Definition
A polyp is a term used to describe a small lump that grows on a mucous membrane. Polyps can appear on the nasal lining, respiratory tract, digestive tract, and reproductive system. The endocervix is the inner part of the cervix that is directly connected to the uterus. An endocervical polyp is a lump that grows from the endocervix in women. The endocervix is the part of the cervix that is examined by doctors during a pap smear to detect suspicious cells that could indicate cervical cancer.
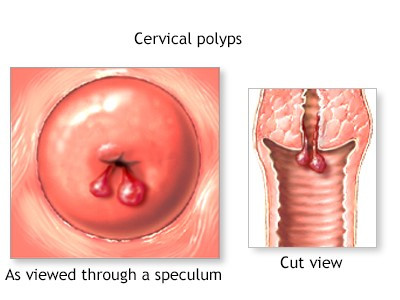
Broadly, cervical polyps are divided into two types: ectocervical polyps and endocervical polyps. The difference is that ectocervical polyps occur on the outer layer of the cervix, while endocervical polyps occur on the inner layer of the cervix. This article will focus on endocervical polyps.
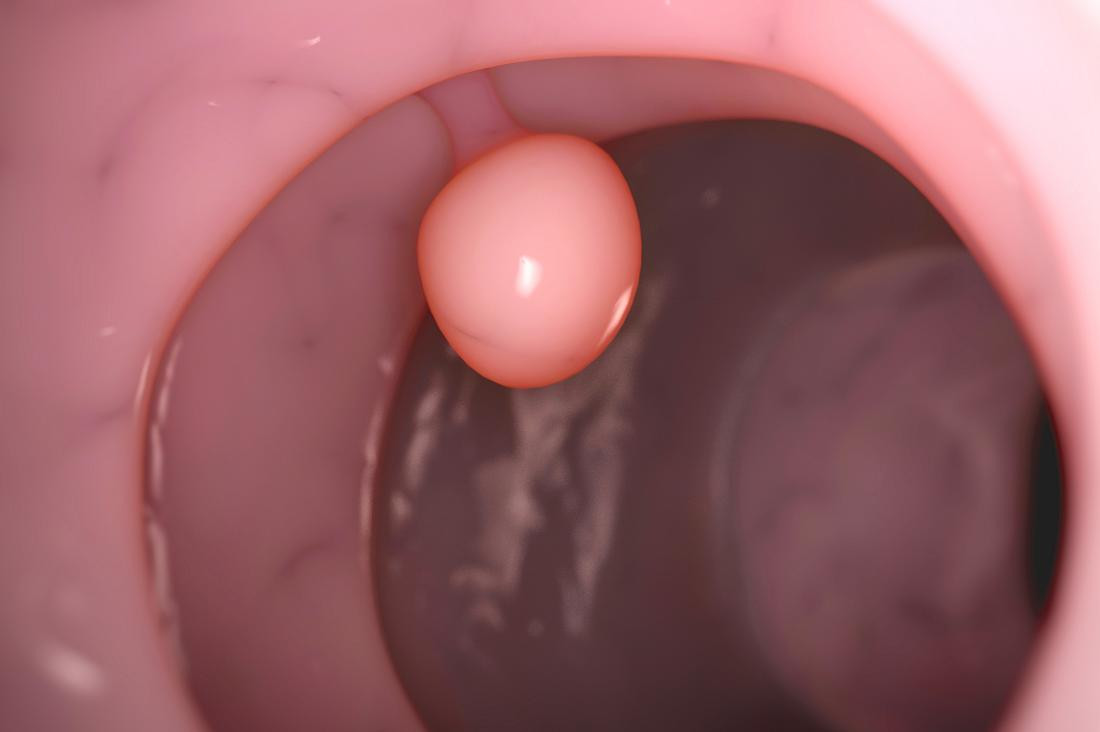
Polyps can occur in women of reproductive age, pregnant women, and even menopausal women. Endocervical polyps are rare in women who have not yet menstruated and are under 18 years old. Polyps can be stalked or non-stalked lumps. The size of endocervical polyps can vary from a few millimeters to 1-2 cm.
Although endocervical polyps are generally benign, polyps with malignant potential can be found in 0.2% to 1.5% of all cervical or endocervical polyps. However, polyps with malignant potential are more common in menopausal women.
Endocervical polyps are the second most common type of polyp found in women, after endometrial polyps. The number of women with endocervical polyps is 2-5% of all women worldwide. Women who have given birth more than once are more likely to develop endocervical polyps compared to those who have never given birth. One in eight women experiences a recurrence of polyps after undergoing surgery.
Causes
Obstruction of Cervical Blood Vessels
The exact cause of endocervical polyps is still unknown. However, several theories are believed by scientists. One such theory suggests that a blockage in the blood vessels of the cervix can disrupt blood flow, leading to polyp development.
Chronic Inflammation of the Cervix
Another theory posits that polyps are caused by chronic infection or inflammation of the cervix. Prolonged exposure to certain chemicals may also cause abnormal changes in the cells of the cervix.
Increased Estrogen Levels
Lastly, many scientists believe that an increase in estrogen levels causes excessive growth of cervical tissue, which is associated with changes in cervical cells.
Risk Factor
The following factors increase the risk of endocervical polyps:
- Premenopausal age (around 40 years old)
- Given birth more than once
- Experienced sexually transmitted infections (STIs)
- Previous history of cervical polyps
Symptoms
Polyps may or may not cause symptoms. Usually, polyps that do not cause symptoms are small. The following symptoms may occur:
- Irregular vaginal bleeding outside the menstrual cycle or after sexual intercourse
- Thick, white vaginal discharge, which can be foul-smelling and different from normal discharge, often due to infection in the uterus
Diagnosis
The diagnosis of endocervical polyps is made through medical interviews, physical examinations, and supporting tests.
The interview begins with questions about the patient's main complaint, accompanying symptoms, menstrual history, pregnancy history, history of certain medications, past medical history, and family history.
Physical Examination
Next, a physical examination is conducted. The doctor will start by assessing the general condition of the patient, including blood pressure, body temperature, respiratory rate, and pulse. Then, the doctor will perform a specific examination of the vagina.
The doctor will examine the external part of the vagina and use a speculum to examine the internal part. The purpose of the speculum examination is to observe the condition inside the cervix so that any internal bleeding or polyps can be detected. The doctor will also check for signs of vaginal discharge that may indicate an infection.
Diagnostic Tests
The doctor may also recommend supporting tests. These may include a biopsy, where a small sample of polyp tissue is taken and examined under a microscope in a laboratory. If the vaginal discharge is suspected of being related to a sexually transmitted infection, the doctor may also take a sample of the discharge for laboratory analysis to determine if there is an STI accompanying the polyp.
The above procedure is important in diagnosing endocervical polyps. If not correctly diagnosed, endocervical polyps can be mistaken for other conditions, including:
- Myoma
- Endometriosis
- Adenomyosis
- Cervical cancer
- Sexually transmitted infections
- Ectopic pregnancy
- Cervical ectropion
- Endometrial hyperplasia
If you want to read more about endometrial hyperplasia, you can read it here: Endometrial Hyperplasia - Definition, Cause, Symptoms, and Treatment.
Management
In some cases, endocervical polyps may disappear on their own during menstruation or sexual intercourse. Various treatments and therapies for endocervical polyps include:
- Using forceps to remove the polyp
- Eliminating the base of the polyp with surgical thread
- Twisting the base of the polyp
In addition, the doctor may use liquid nitrogen to remove the polyp, laser surgery, dilation and curettage, traditional surgery, and electrocautery ablation.
You may experience mild and brief pain during the polyp removal process, which may last a few hours afterward. Vaginal spotting may occur for 1-2 days after removal.
The efficacy of polyp excision is generally high, although in some cases, polyps may regrow, but this is rare, and the polyps usually do not recur.
Complications
The main complications of endocervical polyps include infertility, especially if the polyp grows large enough to block the external part of the cervix. Additionally, polyps can become infected if they swell and become contaminated with certain bacteria or viruses.
For polypectomy or polyp removal procedures, possible complications include:
- Infection
- Bleeding
- Uterine perforation
All polypectomy procedures should be performed by an obstetrician and gynecologist.
Prevention
Although most endocervical polyps are benign, you can prevent them by:
- Regular pelvic exams
- Pap smear tests as recommended
- Wearing cotton underwear that absorbs sweat and is not too tight to prevent vaginal infections
- Avoiding multiple sexual partners
- Using condoms during sexual intercourse to prevent sexually transmitted infections (STIs)
When to See a Doctor?
Consult a doctor if you experience heavy vaginal bleeding outside your menstrual period, foul-smelling vaginal discharge, or if you have risk factors for endocervical polyps. You may seek advice from an obstetrician and gynecologist.
Looking for more information about other diseases? Click here!
- dr Anita Larasati Priyono
What Are Cervical Polyps. Healthline. (2022). Retrieved 6 November 2022, from https://www.webmd.com/women/cervical-polyps
Cervical Polyps. WebMD (2021). Retrieved 6 November 2022, from https://www.webmd.com/women/cervical-polyps
YG Alkilani, I Apodaca - Ramos. (2022). Cervical Polyps. Retrieved 6 November 2022, from https://www.ncbi.nlm.nih.gov/books/NBK562185/