Definition
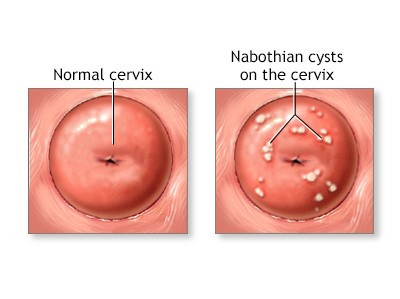
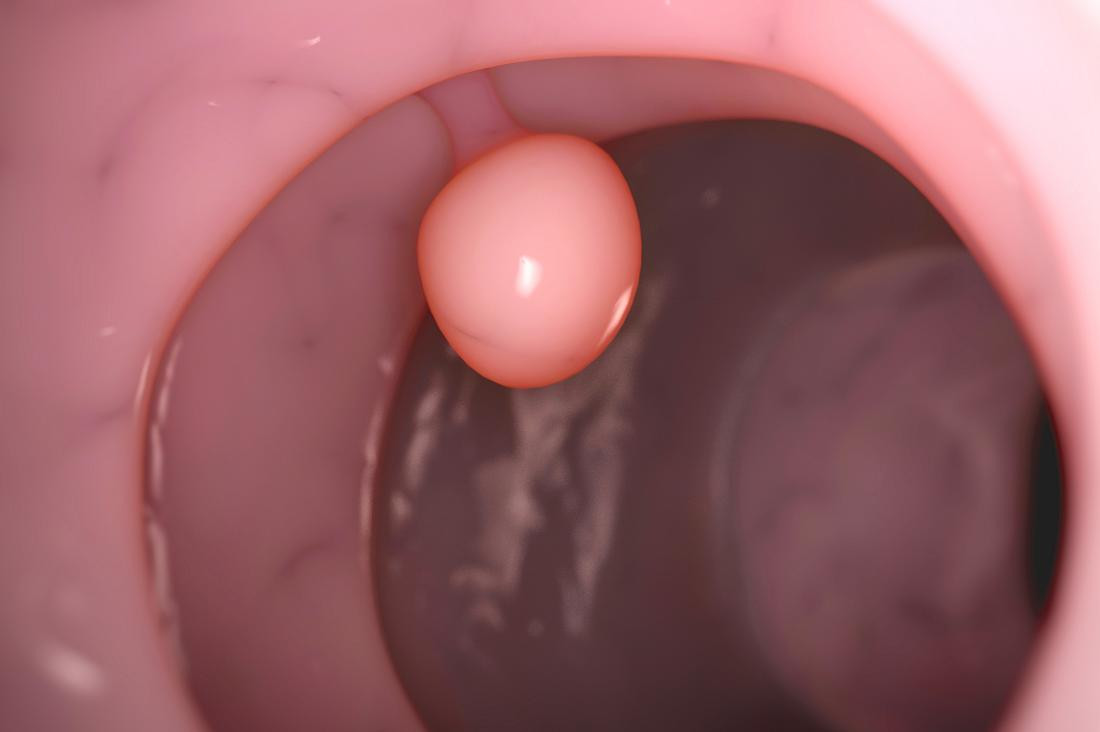
Cervical polyps are benign tumors or non-cancerous growth that often extend outward from the layer of the cervical canal. The cervix is the lower portion of the uterus that serves as the connection between the uterus and the vagina. The ectocervix is the outer portion of the cervix that connects to the vagina. The ectocervix is lined with squamous cells, which appear thin and flat when observed under a microscope. Polyps are delicate tumors that develop from stems anchored on the cervical surface or within the canal. Typically, individuals with polyps have only one polyp and, at most, two or three polyps.
So, it can be inferred that ectocervical polyps are benign growths that develop in the outer part of the cervix. Cervical polyps frequently manifest in women of reproductive age, particularly after 20 years old. While most cervical polyps are non-cancerous or benign, a really small percentage (0.2 to 1.5%) of cases could be malignant. Postmenopausal women have a higher likelihood of developing malignant polyps.
Cervical polyps are classified based on where they originated in the cervix, including:
- Endocervical polyps are the commonest type of cervical polyps and typically manifest in premenopausal women. The polyps commonly originate from the endocervix, which is the inner region of the cervix responsible for forming the endocervical canal.
- Ectocervical polyps are predominantly found in postmenopausal women and originate from the squamous cells on the ectocervix or the outer surface of the cervix.
We also have an article on cervical polyps that you can read here: Cervical Polyp - Definition, Cause And Risk Factor.
Causes
The precise etiology and exact mechanism of ectocervical polyp remain unknown at present. The exact cause is not yet fully comprehended, but several theories have been suggested.
The development of cervical polyp could potentially be associated with:
- Abnormal reaction to an elevation of estrogen levels in the body, leading to excessive proliferation of cervical tissue
- Infection or chronic inflammation of the cervix
- Prolonged exposure to some certain chemicals can potentially lead to abnormal cellular changes in the cervix
- Cervical blood vessel blockage can cause disruptions in blood flow, which can contribute to the development of polyps
Risk Factor
The occurrence of the polyp is predominantly limited to women who have a prior history of pregnancy. Women who have not given birth to a child have a lower risk of developing cervical polyps compared to women who have been pregnant more than once. Here are some other factors that may elevate the risk of cervical polyps:
- Premenopausal women
- Sexually transmitted infections (STIs)
- Prior medical history of cervical polyps
It is crucial to acknowledge that the presence of a risk factor does not guarantee the development of the disease. Furthermore, the absence of a risk factor does not guarantee that an individual will remain unaffected.
Symptoms
Cervical polyps may be asymptomatic. Two-thirds of women with cervical polyps do not show any symptoms. Nevertheless, women who experience symptoms typically exhibit abnormal uterine bleeding, including excessive menstrual bleeding, bleeding between periods, uterine bleeding in postmenopausal women, or vaginal discharge. Infertility can occur when the cervical canal is obstructed by big polyps, however this is a rare occurrence.
Certain symptoms may potentially indicate the presence of malignancy. Polyps can occasionally indicate the initial stage of cervical cancer. Removing the cervical polyp could aid in reducing the risk of malignancy.
Diagnosis
Cervical polyps are typically found by chance during routine pelvic examinations, colposcopies, or abdominal or transvaginal ultrasounds. During a pelvic exam, there could be a presence of long, smooth finger-shaped protrusions on the cervix. The polyps could be red or purple.
During a pelvic exam, a procedure could be performed to collect cells from the ectocervix. The collected samples are then dispatched to a laboratory. These cells are then examined under a microscope to detect any signs of infection, inflammation, cervical cancer, or precancerous alterations. The results often indicate the presence of noncancer polyp cells. Occasionally, there may be instances where there are abnormal cells or patterns of growth that indicate the early stages of cancer.
Management
The management of cervical polyps is determined by their clinical features. Typically, asymptomatic polyps do not require treatment. Sometimes, polyps can detach by themselves from your cervix. Exceptions are made and polyp removal is typically recommended for women that experience symptoms, or the polyps are big or display atypical characteristics.
The method for removing polyps is as follows:
- Rotate the polyp at its base
- The polyp can be removed by pinching the base and cutting it off
- The doctor will remove the polyp using forceps
In some cases, polyps cannot be removed because they are too large. In this case, the doctor will advise you to undergo surgery at the hospital. Polyps that have been removed usually will not return if it is removed properly.
Complications
Polyps have the potential to bleed, which can lead to the occurrence of secondary infections. In addition, postpartum bleeding might be a significant problem due to the vascularity of polyps. Cervical polyps also have the potential to turn malignant. Several studies have indicated that 5% of women experiencing symptoms had polyps that were either precancerous or cancerous. Thus, in women with cervical polyps suspected of malignancy, it is necessary to conduct additional histological examinations in such circumstances. Emotional distress may arise as a result of anxiety and worry about polyps that could turn into cervical cancer.
Prevention
Currently, there are no established ways to prevent the occurrence of ectocervical polyps. However, hysteroscopic polyp removal is considered a gold standard for treating cervical polyps. This treatment option attains a significantly high level of success.
If you have previously experienced polyps, you are more susceptible to experiencing polyp recurrence. Undergoing regular pelvic exams and Pap tests is crucial in detecting any abnormal growths in your cervix. The frequency of Pap tests that you should do is determined on your comprehensive medical history and age. The test is usually recommended to be done every 3-5 years for women who have not previously experienced abnormal Pap findings.
When to See a Doctor?
If you have white or yellow mucus vaginal discharge or unusually heavy bleeding in your periods, it is advisable to promptly consult a gynecologist. Women that experience vaginal spotting or bleeding at this time:
- Post-coitus or after sexual intercourse
- Between periods
- Post-douching
- Postmenopause
They are also advised to have medical consultations.
Looking for more information about other diseases? Click here!
- dr Hanifa Rahma
Alkilani, Y. G., Apodaca-Ramos, I. (2023). Cervical Polyps. Retrieved 31 December 2022, from https://www.ncbi.nlm.nih.gov/books/NBK562185/
National Cancer Institute. Ectocervix. Retrieved 31 December 2022, from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/ectocervix
Nwadike, V. R. (2022). What are Cervical Polyps? Retrieved 31 December 2022, from https://www.healthline.com/health/cervical-polyps#
Purohit, M. P. (2019). Benign Ectocervical Polyp. Retrieved 31 December 2022, from https://www.dovemed.com/diseases-conditions/benign-ectocervical-polyp