Definisi
Kandidiasis mukokutaneous adalah suatu infeksi jamur yang dapat mengenai hampir semua permukaan kulit dan mukosa tubuh. Mukosa merupakan lapisan selaput lendir lembab yang melapisi semua rongga tubuh dan saluran yang terpapar lingkungan luar, seperti mukosa mulut, mukosa pada saluran kemih, dll.
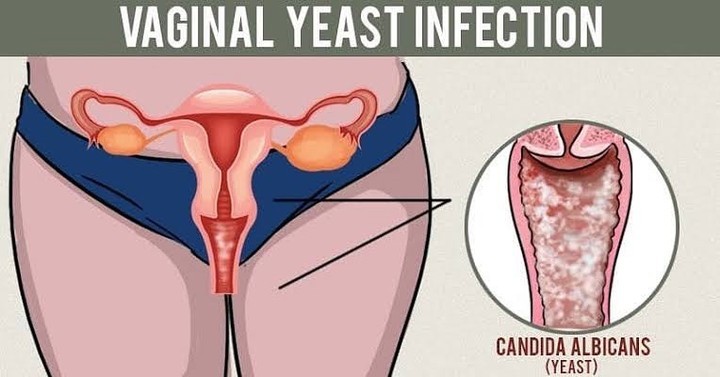
Infeksi kandidiasis mukokutaneous paling sering diakibatkan oleh jamur spesies Candida, terutama Candida albicans. Infeksi dapat terjadi di bagian tubuh mana saja dan paling sering terjadi pada lipatan kulit, alat kelamin, mukosa mulut, dan kuku. Infeksi ini pada dasarnya terbatas di permukaan kulit saja, dan tidak terlalu memiliki kecenderungan untuk menyebar secara luas dalam tubuh.
Kandidiasis mukokutaneous dapat bersifat kronis atau berlangsung dalam jangka waktu yang lama dan bersifat berulang, sehingga disebut juga dengan istilah kandidiasis mukokutaneous kronis. Jamur Candida normalnya terdapat pada kulit dan selaput lendir, dan pada umumnya jamur ini tidak menyebabkan suatu masalah kesehatan. Pada kandidiasis mukokutaneous, diduga terdapat gangguan sistem kekebalan tubuh terhadap spesies jamur Candida sehingga menimbulkan infeksi.
Penyebab
Kandidiasis mukokutaneus disebabkan oleh infeksi jamur Candida. Jamur Candida sendiri memiliki sekitar 150 jenis spesies yang berpotensi menimbulkan infeksi. Namun, spesies yang paling sering menyebabkan infeksi adalah Candida albicans, bertanggung jawab atas sekitar 70 sampai 80% dari semua infeksi Candida. Jenis spesies lain yang juga menyebabkan infeksi antara lain Candida glabrata, Candida tropicalis, Candida krusei, dan Candida dubliniensis.
Candida sendiri merupakan jamur yang sebenarnya tidak berbahaya dan normalnya terdapat pada kulit dan selaput lendir manusia. Hanya saja, pertumbuhan jamur ini dapat meningkat jika dipengaruhi kelembapan, suhu panas, dan adanya gangguan pada sistem pertahanan kulit dan tubuh. Kulit yang sehat dan tidak mengalami luka akan terus mengalami regenerasi kulit (pergantian sel kulit mati dengan sel kulit yang baru), sehingga menjadi pelindung awal yang efektif terhadap infeksi. Terganggunya sistem kekebalan tubuh, khususnya di kulit, dapat memengaruhi keseimbangan mikroorganisme di kulit dan menyebabkan terjadinya infeksi.
Kandidiasis mukokutaneus yang kronis disebabkan oleh adanya gangguan pada sistem kekebalan tubuh. Hal ini terkait dengan berbagai sindrom dan kelainan genetik, di mana terdapat kecenderungan mutasi genetik yang diwariskan dalam keluarga yang mengakibatkan penurunan fungsi sel-sel kekebalan tubuh dalam melawan infeksi. Kandidiasis mukokutaneus juga dikaitkan dengan gangguan kesehatan tertentu, seperti gangguan kelenjar tiroid, paratiroid, diabetes mellitus, dan penyakit Addison (kekurangan hormon kelenjar adrenal). Infeksi Human Immunodeficiency Virus (HIV) juga dapat muncul dengan candidiasis mukokutaneus kronis.
Faktor Risiko
Pada dasarnya, Candida tidak berbahaya dan memang terdapat pada kulit dan selaput lendir. Beberapa faktor dapat memengaruhi laju pertumbuhan jamur dan mengganggu keseimbangan mikroorganisme di kulit, sehingga menyebabkan timbulnya infeksi. Faktor-faktor yang dapat meningkatkan risiko infeksi Candida, antara lain:
- Cuaca yang panas dan lembab
- Sering menggunakan pakaian yang ketat
- Kebersihan kulit yang buruk
- Jarang mengganti popok pada bayi dan anak-anak atau jarang mengganti pakaian dalam pada pasien yang lebih tua
- Perubahan keseimbangan mikroorganisme di kulit akibat penggunaan antibiotik
- Memiliki penyakit kulit tertentu, seperti psoriasis yang dapat menyebabkan timbulnya peradangan pada kulit
- Menderita obesitas
- Memiliki sistem kekebalan tubuh yang menurun, bisa disebabkan akibat:
- Penggunaan obat kortikosteroid atau obat imunosupresif (penekan sistem kekebalan tubuh) lainnya
- Sedang hamil
- Menderita diabetes
- Menderita penyakit HIV/AIDS
- Memiliki gangguan terkait hormon, misalnya penyakit Cushing (kelenjar hipofisis manusia terlalu banyak menghasilkan hormon ACTH), penyakit Addison, atau kekurangan hormon kelenjar tiroid
Gejala
Secara umum gejala pada infeksi Candida berupa rasa gatal yang cukup intens atau rasa terbakar, terutama di sekitar vagina dan anus. Ruam kulit yang muncul tampak berwarna merah di bagian dalam lipatan tubuh, seperti di selangkangan dan celah antarbokong, di bawah payudara, di sudut mulut, antar sela-sela jari, dan di sekitar pusar. Di sekeliling ruam mungkin terdapat ruam-ruam lain yang berukuran lebih kecil.
Pada selaput lendir (mukosa), mungkin ditemui bercak keputihan. Infeksi Candida pada kuku dapat berkembang setelah melakukan manikur yang dilakukan secara tidak benar dan pada pekerja dapur dan orang lain yang tangannya terus-menerus terkena air. Pada orang gemuk, infeksi Candida biasanya terjadi di bawah lipatan perut. Infeksi Candida pada rongga mulut merupakan tanda umum dari penurunan sistem kekebalan tubuh. Kandidiasis mukokutaneus kronis biasanya memengaruhi kuku, kulit, rongga mulut, dan tenggorokan.
Pada kondisi berulang atau yang sudah berlangsung lama, kandidiasis mukokutaneus kronis ditandai dengan ruam merah, berkoreng, dan menebal yang menyerupai psoriasis, terutama pada hidung dan dahi, dan disertai gejala candidiasis di rongga mulut.
Gejala candidiasis mukokutaneous dapat bervariasi berdasarkan lokasi terjadinya infeksi, seperti:
- Rasa gatal dan ruam merah berbatas tegas pada lipatan kulit tubuh
- Lecet pada kulit yang berwarna keputihan dan disertai rasa gatal pada infeksi Candida di anus
- Bila infeksi berada di vulva dan vagina, dapat timbul:
- Rasa gatal, terbakar, atau iritasi di sekitar vagina dan vulva
- Ada cairan kental berwana putih, seperti keju yang menempel pada dinding vagina
- Bisa muncul ruam kemerahan, bengkak dan lecet di sekitar vagina
- Pada infeksi Candida di kuku, dapat timbul:
- Pembengkakan di tepi kuku yang tampak merah dan menyakitkan
- Pemisahan ujung kuku dari bantalan kuku dengan perubahan warna putih atau kuning
- Pada kandidiasis orofaringeal (pada rongga mulut dan tenggorokan), muncul lapisan putih pada selaput lendir mulut yang mungkin berdarah saat dikelupas
- Pada perlèche atau candidiasis yang terjadi di sudut mulut, bisa timbul retakan dan celah kecil di sudut mulut, kondisi ini dapat disebabkan oleh kebiasaan:
- Menjilat bibir
- Mengisap jempol
- Penggunaan gigi palsu yang tidak pas
- Kondisi lain yang membuat sudut mulut cukup lembab sehingga jamur dapat tumbuh
Diagnosis
Dalam mendiagnosis kandidiasis mukokutaneous, dokter akan mulai dengan melakukan wawancara dengan Anda. Dokter akan menanyakan beberapa pertanyaan, seperti:
- Gejala-gejala yang Anda alami
- Sudah berapa lama gejala dirasakan
- Di mana saja lokasi timbulnya ruam
- Riwayat kesehatan lainnya, meliputi riwayat infeksi Candida sebelumnya, riwayat penggunaan obat-obatan tertentu sebelumnya, dan riwayat penyakit lain yang mungkin diderita
Selanjutnya dokter akan melakukan pemeriksaan fisik dengan melihat langsung keadaan kulit dan ruam yang timbul. Diagnosis kandidiasis mukokutaneous pada dasaranya dapat ditegakkan berdasarakan hasil wawancara dan pemeriksaan fisik. Akan tetapi, untuk lebih memastikan diagnosis, dokter dapat melakukan pemeriksaan tambahan berupa pemeriksaan dengan larutan Kalium Hidroksida (KOH). Pada pemeriksaan ini dokter akan mengambil sampel kulit dengan sedikit mengerok kulit yang terdapat ruam. Kemudian sampel kulit tersebut akan ditetesi dengan larutan KOH dan diperiksa di bawah mikroskop untuk mencari adakah jamur Candida pada sampel kulit tersebut.
Tata Laksana
Terapi kandidiasis mukokutaneous umumnya dapat dilakukan dengan mencegah suasana yang lembap dan hangat di sekitar bagian tubuh yang terkena, misalnya dengan tidak menggunakan pakaian yang ketat, sering mengganti pokok atau pakaian dalam jika basah, menghindari kontak dengan air yang berlebihan, dll. Selain itu, dokter juga dapat meresepkan obat antijamur yang dapat berupa obat oles (salep, krim) atau obat yang diminum. Pemilihan dosis dan jenis antijamur yang digunakan tergantung dari lokasi infeksi Candida, seberapa luas infeksinya, dan apakah kondisi baru muncul atau sudah berlangsung lama dan sering berulang.
Komplikasi
Komplikasi kandidiasis mukokutaneous yang cukup sering terjadi adalah infeksi berulang di kemudian hari. Pada penderita dengan sistem kekebalan tubuh yang menurun, dapat terjadi penyebaran infeksi Candida ke seluruh tubuh melalui pembuluh darah. Selain itu, juga dapat terjadi infeksi sekunder oleh bakteri lain, misalnya infeksi saluran pernapasan atau infeksi kulit tambahan akibat bakteri Staphylococcus aureus.
Pencegahan
Beberapa langkah yang dapat Anda lakukan untuk mencegah timbulnya kandidiasis mukokutaneous, antara lain:
- Gunakan pakaian dalam yang menyerap keringat
- Gunakan pakaian yang longgar
- Hindari mandi dengan air yang terlalu panas
- Ganti pakaian jika basah
- Pada wanita, jika membersihkan alat kelamin, selalu bersihkan dari arah depan ke belakang
- Saat sedang menstruasi, gantilah tampon atau pembalut Anda sesering mungkin
- Kontrol kadar gula darah jika Anda menderita diabetes
- Gunakan antibiotik hanya jika perlu dan sesuai resep dokter
- Jaga kesehatan mulut dengan sikat gigi 2 kali sehari dan rajin berkumur
- Bersihkan gigi palsu secara teratur
Kapan Harus ke Dokter?
Seringkali ruam akibat infeksi jamur sulit dibedakan dengan penyakit kulit lainnya bagi orang awam. Konsultasikan diri Anda ke dokter jika mengalami gatal dan ruam yang mengarah ke infeksi jamur Candida. Dokter akan membantu Anda dalam mendiagnosis dan memberikan pengobatan yang tepat.
Mau tahu informasi seputar penyakit lainnya, cek di sini ya!
- dr Hanifa Rahma
Aaron, DM. Candidiasis (Mucocutaneous). (2021). Retrieved 24 Maret 2022, from https://www.msdmanuals.com/professional/dermatologic-disorders/fungal-skin-infections/candidiasis-mucocutaneous
Cherney, K. Ways to Prevent Yeast Infections. (2019). Retrieved 24 Maret 2022, from https://www.healthline.com/health/how-to-prevent-yeast-infections
Familial Candidiasis. Retrieved 24 Maret 2022, from https://medlineplus.gov/genetics/condition/familial-candidiasis/#references
Galadari, HI. Chronic Mucocutaneous Candidiasis. (2021). Retrieved 24 Maret 2022, from https://emedicine.medscape.com/article/1091928-overview
Gomez, J. Chronic Mucocutaneous Candidiasis. (2017). Retrieved 24 Maret 2022, from https://dermnetnz.org/topics/chronic-mucocutaneous-candidiasis
Roifman, CM. Chronic Mucocutaneous Candidiasis. (2019). Retrieved 24 Maret 2022, from https://www.uptodate.com/contents/chronic-mucocutaneous-candidiasis
Shinkai K, Fox LP. Mucocutaneous Candidiasis. In: Papadakis MA, McPhee SJ, Rabow MW. eds. Current Medical Diagnosis and Treatment 2020. McGraw Hill; 2020. Retrieved 23 Maret 2022, from https://accessmedicine.mhmedical.com/content.aspx?bookid=2683§ionid =225034992