Definisi
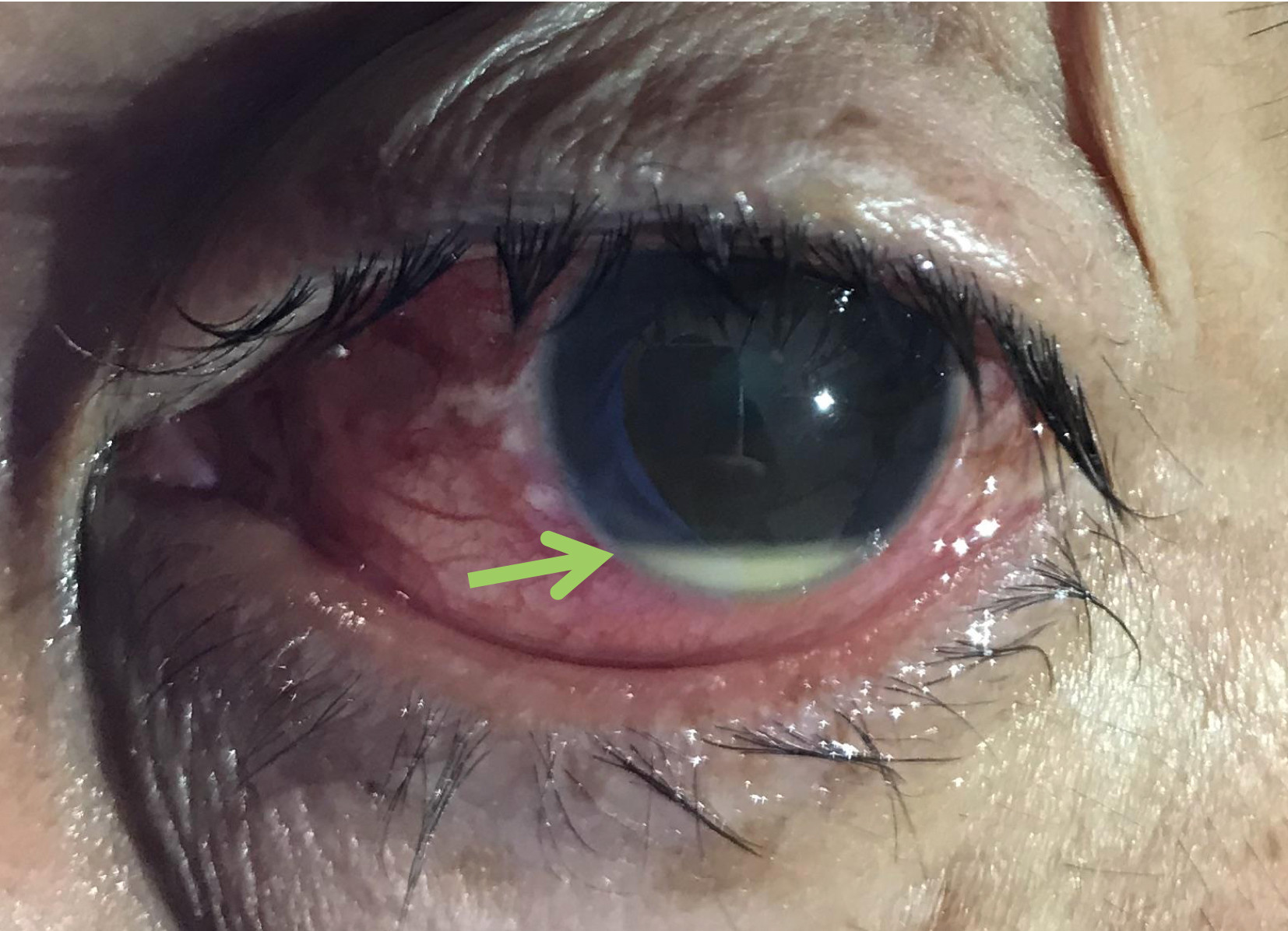
Hipopion merupakan pengumpulan sel darah putih pada Bilik Mata Depan (BMD). Hipopion bukan merupakan diagnosis namun merupakan gejala dari inflamasi atau peradangan berat pada struktur mata lainnya. Jika Anda mengalami kondisi ini, Anda dapat melihat adanya cairan putih pada bagian hitam mata Anda ketika bercermin.
Penyebab
Hipopion dapat disebabkan oleh kondisi infeksi atau non infeksi. Kondisi infeksi yang dapat menyebabkan hipopion antara lain:
- Peradangan seluruh lapisan mata (endoftalmitis)
- Peradangan pada kornea (Keratitis)
- Infeksi toxoplasma
- Infeksi sifilis
- Infeksi HSV
Kondisi non infeksi yang dapat menyebabkan hipopion antara lain:
- HLA-B26
- Behçet disease
- Spondiloartropati
- Keganasan/trauma/prosedur medis
Pada kondisi non infeksi, umumnya hipopion yang terjadi diakibatkan oleh peradangan pada lapisan uvea yang disebut uveitis anterior. Berikut akan dibahas mengenai kondisi yang paling sering menyebabkan hipopion, antara lain adalah keratitis, endoftalmitis, dan uveitis anterior.
Keratitis
Keratitis atau peradangan pada kornea dapat disebabkan oleh bakteri, seperti P. aeruginosa, S. aureus, S. pneumoniae, dan Enetrobacteriaceae. Bakteri ini dapat merusak kornea dan membuat rongga pada lapisan kornea yang mengganggu penglihatan. Agen lain yang dapat menyebabkan keratitis adalah virus, antara lain Herpes simplex dan varicella-zoster virus. Radang yang hebat dapat menyebabkan sel-sel darah putih yang bertujuan untuk menangani peradangan tersebut keluar dari pembuluh darah dan menetap di BMD. Keratitis yang lebih sering menyebabkan hipopion adalah keratitis yang disebabkan oleh jamur (keratitis jamur).
Endoftalmitis
Endoftalmitis merupakan kondisi peradangan pada lapisan bola mata dan rongga bola mata, termasuk vitreous humor, cairan yang berada di balik iris. Penyebab endoftalmitis utamanya adalah infeksi, namun juga dapat disebabkan oleh kondisi non infeksi (endoftalmitis endogen). Dalam kondisi normal, sawar darah-mata dapat memberikan perlindungan pada bola mata dari agen patogen yang dapat merusak. Namun pada beberapa kondisi seperti rusaknya integritas jaringan mata, operasi, keganasan, dapat merusak lapisan tersebut sehingga infeksi dapat menyebar. Endoftalmitis dapat menyebabkan kebutaan permanen.
Uveitis Anterior
Uveitis adalah peradangan yang terjadi pada lapisan uvea bola mata. Iris merupakan salah satu lapisan uvea yang berada pada sisi depan (anterior). Uveitis anterior merupakan kondisi peradangan pada lapisan uvea yang berada di depan, seperti iris dan badan siliar. Peradangan pada struktur ini dapat disebabkan oleh kondisi autoimun, genetik, trauma, dan infeksi; namun paling sering disebabkan oleh kondisi autoimun atau tidak diketahui sama sekali. Kondisi autoimun yang berkaitan dengan uveitis anterior adalah SLE (4.8%), arthritis reumatoid juvenil (5.6%), dan sarkoidosis (9.6%).
Faktor Risiko
Faktor risiko dari hipopion bergantung pada penyakit yang mendasarinya. Misalnya sebagai berikut:
Keratitis
- Penggunaan lensa kontak
- Trauma bola mata
- Operasi mata sebelumnya
- Mata terpapar dengan bahan organik, seperti tumbuhan, padi, ilalang
- Imunitas yang sedang turun
- Penggunaan kortikosteroid
Endoftalmitis
- Trauma bola mata
- Penanganan trauma yang tidak steril
- Ruptur lensa
- Usia >50 tahun
- Datang ke dokter setelah 24 jam pascatrauma
- Pascaoperasi katarak
Uveitis Anterior
- Memiliki penyakit autoimun
- Memiliki riwayat keluarga dengan uveitis anterior atau penyakit autoimun lainnya
Gejala
Jika Anda mengalami hipopion, Anda dapat melihat adanya benda atau cairan putih pada bagian hitam mata Anda ketika Anda bercermin. Hipopion merupakan salah satu gejala dari penyakit lainnya, sehingga gejala yang menyertai hipopion bergantung pada penyakit tertentu.
Keratitis
Selain hipopion, Anda dapat mengalami:
- Mata merah
- Mata terasa nyeri
- Mata berair terus menerus
- Sekret atau cairan mata kental berwarna putih, kuning, atau kehijauan
- Pandangan buram dan tidak membaik dengan apapun
- Nyeri ketika melihat cahaya
- Merasa ada benda asing pada mata Anda
Endoftalmitis
Selain hipopion, Anda dapat mengalami:
- Buram mendadak, bisa hingga tidak dapat melihat cahaya
- Mata merah
- Nyeri berat pada mata
- Kelopak mata bengkak
- Mata berair
- Tidak dapat melihat cahaya
Uveitis Anterior
Selain hipopion, Anda dapat mengalami:
- Mata merah
- Pandangan buram
- Melihat titik-titik hitam
- Sensitif terhadap cahaya
Diagnosis
Dokter akan melakukan pemeriksaan pada keluhan hipopion Anda. Dokter Anda akan mencari tahu mengenai sejak kapan hipopion tersebut muncul, apa hal yang mengawali munculnya hipopion, dan faktor risiko yang berkaitan dengan penyakit yang mendasari hipopion, seperti keratitis, endoftalmitis, dan uveitis anterior. Dokter Anda juga akan mencari tahu mengenai ada atau tidaknya penurunan ketajaman penglihatan dan agen infeksius atau non infeksius yang menyebabkan penyakit dasar dari hipopion tersebut. Dokter juga akan menanyakan mengenai penyakit autoimun yang mungkin Anda atau keluarga Anda alami, riwayat operasi bola mata, obat-obatan yang Anda konsumsi, dan riwayat trauma pada mata. Pada pemeriksaan fisis, dokter Anda akan melakukan pemeriksaan terhadap ketajaman penglihatan (visus) dan kondisi bola mata Anda dengan menggunakan slit lamp atau funduskopi. Jika dibutuhkan, Dokter akan melakukan pemeriksaan fluorescein untuk melihat adanya kerusakan pada kornea Anda. Jika dokter Anda mencurigai adanya penyakit sistemik yang mendasari kondisi Anda, dokter Anda akan melakukan pemeriksaan darah lengkap, pemeriksaan urin, pemeriksaan radiologi toraks, dan pemeriksaan penyebab infeksi lainnya.
Tata Laksana
Pengobatan hipopion bergantung pada penyakit yang mendasarinya.
Keratitis
- Keratitis non infeksi, contohnya pada goresan kornea akibat gesekan, pengobatan yang dilakukan adalah observasi dan air mata buatan. Namun jika kondisi keratitis menyebabkan nyeri dan mata berair, penutupan mata dengan patch selama 24 jam dapat dilakukan
- Pada keratitis infeksi, pengobatan bergantung pada penyebabnya:
- Keratitis bakteri, dilakukan pemberian antibiotik tetes atau antibiotik oral jika berat
- Keratitis jamur/fungi, pemberian antijamur
- Keratitis virus, diberikan antijamur tetes mata dan obat antivirus oral
- Jika kondisi keratitis tidak membaik dengan pemberian pengobatan tersebut dan penglihatan sangat terganggu, transplantasi kornea dapat dilakukan
Endoftalmitis
Pengobatan endoftalmitis bergantung pada bagian yang mana yang mengalami infeksi. Antibiotik dapat diberikan dengan menginjeksikan langsung ke bola mata dengan jarum kecil. Kortikosteroid dapat ditambahkan jika terdapat pembengkakan. Jika terdapat benda asing pada mata, dokter Anda akan mengeluarkan benda asing tersebut. Jangan mengeluarkannya sendiri dan segera kunjungi fasilitas kesehatan terdekat. Pengobatan untuk menatalaksana endoftalmitis umumnya bersifat operatif dan dilakukan oleh dokter spesialis mata.
Uveitis Anterior
Pengobatan yang akan diberikan antara lain:
- Obat-obatan untuk menurunkan inflamasi, seperti kortikosteroid
- Obat untuk mengendalikan spasme, dengan cara melebarkan pupil untuk menurunkan nyeri
- Antibiotik, jika kondisi tersebut disebabkan oleh bakteri
Pengobatan tersebut dapat menyebabkan kondisi mata lain, seperti glaukoma. Selain terapi medis, terapi operatif seperti vitrektomi dapat dilakukan.
Komplikasi
Komplikasi dari hipopion bergantung pada penyakit yang mendasarinya.
- Keratitis dapat menyebabkan ulserasi kornea yang dapat menurunkan kemampuan penglihatan secara permanen. Glaukoma, sinekia (penempelan iris ke lensa atau ke kornea), glaukoma, endoftalmitis, dan katarak juga dapat terjadi.
- Endoftalmitis dapat menyebabkan hilangnya penglihatan secara permanen. Pada kondisi yang parah, enukleasi (pengeluaran atau ekstraksi bola mata) perlu dilakukan untuk mencegah infeksi berkelanjutan
- Jika uveitis anterior tidak ditangani, pembengkakan retina, glaukoma, katarak, kerusakan nervus optik, ablasio retina, kehilangan penglihatan permanen dapat terjadi
Pencegahan
- Bersihkan lensa kontak Anda secara berkala, tidak menggunakan lensa kontak ketika tidur, dan pastikan tangan Anda bersih sebelum menggunakan lensa kontak
- Ganti lensa kontak Anda setiap 3–6 bulan sekali
- Jangan menggunakan lensa kontak ketika berenang
- Hanya gunakan obat-obatan yang diresepkan dokter
- Cuci tangan dengan 5 langkah WHO sebelum menyentuh mata
- Gunakan pelindung mata saat Anda melakukan pekerjaan yang dapat menyebabkan trauma mata, seperti ketika memotong kayu, menggunakan las, atau berolahraga. Pelindung mata yang dapat digunakan antara lain adalah googles, eye shields, dan helm.
- Jika Anda baru saja melakukan operasi mata, lakukan instruksi postoperatif dari dokter Anda
Kapan Harus ke Dokter?
Jika Anda mengalami kondisi berikut, segera periksakan diri Anda ke fasilitas kesehatan terdekat.
- Anda mengalami hipopion
- Tanda keratitis, endoftalmitis, dan uveitis
- Penurunan penglihatan secara mendadak
- Mengalami mata merah, nyeri dan penurunan penglihatan mendadak setelah operasi katarak atau trauma bola mata
- Anda memiliki penyakit autoimun dan mengalami penurunan penglihatan
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Ayu Munawaroh, MKK
Muchatuta MN. (2019). Iritis and Uveitis. Medscape. Retrieved 08 November 2021, from https://emedicine.medscape.com/article/798323-overview#a1.
Egan DJE. (2018). Endophthalmitis. Medscape. Retrieved 08 November 2021, from https://emedicine.medscape.com/article/799431-overview#a4.
Ross M. (2019). Fungal Keratitis. Medscape. Retrieved 08 November 2021, from https://emedicine.medscape.com/article/1194167-overview#a4.
MayoClinic. (2020). Uveitis. MayoClinic. Retrieved 08 November 2021, from https://www.mayoclinic.org/diseases-conditions/uveitis/diagnosis-treatment/drc-20378739.
MayoClinic. (2020). Keratitis. MayoClinic. Retrieved 08 November 2021, from https://www.mayoclinic.org/diseases-conditions/keratitis/diagnosis-treatment/drc-20374114.
McBean B. (2018). What is endophthalmitis?. Healthline. Retrieved 08 November 2021, from https://www.healthline.com/health/endophthalmitis.