Definisi
Prolaps uterus atau sering dikenal dengan turun peranakan adalah kondisi rahim yang jatuh ke vagina akibat otot dan jaringan rahim melemah. Kondisi ini merupakan bagian dari Prolaps Organ Panggul (POP). Prolaps uterus umumnya terjadi pada wanita setelah menopause, wanita yang melahirkan lebih dari sekali, wanita dengan riwayat keluarga prolaps uterus, atau riwayat operasi di organ panggul.
Otot dasar panggul yang menopang rahim, anus, vagina, kandung kemih, dan organ panggul dapat melemah atau rusak sehingga tidak dapat menyokong organ-organ tersebut. Hal ini menyebabkan organ pelvis turun atau jatuh ke vagina. Rahim dapat keluar dari posisi nya dan turun ke vagina.
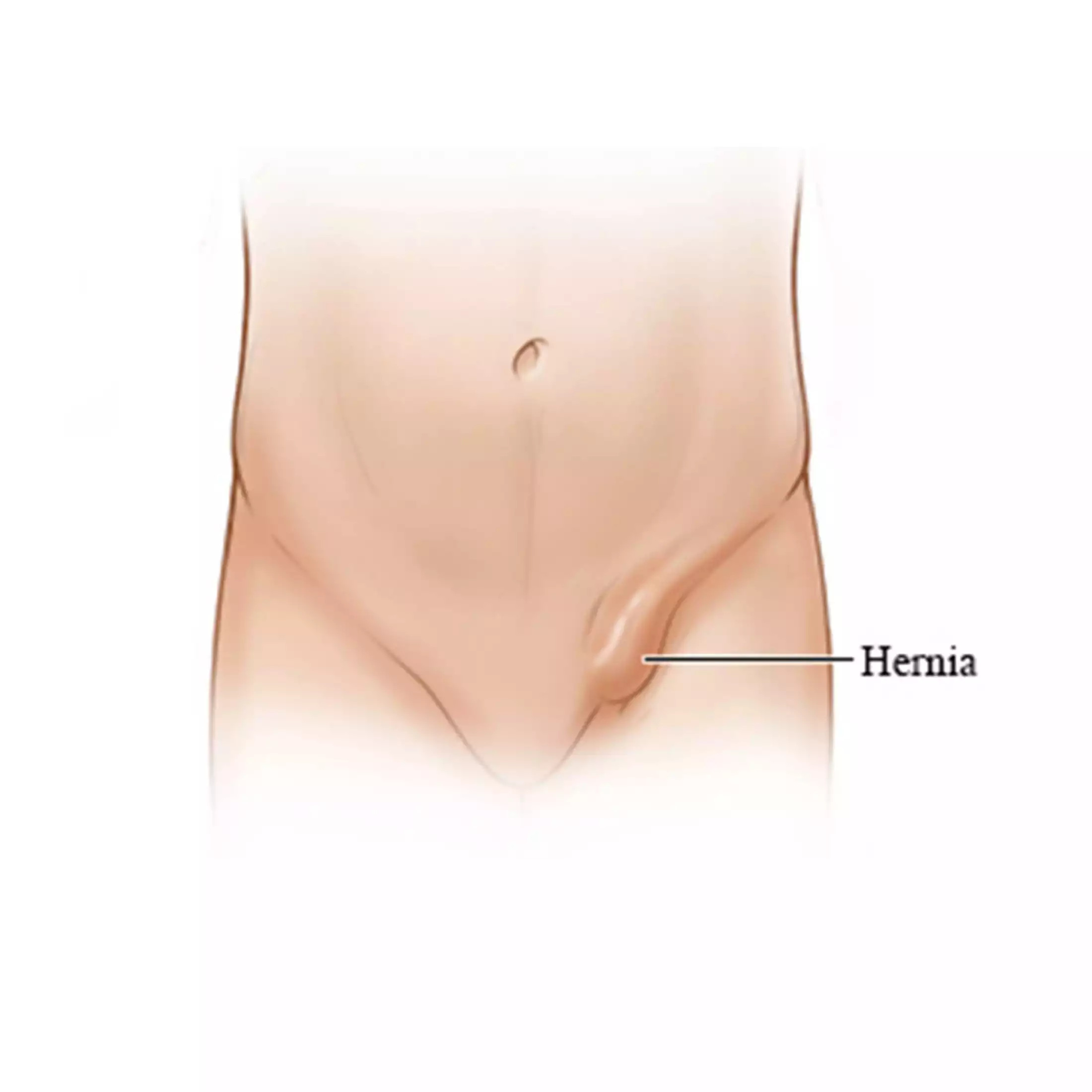
Prolaps uterus dapat terlihat mulai dari seperti benjolan hingga adanya organ rahim yang terlihat turun di vagina.
Terdapat beberapa derajat klasifikasi prolaps uterus, antara lain:
- Derajat 1 : rahim jatuh ke bagian atas dari vagina
- Derajat 2 : rahim jatuh ke bagian bawah dari vagina
- Derajat 3 : rahim menonjol dari vagina
- Derajat 4 : Seluruh rahim nampak keluar dari vagina
Penyebab
Melemahnya otot dasar panggul menjadi penyebab utama prolaps uterus. Namun, terdapat beberapa penyebab lain dari terjadinya prolaps uterus, antara lain:
- Riwayat persalinan melalui vagina, terutama bila melahirkan bayi kembar atau berat badan bayi lebih dari 4 kg.
- Kondisi yang menyebabkan tekanan pada bagian perut, seperti batuk kronis (pada bronkitis dan asma), mengejan (pada konstipasi), tumor organ panggul, atau akumulasi cairan pada perut.
- Riwayat operasi besar pada bagian panggul yang menyebabkan hilangnya fungsi penyokong otot.
- Merokok karena dapat menyebabkan batuk kronis.
Faktor Risiko
Beberapa faktor risiko meningkatnya terjadinya prolaps uterus seperti:
- Riwayat persalinan atau operasi melalui vagina.
- Bertambahnya usia (penuaan). Hal ini berkaitan dengan menurunnya kadar hormon estrogen.
- Olahraga berlebihan, terutama memerlukan banyak mengejan.
- Riwayat keluarga dengan kondisi prolaps uterus.
- Gaya hidup seperti merokok dan berat badan berlebih (obesitas).
Gejala
Prolaps uterus dapat tidak bergejala, terutama pada derajat sedang. Namun, seiring dengan bergesernya rahim dari posisinya, hal ini dapat memberikan tekanan pada organ panggul lainnya (seperti kandung kemih). Jika derajat prolaps uterus semakin berat, dapat terjadi gejala sebagai berikut:
- Rasa berat, penuh, atau tertekan pada panggul.
- Nyeri pada panggul atau perut bagian bawah.
- Nyeri ketika berhubungan seksual
- Jaringan rahim yang keluar melalui bukaan vagina.
- Kesulitan dalam memasukkan tampon atau aplikator lain ke dalam vagina.
- Konstipasi
- Keinginan berkemih terus-menerus atau mendadak. Seringkali pasien juga tidak dapat menahan keinginan berkemih atau mengalami inkontinensia urin.
Gejala di atas dapat memburuk ketika berdiri atau berjalan dalam waktu yang lama, batuk, dan bersin. Kondisi tersebut diakibatkan adanya gravitasi yang memberikan tekanan tambahan pada otot dasar panggul.
Diagnosis
Dokter akan memeriksa panggul untuk menentukan posisi rahim. Pada pemeriksaan panggul, dokter akan memasukkan alat bernama spekulum untuk melihat kondisi vagina dan rahim.
Dokter akan memeriksa apakah ada benjolan yang menyebabkan rahim turun ke dalam vagina. Selain itu, dokter akan meminta pasien untuk batuk, mengejan, atau seperti menahan air kencing. Hal ini dapat melihat seberapa lemah otot dasar panggul.
Dokter juga akan menyarankan pasien melakukan pemeriksaan radiologi, seperti MRI (Magnetic Resonance Imaging). Pemeriksaan ini akan memberikan gambaran mengenai organ-organ panggul serta organ sekitar panggul.
Selain MRI, dokter dapat menyarankan pemeriksaan penunjang lain, seperti foto rontgen saluran kemih, USG panggul dan saluran kemih, serta tes fungsi otot dan saraf.
Tata Laksana
Terapi prolaps uterus dapat dilakukan melalui nonoperasi dan operasi. Berikut penjelasan mengenai tata laksana prolaps uteri:
Tata laksana nonoperasi
- Perubahan gaya hidup, seperti mengurangi atau berhenti merokok dan mengurangi berat badan.
- Perbanyak konsumsi air dan fiber untuk mencegah konstipasi.
- Melakukan olahraga untuk memperkuat otot dasar panggul. Olahraga jenis kegel exercise dapat dilakukan dengan menekan otot yang mengendalikan aliran kemih dan ditahan hingga 10 detik lalu dilepaskan. Lakukan hingga 50 kali sehari.
- Penggunaan alat vaginal pessary, yaitu alat yang berbentuk seperti donat terbuat dari plastik yang pas disekitar area bagian bawah rahim anda. Alat ini membantu menyokong rahim pada tempatnya. Dokter akan membantu mengatur dan menjelaskan penggunaan alat tersebut. Alat tersebut harus sering dibersihkan dan dilepaskan ketika berhubungan seksual.
Tata laksana operasi
- Operasi perbaikan posisi rahim. Tindakan ini dapat dilakukan dengan mengganti jaringan penyangga rahim.
- Operasi pengangkatan rahim atau disebut dengan histerektomi.
Komplikasi
Komplikasi yang muncul dari prolaps uterus di antaranya:
- Prolaps vagina anterior atau disebut dengan sistokel
- Prolaps anterior terjadi karena lemahnya jaringan ikat yang memisahkan kandung kemih dan vagina sehingga membengkak ke dalam vagina.
- Prolaps vagina posterior atau disebut dengan rektokel
- Prolaps vagina posterior terjadi karena lemahnya jaringan ikat yang memisahkan usus besar dengan vagina sehingga usus melebar ke dalam vagina. Hal ini dapat menyebabkan kesulitan buang air besar.
- Rahim menonjol keluar
- Infeksi
- Hal ini disebabkan adanya gesekan antara pakaian yang dapat menyebabkan luka pada vagina. Bila tidak segera diobati, infeksi tersebut dapat meningkatkan risiko cedera pelvis dan menyebabkan luka pada serviks.
Pencegahan
Beberapa hal di bawah ini dapat mengurangi risiko prolaps uterus, yaitu:
- Mengonsumsi air yang cukup dan makanan tinggi serat seperti buah, sayur, biji, dan kacang - kacangan untuk mencegah konstipasi.
- Menghindari mengangkat barang berat atau angkat berat dengan postur yang tidak benar. Bila mengangkat barang berat, gunakan postur dengan menggunakan tenaga kaki dibandingkan menarik pada pinggang atau punggung.
- Mengobati batuk bila disebabkan oleh batuk kronis atau bronkitis.
- Menghindari dan berhenti merokok sehingga mengurangi risiko batuk kronis.
- Berolahraga secara teratur untuk menjaga berat badan.
- Lakukan kegel excercises untuk memperkuat otot dasar panggul.
Kapan Harus ke Dokter?
Hubungi dokter bila Anda mengalami gejala prolaps uterus seperti:
- Anda merasa ada sesuatu yang mengganjal atau keluar dari vagina
- Nyeri ketika buang air kecil atau buang air besar
- Memiliki nyeri pada punggung bagian bawah atau tekanan panggul yang tidak disebabkan oleh kondisi lainnya.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Ayu Munawaroh, MKK
Uterine Prolapse. (2022). Retrieved 25 October 2022, from https://www.mayoclinic.org/diseases-conditions/uterine-prolapse/symptoms-causes/syc-20353458
Prolapsed Uterus. (2022). Retrieved 25 October 2022, from https://www.webmd.com/women/guide/prolapsed-uterus
Uterine Prolaps. (2022). Retrieved 25 October 2022, from https://www.ncbi.nlm.nih.gov/books/NBK564429/
Pelvic Organ Prolapse. (2021). Retrieved 25 October 2022, from https://www.nhs.uk/conditions/pelvic-organ-prolapse/
Uterine Prolapse. (2022). Retrieved 25 October 2022, from https://my.clevelandclinic.org/health/diseases/16030-uterine-prolapse
Prolapsed Uterus. (2021). Retrieved 25 October 2022, from https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/prolapsed-uterus
Uterine Prolapse. (2022). Retrieved 25 October 2022, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/uterine-prolapse