liar maupun peliharaan, merupakan satu-satunya hewan yang dapat mengeksresikan kista parasit ini di dalam kotorannya. Beberapa kondisi yang dapat menyebabkan seseorang terinfeksi toksoplasma, antara lain:
- Mengonsumsi daging hewan kurang matang. Hewan lain dapat terinfeksi toksoplasma dan kista parasit tersebut menetap di otot atau daging hewan. Jika Anda mengonsumsi daging hewan tersebut dalam kondisi kurang matang, Anda berisiko terinfeksi toksoplasma.
- Terpapar kotoran kucing yang mengandung parasit ketika sedang membersihkan kandang kucing atau ketika menyentuh apapun yang terpapar dengan kotoran kucing
- Mengonsumsi makanan atau air yang terkontaminasi parasit. Susu yang tidak terpasteurisasi dapat mengandung parasit. Buah-buahan dan sayur yang tidak dicuci dengan baik dapat mengandung parasit, sehingga penting untuk mengupas buah sebelum dikonsumsi.
- Penularan dari ibu ke anak.
- Terpapar dari transplantasi organ atau transfusi darah.
Jika Anda terpapar dengan T. gondii, kista parasit tersebut dapat menetap di seluruh bagian tubuh, termasuk otak dan jantung. Imunitas yang baik dapat mengatasi parasit tersebut dan membuatnya tidak aktif. Namun, jika imunitas Anda menurun atau Anda mengonsumsi obat-obatan untuk menurunkan imunitas, infeksi ini dapat kembali dan menyebabkan komplikasi berat.
Faktor Risiko
Semua orang dapat mengalami toksoplasmosis. Namun, toksoplasmosis serebri lebih sering menyerang populasi berikut:
- Penyandang HIV/AIDS dengan CD4 <200 sel/uL. Penyandang HIV/AIDS lebih rentan mengalami toksoplasmosis, baik infeksi yang baru terjadi maupun reaktivasi dari infeksi sebelumnya. Hal ini lebih sering terjadi pada penyandang yang tidak mengonsumsi antibiotik profilaksis sebelumnya.
- Menjalani kemoterapi. Kemoterapi dapat menurunkan sistem imun Anda dan menyebabkan tubuh Anda tidak dapat mengatasi infeksi.
- Mengonsumsi steroid atau obat-obatan penekan sistem imun.
Gejala
Gejala yang dapat dialami seseorang dengan toksoplasmosis serebri, antara lain:
- Nyeri kepala
- Gangguan penglihatan
- Kelumpuhan saraf otak
- Leher kaku
- Kejang
- Muntah menyemprot
- Penurunan kesadaran
Diagnosis
Dokter akan menanyakan mengenai perjalan penyakit Anda, riwayat penyakit dahulu, dan obat-obatan yang Anda konsumsi. Diagnosis pasti dari toksoplasmosis serebri adalah dengan menemukan kista pada biopsi otak, namun hal ini jarang dilakukan. Pemeriksaan penunjang yang sering dilakukan untuk membantu penegakan diagnosis, antara lain:
- Serologi. Pemeriksaan titer antibodi terhadap toksoplasma dapat bertindak sebagai skrining cepat. Namun, hasil pemeriksaan serologi yang negatif belum tentu pasti mengeksklusi toksoplasma, terutama di Indonesia yang memiliki kejadian toksoplasma yang tinggi.
- CT scan atau MRI dengan kontras. Pemeriksaan ini bertujuan untuk memberikan gambaran radiologis terhadap kondisi kepala dan otak. Prosedur MRI merupakan prosedur dengan risiko rendah dan noninvasif, walaupun memakan waktu lama. Pada penyandang toksoplasmosis, dokter dapat menemukan lesi menyangat berbentuk cincin pada otak.
- PCR cairan serebrospinal.
Tata Laksana
Pengobatan toksoplasmosis serebri bertujuan untuk membatasi parasit memperbanyak diri selama infeksi aktif. Terapi ini terutama diberikan pada individu dengan kelemahan sistem imun dan infeksi yang berkepanjangan. Pengobatan toksoplasmosis serebri dapat dibagi menjadi dua fase, yaitu terapi primer dan terapi sekunder. Pada kedua fase tersebut, dokter akan memberikan tiga kombinasi antibiotik yang berbeda. Terapi primer dilakukan selama minimal 6 minggu, sedangkan terapi sekunder akan diberikan selama 6 bulan berturut-turut setelahnya. Dokter juga dapat memberikan asam folat untuk mencegah defisiensi (kekurangan) asam folat.
Komplikasi
Pada kondisi infeksi berat, toksoplasmosis serebri dapat menyebabkan kematian. Namun, jika ditangani dengan cepat dan tepat, toksoplasmosis serebri dapat mengalami perbaikan klinis setelah 10-14 hari setelah pemberian antibiotik. Relaps (kambuh) dari penyakit ini merupakan hal yang cukup sering terjadi. Melanjutkan terapi ARV secara rutin dan penggunaan antibiotik sangat penting untuk mencegah kekambuhan penyakit.
Salah satu penyulit dari toksoplasmosis serebri pada penyandang HIV/AIDS adalah kemungkinan terjadi Immune Reconstruction Inflammatory Syndrome (IRIS) dengan penggunaan ARV dan antibiotik secara bersamaan.
Pencegahan
Pencegahan merupakan faktor penting dari toksoplasmosis serebri. Langkah pencegahan tersebut antara lain:
- Menggunakan sarung tangan jika sedang berkebun atau berkontak dengan tanah.
- Jangan mengonsumsi daging yang kurang matang.
- Bersihkan alat dapur Anda secara menyeluruh, terutama setelah mengolah daging mentah. Gunakan air hangat dan sabun untuk mencegah kontaminasi ke makanan lain. Cuci tangan Anda setelah mempersiapkan makanan.
- Cuci seluruh buah-buahan dan sayur sebelum dikonsumsi. Jika memungkinkan, kupas buah-buahan tersebut setelah dicuci.
- Jangan konsumsi susu yang tidak dipasteurisasi.
- Jaga kesehatan kucing peliharaan kesayangan Anda. Hindari memberikan daging mentah dan berikan kucing makanan kaleng atau kering. Lakukan pemeriksaan kesehatan kucing Anda secara berkala.
- Hindari mengadopsi kucing liar. Jika Anda ingin mengadopsi salah satunya, lakukan pemeriksaan T. gondii sebelumnya. Kucing umumnya tidak menunjukkan tanda terinfeksi parasit, sehingga pemeriksaan perlu dilakukan.
- Lakukan pemeriksaan kesehatan lengkap sebelum hamil.
Pencegahan yang dapat dilakukan oleh penyandang HIV/AIDS adalah dengan mengonsumsi antibiotik profilaksis jika hasil CD4 <200 sel/uL hingga mendapatkan ART dan CD4 dapat bertahan >200 sel/uL selama tiga bulan berturut-turut. Konsultasikan hal ini dengan dokter Anda.
Kapan Harus ke Dokter?
Jika Anda merupakan penyandang HIV/AIDS, sedang mengonsumsi obat-obatan yang dapat menurunkan kekuatan sistem imun, sedang hamil atau berencana akan hamil, lakukan pemeriksaan di fasilitas kesehatan terdekat mengenai kondisi Anda dan kemungkinan Anda mengalami infeksi toksoplasma. Hasil yang negatif dapat berarti Anda tidak terpapar oleh toksoplasma, atau infeksi yang terjadi masih bersifat akut. Konsultasikan pengobatan selanjutnya dengan dokter Anda.
Gejala awal dari toksoplasmosis serebri, seperti nyeri kepala hebat, gangguan penglihatan, kejang, hingga kehilangan kesadaran merupakan tanda bahaya di mana harus segera ditangani di fasilitas kesehatan.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Nadia Opmalina
Aninditha T, Wiratman W. (2017). Buku Ajar Neurologi. Departemen Neurologi Fakultas Kedokteran Universitas Indonesia.
Madireddy S, Rivas Chacon ED, Mangat R. Toxoplasmosis. [Updated 2021 Sep 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563286/
Mayo Clinic Staff. (2020). Toxoplasmosis. MayoClinic. Available from: https://www.mayoclinic.org/diseases-conditions/toxoplasmosis/diagnosis-treatment/drc-20356255
Centers for Disease Control and Prevention. (2018). Toxoplasmosis (Toxoplasma infection). cdc.gov. Available from: https://www.cdc.gov/parasites/toxoplasmosis/index.html