Definisi
Gagal hati adalah kehilangan fungsi hati. Gagal hati dapat terjadi secara cepat/akut atau secara lambat/kronik. Gagal hati akut dapat terjadi selama beberapa hari atau minggu, paling cepat 48 jam. Sementara itu, gagal hati kronik biasanya terjadi akibat penyakit hati yang sudah berlangsung selama bertahun-tahun.
Penyebab
Gagal hati akut dan kronik memiliki penyebab yang berbeda. Gagal hati akut dapat disebabkan oleh dosis parasetamol yang terlalu tinggi, obat-obatan yang diresepkan dokter, suplemen herbal, hepatitis dan virus lainnya, toksin, penyakit autoimun, gangguan pembuluh darah di hati, penyakit metabolik, kanker, syok, dan heat stroke.
Gagal hati akut yang disebabkan oleh parasetamol dapat terjadi karena mengonsumsi obat tersebut dalam dosis yang terlalu banyak satu kali, atau dosis yang melebihi normal selama beberapa hari. Sementara itu, obat-obatan resep dokter yang dapat menyebabkan gagal hati akut dapat berupa antibiotik, antinyeri, dan antikejang. Suplemen herbal yang sudah diketahui terkait dengan gagal hati akut adalah kava, efedra, skullcap, dan pennyroyal.
Virus-virus yang dapat menyebabkan gagal hati akut dapat berupa virus hepatitis A, B, dan E, serta virus Epstein-Barr, sitomegalovirus, dan virus herpes simpleks. Toksin yang dapat menyebabkan gagal hati akut di antaranya adalah toksin dari jamur Amanita phalloides, serta karbon tetraklorida, yang ditemukan pada pendingin, lilin, dan pernis.
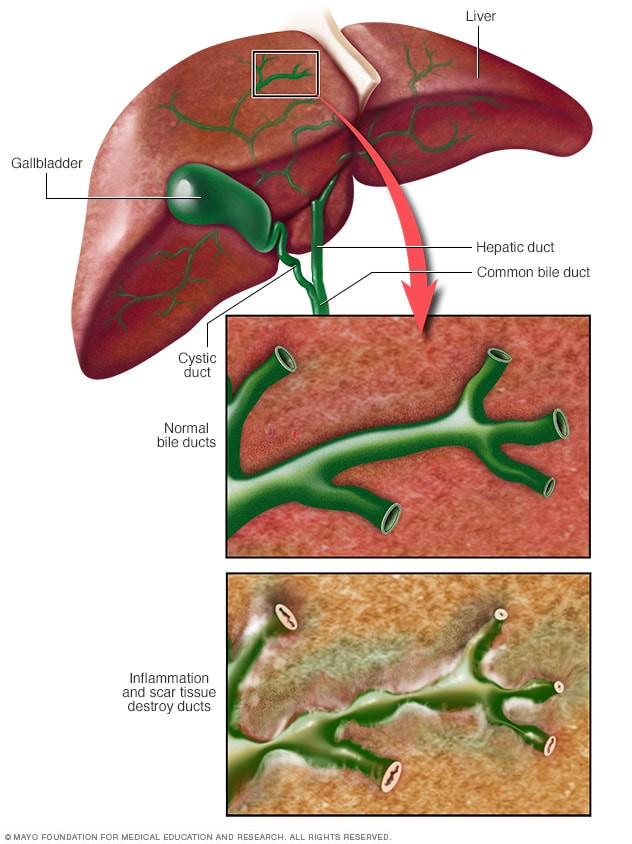
Penyakit yang dapat menyebabkan gagal hati akut dapat berupa hepatitis autoimun, yaitu kondisi ketika sel kekebalan tubuh menyerang sel-sel hati, penyakit Wilson, serta perlemakan hati akut saat kehamilan. Syok yang dapat menyebabkan gagal hati adalah syok berupa kegagalan organ, misalnya akibat infeksi hebat (sepsis). Heat stroke adalah sebuah kondisi ketika seseorang melakukan aktivitas fisik yang ekstrem pada cuaca panas.
Sementara itu, gagal hati kronik biasanya merupakan hasil dari sirosis atau pengerasan hati. Sirosis dapat disebabkan oleh penggunaan alkohol jangka panjang, hepatitis B, hepatitis C, dan hemokromatosis atau penyakit bawaan yang menyebabkan kadar besi di hati terlalu tinggi.
Faktor Risiko
Faktor risiko gagal hati sangat tergantung dari penyebabnya. Misalnya, hepatitis E dan penyakit hati autoimun lebih sering terjadi pada wanita dibandingkan pria. Sementara itu, hepatitis B dan C banyak terjadi pada orang-orang yang memiliki riwayat transfusi darah, penggunaan jarum suntik untuk obat-obatan resep ataupun obat-obatan terlarang, orang bertato, orang yang memiliki pasangan seksual lebih dari satu, tenaga kesehatan yang berurusan dengan cairan tubuh pasien, dan sebagainya. Selain itu, konsumsi alkohol berlebih juga dapat menjadi faktor risiko gagal hati, terutama gagal hati kronik. Gagal hati yang disebabkan oleh penyakit bawaan seperti penyakit Wilson dapat pula diketahui dari riwayat penyakit keluarga.
Gejala
Gejala gagal hati akut dapat berupa kuning pada kulit dan bagian putih bola mata (sklera), nyeri pada perut bagian kanan atas, gejala saluran cerna lain seperti mual atau muntah dan penurunan nafsu makan, pembengkakan perut yang berisi cairan, pembengkakan kaki, rasa tidak enak badan (malaise), bingung atau disorientasi, mengantuk, napas berbau apek, tremor atau getaran pada anggota gerak tubuh yang terjadi tanpa disadari, mudah berdarah terutama pada lambung, perdarahan saluran cerna atas dapat bermanifestasi dengan gejala muntah darah atau tinja berwarna hitam pekat, serta diare.
Gejala gagal hati kronik biasanya baru muncul apabila stadium penyakit sudah cukup parah untuk menyebabkan gejala.
Diagnosis
Diagnosis gagal hati dimulai dari pertanyaan mengenai onset atau kapan gejala muncul. Dokter dapat menanyakan berbagai faktor risiko terkait gagal hati untuk menentukan apakah gagal hati terjadi secara akut atau kronik, misalnya seperti riwayat penggunaan alkohol, penggunaan obat-obatan baik obat resep dokter atau obat-obatan terlarang, penggunaan obat herbal, riwayat keluarga dengan penyakit serupa, faktor risiko hepatitis seperti perjalanan ke daerah endemis, transfusi darah, kontak seksual, pekerjaan, dan tindik, serta racun hati seperti jamur, pelarut organik, dan fosfor pada kembang api.
Pemeriksaan langsung kepada penderita juga dapat dilakukan oleh dokter untuk mencari adanya kuning, nyeri pada perut bagian kanan atas, tekanan darah tinggi disertai denyut nadi lambat, pembengkakan perut dan kaki, serta adanya muntah darah atau BAB hitam.
Pemeriksaan laboratorium memiliki peran yang sangat penting untuk menegakkan diagnosis, mencari komplikasi, dan memerkirakan tingkat kesembuhan penderita. Pemeriksaan ini dapat mencakup pemeriksaan darah lengkap untuk melihat jumlah trombosit, pemeriksaan pembekuan darah, enzim hati, bilirubin, amonia serum, gula darah, laktat, analisis gas darah, kreatinin, fosfat, penanda autoimun seperti antinuclear antibodies (ANA), kadar parasetamol, serta toksikologi obat-obatan terlarang.
Selain itu, pemeriksaan untuk mengetahui adanya infeksi virus juga dapat dilakukan dengan pemeriksaan antigen-antibodi. Kultur darah dapat pula dilakukan apabila penderita dicurigai mengalami infeksi bakteri. Apabila ada kecurigaan terhadap penyakit hati autoimun, kanker pada hati atau pada bagian tubuh lainnya, serta infeksi virus herpes simpleks, pengambilan jaringan hati dapat dilakukan.
Pemeriksaan pencitraan ultrasonografi (USG) dapat dilakukan untuk mencari penumpukan cairan di perut serta melihat bentuk pembuluh darah hati. Pemeriksaan computed tomography scan (CT scan) juga dapat membantu melihat bentuk hati serta adanya massa atau tumor di sekitar hati. Tidak hanya itu, CT scan dapat pula dilakukan pada kepala, untuk mencari adanya perdarahan di dalam kepala yang sama-sama dapat menyebabkan penurunan kesadaran, seperti halnya gagal hati akut yang dapat menyebabkan kerusakan otak.
Tata Laksana
Gagal hati, terutama akut, merupakan kondisi kegawatdaruratan. Apabila penderita datang dalam keadaan tidak sadar atau koma, tenaga kesehatan akan berusaha menjaga agar jalan napas tetap terbuka dengan bantuan selang napas (intubasi). Selain itu, pemasangan selang makan dapat dilakukan untuk menurunkan tekanan pada lambung dan memberikan makan kepada penderita.
Apabila penderita sadar, pengobatan yang dilakukan dapat bervariasi tergantung penyebab gagal hati. Misalnya, apabila gagal hati disebabkan oleh keracunan parasetamol, jamur, dan sebagainya, obat-obatan tertentu dapat diberikan sebagai penangkal racun tersebut. Apapun penyebab gagal hatinya, sangat mungkin penderita memerlukan perawatan intensif di unit intensif (intensive care unit, ICU).
Apabila sisa bagian hati yang masih dapat bekerja tinggal sedikit, dokter dapat menyarankan Anda untuk menjalani transplantasi hati. Namun, prosedur ini hanya dapat dilakukan di pusat rujukan nasional di Indonesia.
Komplikasi
Komplikasi gagal hati dapat berupa pembengkakan otak akibat penumpukan cairan. Penumpukan cairan ini terjadi karena pembuluh darah hati menyempit, dan dapat terjadi pada otak, perut, dan kaki. Namun, yang paling berbahaya adalah otak, karena dapat mematikan. Selain itu, komplikasi lainnya adalah gangguan pembekuan darah, karena banyak faktor pembekuan darah yang dihasilkan oleh hati. Selain itu, infeksi seperti pada paru (pneumonia) dan saluran kemih seringkali terjadi karena sistem kekebalan tubuh yang menurun. Tidak hanya itu, gagal hati juga memengaruhi kerja ginjal sehingga gagal ginjal dapat terjadi sebagai komplikasi.
Pencegahan
Pencegahan gagal hati dapat dilakukan dengan berbagai langkah sebagai berikut:
- Ikuti anjuran dosis yang tertera pada obat, misalnya pada kertas yang ada bersama dengan bungkus obat.
- Sebutkan seluruh obat-obatan Anda kepada dokter, karena pengobatan tanpa resep dan herbal dapat berinteraksi dengan obat resep dokter
- Batasi atau hindari minum alkohol, maksimal 1 gelas per hari untuk perempuan dan 2 gelas per hari untuk laki-laki
- Hindari tindakan berisiko seperti penggunaan obat-obatan terlarang, penggunaan jarum suntik bersama, berhubungan seks tanpa kondom. Berhati-hatilah ketika hendak menato atau menindik tubuh, cari tempat yang bersih dan aman
- Vaksinasi virus hepatitis
- Hindari kontak dengan darah atau cairan tubuh orang lain, misalnya dengan menghindari penggunaan jarum suntik, pisau cukur, dan sikat gigi bersama
- Jangan memakan jamur liar, karena sulit untuk membedakan jamur yang beracun dan tidak beracun
- Hati-hati dalam menggunakan semprotan aerosol seperti pembunuh serangga, pembunuh jamur, cat, dan bahan kimia beracun lainnya. Pastikan ruangan memiliki aliran udara yang baik
- Awasi cairan yang menyentuh tubuh Anda. Saat menggunakan pembunuh serangga, misalnya, lindungi kulit Anda dengan sarung tangan, baju berlengan panjang, topi, dan masker
- Jaga berat badan ideal karena obesitas dapat menyebabkan perlemakan hati, yang selanjutnya dapat menyebabkan gagal hati kronik
Kapan Harus ke Dokter?
Segeralah ke dokter apabila Anda atau orang di sekitar Anda tiba-tiba kuning pada kulit atau matanya, mengalami nyeri pada perut bagian kanan atas, serta tiba-tiba mengalami gangguan kesadaran seperti mengantuk, mengamuk, atau koma. Kecurigaan terhadap gagal hati semakin kuat apabila orang tersebut memiliki riwayat penyakit hati, obesitas, mengonsumsi alkohol berlebih, atau menggunakan obat-obatan terlarang secara rutin.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Hanifa Rahma
Acute liver failure - Symptoms and causes. (2020). Retrieved 12 January 2022, from https://www.mayoclinic.org/diseases-conditions/acute-liver-failure/symptoms-causes/syc-20352863
Begum, J. (2021). Information on Liver Failure. Retrieved 12 January 2022, from https://www.webmd.com/digestive-disorders/digestive-diseases-liver-failure
Sood, G. (2019). Acute Liver Failure: Practice Essentials, Background, Pathophysiology. Retrieved 12 January 2022, from https://emedicine.medscape.com/article/177354-overview
Wu, B., & Sethi, S. (2018). What You Need to Know About Hepatic Failure (Liver Failure). Retrieved 12 January 2022, from https://www.healthline.com/health/hepatic-failure#treatment