Definition
Idiopathic Thrombocytopenic Purpura (ITP) is a blood disorder characterized by a reduced platelet count, which is vital for stopping bleeding. Thrombocytopenia refers to the lowered platelet levels in the body, while purpura appears as changes in skin color, such as bruises or a purple rash.
This blood disorder can lead to easy bruising or excessive bleeding following injury. Though rare, severe cases may result in complications such as internal organ bleeding.
ITP is a relatively common blood disorder affecting both children and adults. In children, it can develop following a viral infection and may resolve spontaneously. In contrast, the condition in adults often tends to become chronic.
There are two types of ITP based on symptom duration:
Acute ITP
As the name suggests, this condition has a sudden onset, with symptoms typically resolving within a few weeks to no more than 6 months. Acute ITP is most commonly found in children aged 2-6 years and often follows a viral infection, such as chickenpox. Treatment is often unnecessary, and recurrence is rare.
Chronic ITP
This type of ITP can occur at any age, and its symptoms persist longer than acute ITP. Symptoms may last over 6 months, several years, or even a lifetime. Due to its chronic nature, patients often experience relapses and require regular monitoring by a hematologist.
Causes
The normal function of the immune system is to protect the body against foreign substances. However, in some patients with ITP, the immune system mistakenly produces antibodies that attack healthy platelets. In rare cases, a specific type of white blood cell called T cells may directly target platelets, leading to decreased platelet levels.
Several factors or conditions are suspected to trigger this immune response, including:
- Pregnancy
- Certain medications have been linked to decreased platelet levels in some cases
- Infections, particularly viral infections such as chickenpox, influenza, hepatitis C, HIV/AIDS, or the bacterium H. pylori in the stomach
- Autoimmune diseases like rheumatoid arthritis and lupus
- Blood cancers such as leukemia and low-grade lymphoma
It's important to note that in some instances, the exact cause of ITP in patients remains unknown.
Risk factor
In some cases, viral infections can increase the risk of ITP in children. Typically, ITP in children manifests acutely, lasting for less than six months, and often does not recur later. However, chronic ITP, lasting more than six months, is more commonly observed in women than in men.
Symptoms
The normal platelet count typically ranges from 150,000 to 450,000 per microliter of blood. However, in patients with ITP, platelet levels can drop below 100,000. Often, individuals with ITP may not be aware of their condition until they experience difficulty stopping bleeding after an injury. They may also notice an increase in bleeding-related issues.
Although symptoms can vary from person to person, here are some common complaints experienced by individuals with ITP:
- Easy bruising or reddish-purple discoloration on the skin, particularly noticeable around the joints of the elbows and knees, even with minor movement.
- Appearance of small red spots under the skin.
- Nosebleeds or bleeding gums occurring without any obvious cause.
- Heavy menstrual periods in women.
- Presence of blood in urine or stool.
It's important to note that symptoms of ITP can resemble those of other medical conditions. Therefore, it's essential to consult a healthcare provider for an accurate diagnosis.
Diagnosis
The doctor will conduct a comprehensive medical interview and physically examine the patient. During the medical interview, the doctor may inquire about:
- The patient's primary complaints and the duration of their occurrence.
- Previous medical history.
- Family medical history.
- Past treatments.
- Allergies and pregnancies, particularly in women.
A thorough physical examination will involve assessing all vital signs and conducting a head-to-toe examination. Bruising and bleeding on the body will be scrutinized and correlated with the information gathered during the medical interview.
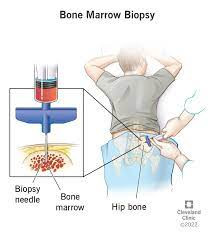
In addition to a detailed medical history and physical examination, the doctor may recommend further tests, such as a complete blood count to assess blood cell levels, especially platelets. Specific antibody tests targeting platelet antigens, or platelet-associated immunoglobulin, may also be conducted, although they are not routinely used for diagnosing ITP. Although uncommon, a bone marrow sample may be obtained to investigate any potential abnormalities in the patient.
Management
Patients with mild ITP may undergo observation with regular blood checks. Children with acute ITP typically show improvement without requiring treatment. Treatment is generally warranted if ITP leads to severe symptoms or persists for an extended period.
Treatment options may involve medication to boost platelet levels in the blood or surgical interventions such as splenectomy, which involves removing the spleen. The spleen often becomes the primary site of platelet destruction due to antibodies in the body. Discussing the risks and benefits of treatment options with your doctor is crucial. Some individuals may find that the treatment's side effects outweigh the disease's effects.
Although rare, severe bleeding can occur in individuals with ITP. Emergency treatment often involves transfusion of platelet concentrate. Steroids and immunoglobulins may also be administered as emergency measures.
Doctors will provide guidance on preventive measures to minimize the risk of injury and excessive bleeding, including:
- Creating the safest possible environment for young children, such as lining the baby's bed, ensuring they wear helmets, and providing protective clothing to reduce the likelihood of injury.
- Considering restrictions on activities involving physical contact, riding bicycles, and rough play.
It's essential to consult with a pediatrician to determine any additional precautions necessary to prevent injury in children with ITP.
Complications
The most severe complication of ITP is bleeding. Head injuries or internal organ injuries can be particularly dangerous as they may lead to prolonged bleeding and potentially life-threatening situations.
Prevention
There's no known way to prevent ITP, but you can take several steps to minimize complications from the disease:
- Avoid sports involving physical contact. Depending on your risk of bleeding, head collisions during activities like boxing, martial arts, and soccer could potentially lead to brain bleeding. Discuss safe activities with your doctor.
- Exercise caution with over-the-counter medications. Excessive use of non-prescription drugs may lead to dangerous side effects.
When to see a doctor?
Schedule an appointment with your doctor if you or your child experience excessive bruising or bleeding without an apparent cause.
Looking for more information about other diseases? Click here!
- dr Hanifa Rahma
John Hopkins - Idiopathic Thrombocytopenic Purpura (2022). Retrieved 31 March 2023, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/idiopathic-thrombocytopenic-purpura#.
Mayo Clinic - Immune Thrombocyropenic Purpura (2021). Retrieved 31 March 2023, from https://www.mayoclinic.org/diseases-conditions/idiopathic-thrombocytopenic-purpura/symptoms-causes/syc-20352325.
Medscape - Immune Thrombocytopenic Purpura (2023). Retrieved 31 March 2023, ftom https://emedicine.medscape.com/article/202158-overview.