Definisi
Anemia hemolitik merupakan gangguan darah yang membuat sel darah merah terurai atau mati lebih cepat dibandingkan terbentuknya sel darah merah baru oleh tubuh. Pada umumnya sel darah merah dapat hidup sekitar 120 hari. Ketika sel darah merah terurai atau mati terlalu cepat, sumsum tulang belakang tidak memiliki waktu yang cukup untuk menghasilkan sel darah merah yang baru sehingga menyebabkan anemia atau jumlah sel darah merah yang rendah.
Anemia tipe lain dapat terjadi ketika pendarahan berlebih sehingga sel darah merah terkuras lebih cepat dibanding kecepatan tubuh menghasilkan sel darah merah yang baru untuk menggantikan sel darah merah yang hilang. Anemia tipe lainnya dapat terjadi saat kondisi yang mempengaruhi produksi sel darah merah dalam tubuh sehingga menyebabkan jumlah sel darah merah lebih sedikit dari biasanya atau menghasilkan sel darah merah yang tidak normal.
Anemia hemolitik jarang terjadi dibandingkan tipe anemia yang disebabkan oleh pendarahan berlebih atau produksi sel darah merah yang rendah. Pasien penderita anemia hemolitik dapat disebabkan oleh kondisi genetik yang menyebabkan anemia. Beberapa orang dapat memiliki gejala ringan dari anemia hemolitik dan dapat hilang dengan adanya pengobatan.
Penyebab
Anemia hemolitik dapat disebabkan oleh kondisi genetik yang mempengaruhi sel darah merah. Kondisi yang mempengaruhi sel darah merah juga dapat disebabkan oleh kondisi infeksi tertentu atau bila menerima transfusi darah dari donor dengan golongan darah yang tidak sesuai. Selain kondisi genetik, infeksi dapat menyebabkan anemia hemolitik.
Beberapa kondisi genetik seperti :
- Anemia sel sabit
Tubuh menghasilkan sel darah merah berbentuk tidak normal sehingga terjebak pada pembuluh darah kecil dan pada hati
- Thalasemia
Salah satu gangguan darah genetik yang menyebabkan tubuh anda membentuk sel darah merah yang mudah terurai
- Kekurangan G6PD
Gangguan genetik yang mempengaruhi enzim yang melindungi sel darah merah. Ketika kadar enzim ini turun, sel darah merah akan terpapar pada infeksi atau pengobatan tertentu sehingga memungkinkan akan mudah terurai
Infeksi yang terkait atau dapat menyebabkan anemia hemolitik antara lain:
- Malaria
Penyakit terjadi ketika nyamuk yang terinfeksi dengan parasit malaria mengigit manusia sehingga parasit tersebut masuk ke dalam pembuluh darah. Bila tidak diobati, malaria dapat menyebabkan anemia hemolitik.
- Demam rocky mountain
Infeksi ini terjadi ketika kutu yang terinfeksi dengan bakteri Rickettsia rickettsi mengigit orang
- Penyakit influenza haemophilus
Infeksi ini disebabkan oleh bakteri influenza
- Human immunodeficiency virus (HIV)
Virus ini menyebabkan penurunan imunitas tubuh dan menyebabkan Acquired immunodeficiency syndrome (AIDS)
Selain hal yang telah disebutkan, kemungkinan lain penyebab dari anemia hemolitik adalah gangguan autoimun yang menyebabkan sistem imun memperkirakan sel darah merah sebagai benda asing sehingga menghancurkan sel darah merah sendiri. Penyebab lainnya adalah paparan pada zat kimia, obat, atau toksin tertentu, infeksi, adanya gumpalan darah pada pembuluh darah, dan transfusi darah dengan tipe darah yang tidak cocok dengan tipe golongan darah.
Faktor Risiko
Faktor risiko dari anemia hemolitik melibatkan kerusakan terhadap sel darah merah. Secara luas, faktor risiko dapat dikategorikan sebagai stress oksidatif, luka fisik, dan kondisi genetik. Pada stress oksidatif terkait dengan kekurangan G6PD yang dapat terjadi akibat efek dari penggunaan obat (Primiquin pada pengobatan malaria, dapson untuk PCP atau lepra, dan obat golongan sulfa untuk pengobatan kulit, infeksi saluran kecil, atau infeksi lain).
Gejala
Tingkat beratnya gejala dari anemia hemolitik dapat muncul dengan tingkat sedang hingga berat. Gejala dapat terjadi secara tiba - tiba atau muncul dengan berjalannya waktu.
Beberapa gejala yang dapat muncul seperti :
- Jaundice
Kondisi ini mempengaruhi kulit, bagian putih mata (sklera) dan membran mukus sehingga berubah menjadi kuning. Hal ini terjadi ketika kadar bilirubin tinggi yang disebabkan oleh pemecahan sel darah merah
- Sesak napas (dispnea)
Sesak terjadi ketika tubuh tidak memiliki sel darah merah yang mencukupi untuk membawa oksigen ke seluruh tubuh, sehingga menyebabkan sesak napas
- Kelelahan
- Detak jantung yang cepat (takikardia)
- Tekanan darah rendah
- Terdapatnya darah di urin (hematuria) yang dapat terhadi dari gejala anemia sel sabit.
- Pembesaran limpah atau hati
Limfa dan hati menyaring sel darah merah ketika sel bergerak melalui tubuh. Sel darah merah yang rusak atau segera mati akan tertahan di limfa dan hati yang akan menghancurkan sel. Pembesaran limfa atau hati dapat menjadi tanda bahwa sel darah merah mengalami kerusakan.
Diagnosa
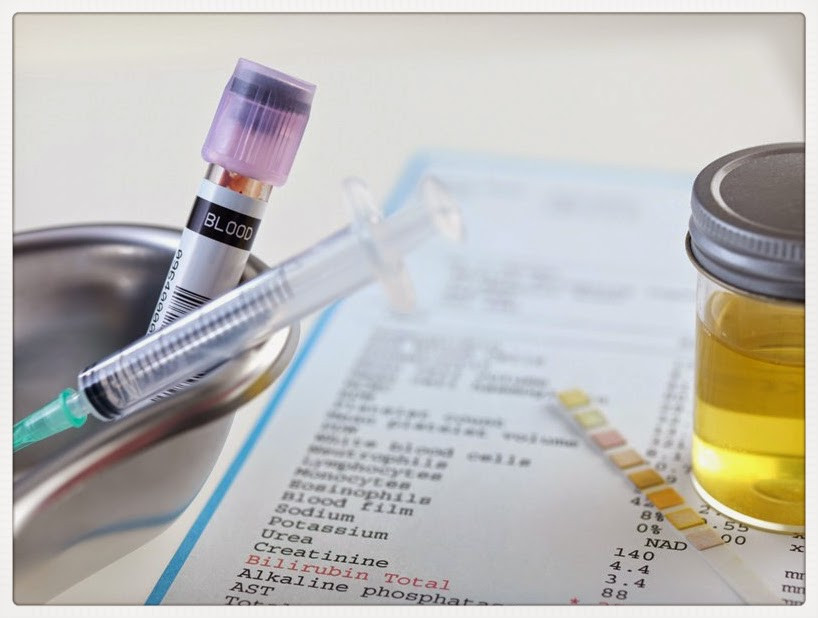
Dokter akan melakukan diagnosa dari anemia hemolitik dengan menanyakan beberapa pertanyaan terkait riwayat kesehatan pasien, terutama bila ada riwayat keluarga yang memiliki anemia. Dokter akan menanyakan apakah memiliki riwayat infeksi tertentu atau sedang mengkonsumsi obat - obatan tertentu yang dapat menyebabkan anemia hemolitik. Dokter akan melakukan pemeriksaan fisik terfokus dengan tanda dan gejala anemia, jaundice, bila adanya pembesaran pada hati atau limfa.
Dokter akan menyarankan melakukan pemeriksaan darah untuk melakukan diagnosa dari anemia hemolitik. Pemeriksaan darah yang dilakukan dapat bersamaan dengan pemeriksaan marker genetik yang dapat menjadi tanda bahwa kondisi genetik menjadi penyebab dari hemolitik anemia.
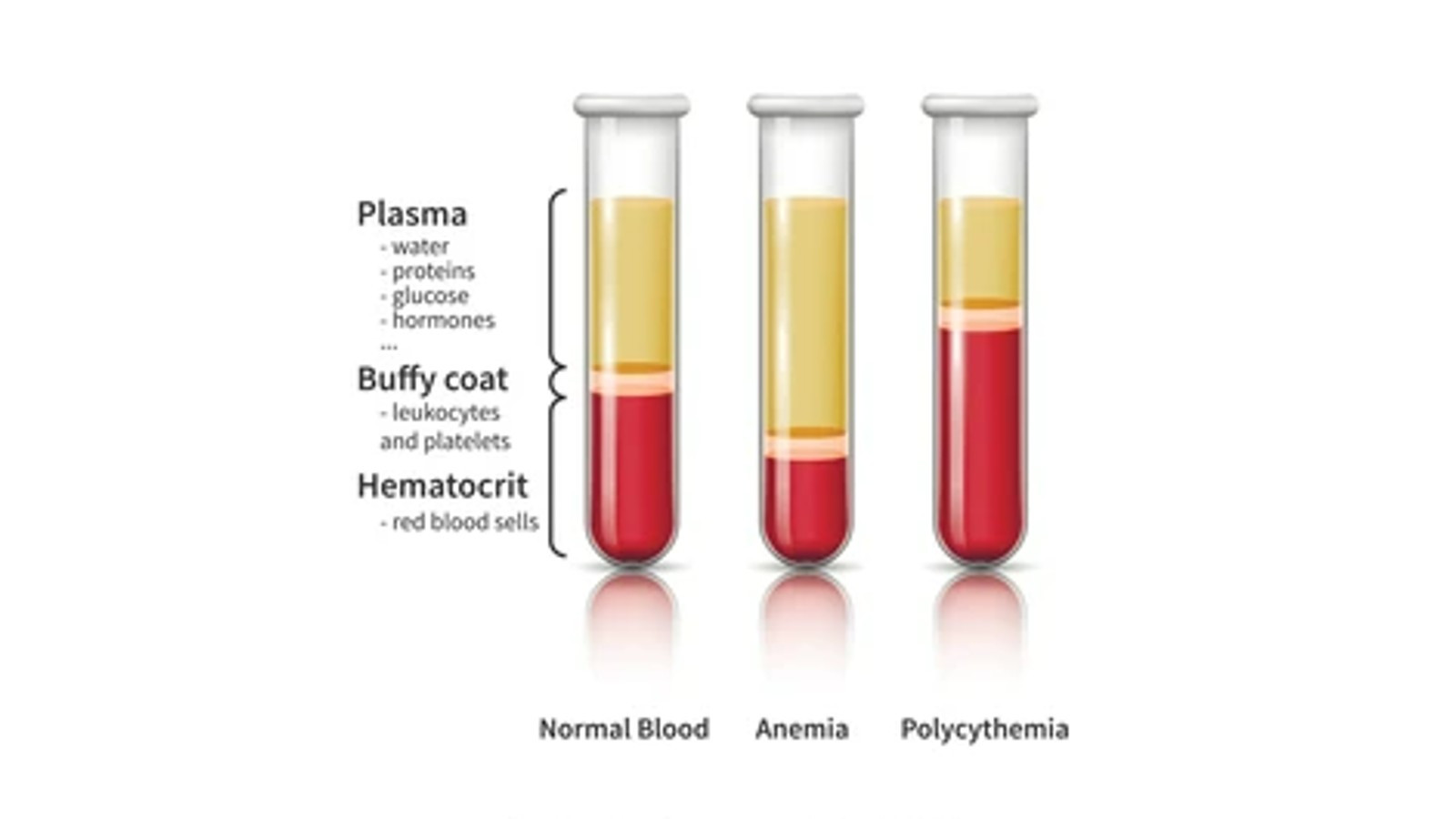
Pada umumnya, dokter akan melakukan pemeriksaan awal untuk menentukan bila gejala disebabkan dari anemia. Pemeriksaan darah lengkap merupakan salah satu pemeriksaan awal. Pemeriksaan darah lengkap yang dilakukan untuk memeriksa jumlah dari sel darah merah, sel darah putih dan keping darah yang anda miliki, ukuran sel darah merah, hemoglobin (Protein di dalam darah yang membawa oksigen ke seluruh tubuh), dan hematokrit dimana mengukur jumlah jeda antara sel darah merah di dalam darah.
Tata Laksana
Dokter akan melakukan pengobatan anemia hemolitik berdasarkan dari gejala dan penyakit penyebab bila memiliki gejala yang berat. Bila dokter memperkirakan anda memiliki anemia yang berat, dokter dapat menyarankan transfusi darah untuk menstabilkan jumlah sel darah merah. Dokter juga akan melakukan diagnosa untuk mencari penyebab dari penyebab anemia sehingga dapat mengobati kondisi sesuai penyebab anemia.
Komplikasi
Anemia hemolitik apabila tidak diobati atau ditangani dengan baik, dapat menyebabkan komplikasi seperti gangguan irama jantung, kelainan otot jantung hingga gagal jantung.
Pencegahan
Anemia hemolitik yang disebabkan oleh faktor genetik tidak dapat dicegah, tetapi individu dapat melakukan konsultasi dengan dokter untuk mengetahui peluang penyakit ini diturunkan pada anak. Bila anemia hemolitik disebabkan oleh efek samping obat - obat, pasien dapat berkonsultasi dengan dokter terkait obat pengganti atau bila perlu menghindari obat yang memicu terjadinya anemia hemolitik.
Anemia hemolitik dapat dicegah dengan mencegah infeksi, seperti menghindari kontak langsung dengan orang yang sedang terkena infeksi, menjauhi kerumunan orang banyak bila memungkinkan, mencuci tangan dan menggosok gigi secara rutin, menghindari makanan mentah atau setengah matang, dan menjalanan vaksinasi flu tiap tahun.
Kapan Harus ke Dokter
Bila mengalami gejala dari anemia hemolitik, segera hubungi ke dokter untuk berkonsultasi lebih lanjut. Bila memiliki riwayat atau keluarga dengan kondisi autoimun atau obat - obat yang memiliki efek samping anemia hemolitik, segera konsultasikan ke dokter dan lakukan pemeriksaan rutin untuk mengawasi dan berkonsultasi tentang penyakit dan efek samping obat tersebut.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr. Pandu Lesmana
Hemolytic Anemia. (2023). Retrieved 13 March 2023, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/hemolytic-anemia
Hemolytic Anemia. (2023). Retrieved 13 March 2023, from https://my.clevelandclinic.org/health/diseases/22479-hemolytic-anemia
Hemolytic Anemia. (2022). Retrieved 13 March 2023, from https://medlineplus.gov/ency/article/000571.htm
Hemolytic Anemia : What It Is and How to Treat It. (2019). Retrieved 13 March 2023, from https://www.healthline.com/health/hemolytic-anemia
What to Know About Hemolytic Anemia. (2022). Retrieved 13 March 2023, from https://www.medicalnewstoday.com/articles/hemolytic-anemia
Hemolytic Anemia. (2022). Retrieved 13 March 2023, from https://emedicine.medscape.com/article/201066-overview