Definition
Diverticulosis is the formation of pockets in the wall of the gastrointestinal tract. These pockets are called diverticula and are created in weakened areas of the intestine wall due to pressure on the inner layer. The pressure causes the intestinal wall to protrude outward, forming small pockets. The size of the diverticula varies, ranging from the size of a peanut to larger sizes. Although diverticula can form in all layers of the large intestine, diverticulosis predominantly occurs in the rectum area. The rectum, located at the bottom of the large intestine, has a shape resembling the letter "S."
Diverticulosis is distinct from diverticulitis. Diverticulitis occurs when one or more pockets become inflamed or infected. This results in swelling, abdominal pain, nausea, and fever. Prompt treatment is necessary to reduce the spread of infection. In contrast, diverticulosis typically presents no symptoms and does not require treatment. Adopting a healthy lifestyle and maintaining a high-fibre diet is usually sufficient to prevent the inflammation of diverticulitis or other complications.
Diverticulosis is commonly found in Western countries, with 10% of affected individuals older than 40 and 50% older than 60. The incidence of diverticulosis increases with age and is almost always found in individuals over 80.
Causes
At present, the exact cause of diverticulosis is not fully understood. Previously, it was hypothesized that diverticulosis might be associated with a fiber shortage, primarily found in vegetables, fruits, nuts, and grains.
A reduced intake of fiber can lead to constipation. Hard stools that are difficult to pass can accumulate in the bowel, exerting pressure on the intestine. This increased pressure can form small pockets in the weakened areas of the intestinal wall.
Risk Factor
Some risk factors for diverticulosis include:
- Age: Diverticulosis is common in people over 60 years old and rare in those under 30. Experts believe that the likelihood of developing pockets increases with age
- Male gender
- Overweight
- Low-fiber diet
- High-fat and red meat diet
- Lack of regular exercise
- Incorrect use of anti-inflammatory drugs
- Smoking
- Family history: Some research suggests a possible genetic factor in diverticulosis. If a family member (parent or sibling) has diverticulosis, the risk is higher.
Symptoms
Most individuals affected by diverticulosis experience no symptoms. For those who do, common symptoms include:
- Abdominal pain or cramps
- Bloated stomach
- Constipation
- Diarrhea
The onset of symptoms does not necessarily mean that the individual has diverticulosis. Other conditions, such as irritable bowel syndrome, stomach ulcers, appendicitis, and other gastrointestinal tract disorders, can cause similar symptoms. Therefore, physicians need to exclude other potential causes.
Diagnosis
Most doctors may not initially identify diverticulosis in a patient. It is often discovered incidentally during examinations for other diseases. Doctors typically conduct a complete examination to confirm the diagnosis if diverticulosis is suspected or found.
First, the physician will inquire about the patient's complaints and medical history, including dietary habits, previous illnesses, medications taken, and defecation patterns. Following this, a physical examination will be conducted. This may include a rectal touch examination, where the doctor examines the inner wall of the rectum using a lubricated finger. During this examination, the doctor checks for signs of blood, pain, or other abnormalities.
To confirm the diagnosis, the doctor may also perform various tests, including:
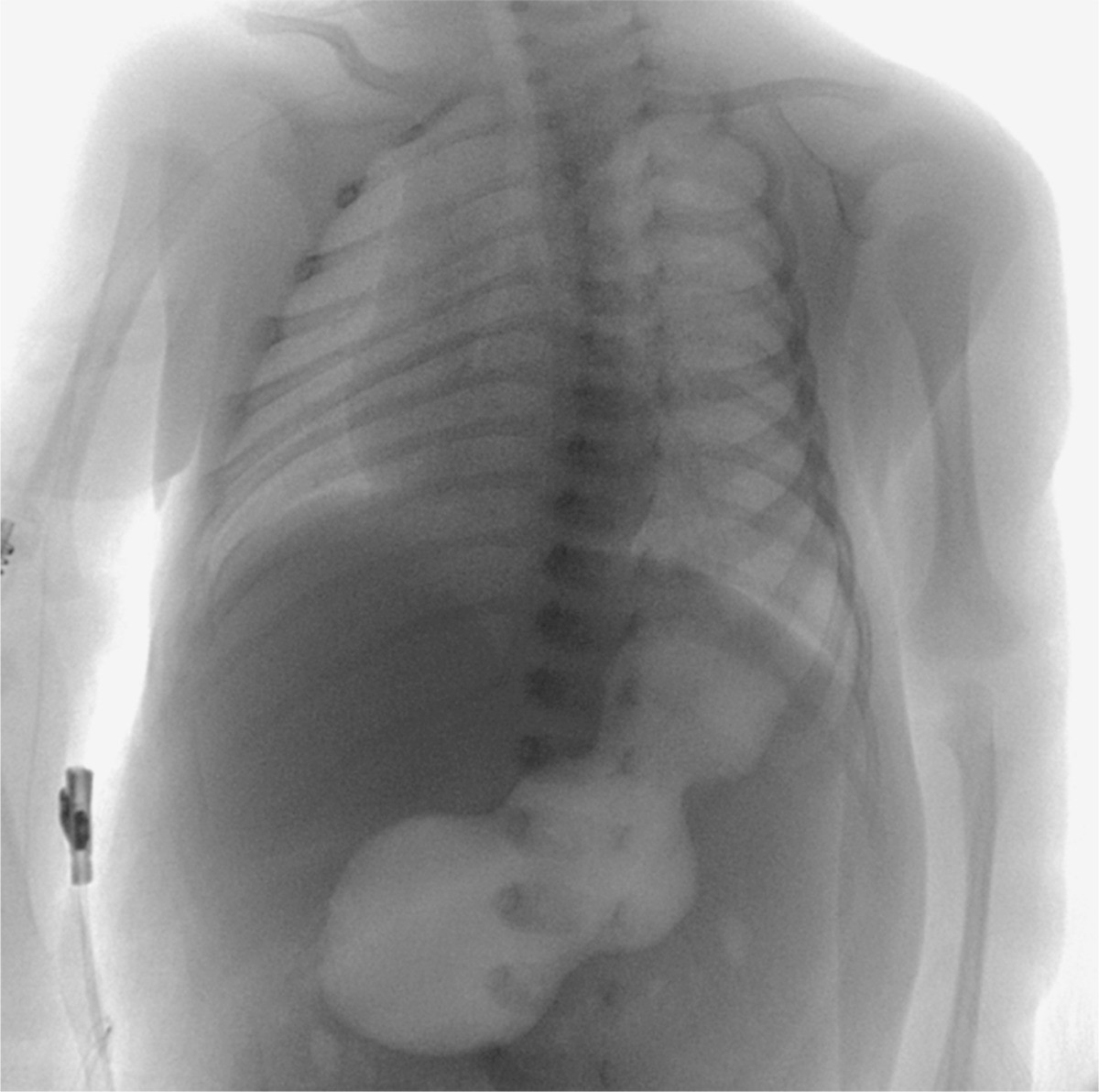
- CT scan to provide images of the gastrointestinal tract
- Colonoscopy: to visually assess the condition of the bowel
- Blood tests: to check for signs of infection or anemia
- Serial X-rays: to examine the lower gastrointestinal tract
Management
If you have diverticulosis, it is often without symptoms and may not require treatment. However, as diverticulosis can worsen and progress to diverticulitis, a high-fiber diet is recommended as a preventive measure. The primary goal of treatment is to prevent complications such as inflammation or infection of the diverticular pockets. To achieve this, the doctor may recommend:
- High-fiber diet or fiber supplements: The type of diet depends on your fiber needs. Consuming high-fiber foods can help reduce gas and abdominal pain. The doctor may recommend fiber products like Citrucel or Metamucil, which are available in pills, powder, or wafer form. It's important to consume fiber with adequate water intake.
- Medications to reduce symptoms
- Probiotics: These are beneficial bacteria that live in the intestines. While research on probiotics is limited, some studies suggest that they may help alleviate the symptoms of diverticulosis. Consult with your physician before taking supplements.
Complications
Some complications of diverticulosis include:
- Infected or burst pockets: An infected or inflamed pocket is called diverticulitis. Infection occurs when bacteria in feces accumulate and fill the diverticular pocket. If the pocket wall erodes due to continuous pressure, it may burst and become easily infected. Diverticulitis can be treated with bed rest, fluid therapy, and antibiotics
- Spread of infection leading to abscess formation: An abscess is a pocket containing pus. To treat the abscess, a doctor needs to drain the pus
- Perforation in the abdominal wall: Although rare, this complication can be life-threatening and requires immediate surgery if it occurs
- Diverticular bleeding: This complication is rare and results from bursting an artery in the intestinal wall. It can lead to massive bleeding, requiring blood transfusions and hospitalization
Prevention
Currently, diverticulosis is more commonly diagnosed than 100 years ago. This increase is attributed to modern diets high in processed carbohydrates and lower in the necessary fiber, which plays a significant role in the incidence of diverticulosis.
To reduce the risk factors mentioned earlier, preventive measures can be taken. Recommended dietary changes include a balanced diet with low-fat, low-processed carbohydrates and high fiber content. High-fiber diets can be derived from vegetables, fruits, nuts, or grains. Fiber helps draw water into the feces, making them softer and easier to pass. A smooth stool passage pattern can reduce the likelihood of diverticulosis.
A high-fiber diet may also increase water absorption by the feces, necessitating an adequate water intake to keep stools soft and easy to pass. Drinking at least 2 liters, or around eight glasses, of water daily is recommended. For approximately 30 minutes daily, regular exercise can contribute to overall health and facilitate stool passage.
When to See a Doctor?
It is necessary to consult a doctor when:
- Experiencing persistent abdominal pain that cannot be explained by other causes, especially if accompanied by fever or changes in stool patterns such as constipation or diarrhea
- Experiencing recurrent or worsening symptoms
- Observing blood in the stool
- dr Ayu Munawaroh, MKK
What is diverticulosis?. (2021). Retrieved 17, 2022, from https://www.webmd.com/digestive-disorders/what-is-diverticulosis
Diverticulosis and diverticulitis of the colon. (2020). Retrieved 17, 2022, from https://my.clevelandclinic.org/health/diseases/10352-diverticular-disease
Nallapeta NS, Farooq U, and Patel K. (2020). Diverticulosis. Retrieved 24, 2022, from https://www.ncbi.nlm.nih.gov/books/NBK430771