Definition
Cutaneous tuberculosis (TB) is a form of skin disease caused by infection with Mycobacterium tuberculosis. Tuberculosis typically manifests in the lungs as pulmonary TB; however, it is classified as extrapulmonary TB when it affects other areas of the body. Specifically, TB that appears on the skin is known as cutaneous TB.
This form of tuberculosis is relatively uncommon in developed nations. Among patients with extrapulmonary TB, cutaneous TB accounts for approximately 1-2% of cases. Nonetheless, it is more prevalent in certain regions with high rates of HIV infection or in individuals with compromised immune systems. In many developing countries, TB continues to pose a significant health challenge.
Cutaneous TB presents with various symptoms in affected individuals. Primary cutaneous TB occurs when TB bacteria make direct contact with the skin, often entering through a wound and resulting in an initial infection site called a tuberculous chancre. However, the most common form of cutaneous TB is secondary, known as scrofuloderma.
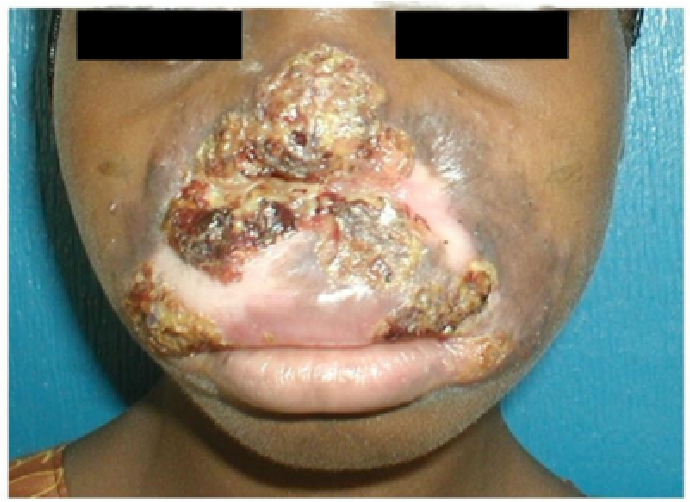
Scrofuloderma is a type of cutaneous TB that typically appears in the neck, where inflamed lymph nodes become irritated. In the United States, scrofuloderma accounts for about 10% of all TB cases diagnosed. Another recurrent form of cutaneous TB is lupus vulgaris, which can appear in various locations but is most frequently reported on the head and neck. Additionally, verrucous cutaneous TB can occur, characterized by nodules that form due to direct skin contact with TB-infected individuals.
Causes
Cutaneous TB is caused primarily by the bacteria Mycobacterium tuberculosis. Transmission occurs from infected individuals to others, although, in rare cases, other Mycobacterium species, such as Mycobacterium bovis, can also be responsible. Mycobacteria species belong to acid-fast bacilli (AFB), a group of bacteria known for their resistance to acidic environments or low pH levels.
Risk Factor
Identifying risk factors is essential in the prevention and management of cutaneous TB. While anyone can be susceptible, several factors heighten the likelihood of developing this condition.
Increased risk factors include:
- having close contact with someone actively infected with TB
- residing in or traveling to areas with a high TB prevalence
- living in densely populated settings
- working in healthcare facilities or similar environments
- inadequate sunlight exposure in living spaces
- possessing a compromised immune system, such as from certain medical treatments or conditions like HIV or cancer
However, exposure to Mycobacterium tuberculosis does not always result in infection, as the immune system’s strength plays a critical role. Around 10% of individuals exposed to the bacteria are estimated to develop active TB.
Symptoms
Typical symptoms, particularly with scrofuloderma, include swelling and lesions in the neck region. This swelling arises from enlarged lymph nodes as the body mounts an inflammatory response against the bacteria. These swollen glands are generally painless and not warm to the touch, although the area may increase in size and may eventually drain pus or other fluids over time.
Other common symptoms include fever, fatigue or lack of energy, night sweats, and unintentional weight loss.
Diagnosis
The diagnosis of cutaneous tuberculosis (TB) is primarily made through pathological analysis, where doctors rely on microscopic examination via a skin biopsy. This procedure typically reveals acid-fast bacilli (AFB) bacteria, which appear as characteristic clusters under the microscope.
Further diagnostic support can be obtained from PCR and culture tests conducted in the laboratory, which help identify the presence of TB bacteria. Additionally, the tuberculin skin test involves an injection beneath the skin, where any existing TB bacteria prompt a raised reaction at the injection site, typically a few millimeters in height.
Despite the high accuracy of these diagnostic tests, physicians also gather detailed patient histories and perform general physical examinations, assessing the characteristic lesions or spots in areas affected by cutaneous TB.
Patients should inform their doctor if they or any family members have had a prior TB or cutaneous TB infection. Information on the timing of symptom onset can assist the doctor in making an accurate diagnosis and in determining the best course of treatment at the initial consultation.
Management
Patients with TB, whether pulmonary or extrapulmonary (such as cutaneous TB), require treatment using a standardized anti-tuberculosis drug regimen, known as multi-drug therapy, which is employed worldwide. This regimen combines drugs like rifampicin, isoniazid, pyrazinamide, and ethambutol and typically requires a minimum of six months of treatment.
In certain cases, surgery may be recommended to improve the appearance of specific forms of cutaneous TB, such as lupus vulgaris and scrofuloderma. For some complex cases, like lupus vulgaris, reconstructive plastic surgery may also be necessary to address disfigurement caused by the infection.
Complications
Cutaneous TB is often linked with a compromised immune response to M. tuberculosis. Rarely, this infection can extend to adjacent areas of skin.
Lupus vulgaris and scrofuloderma, specific types of cutaneous TB, can cause extensive damage to nearby skin, leaving behind irregular scarring. Over time, lupus vulgaris can develop into squamous cell carcinoma or other forms of skin cancer in approximately 10% of cases, with cancer potentially emerging 25–30 years after the initial infection.
Prevention
Once aware of the associated risk factors, steps can be taken to mitigate preventable risks. These steps include:
- avoiding close contact with individuals infected with TB
- refraining from living in overcrowded environments
- ensuring proper ventilation in living spaces
- maintaining a home design that allows sunlight to enter
- adhering closely to prescribed medications and treatment plans
For those who have not yet seen a doctor, a general medical examination can help detect conditions that may increase the risk of developing cutaneous TB, enabling early intervention and prevention of worsening health.
When to See a Doctor?
If you experience prolonged skin symptoms, particularly if lesions continue to spread, it is advisable to consult with a dermatologist or a venereologist. The medical specialist will conduct a thorough medical history, physical examination, and relevant diagnostic tests to confirm the diagnosis and provide appropriate treatment.
Looking for more information about other diseases? Click here!
- dr Anita Larasati Priyono
Dermnet NZ. Cutaneous tuberculosis. March 2021. https://dermnetnz.org/topics/cutaneous-tuberculosis
Charifa A, Mangat R, Oakley AM. Cutaneous Tuberculosis. [Updated 2021 Aug 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482220/
Healthline. Scrofula. September 2018. https://www.healthline.com/health/scrofula#symptoms