Definisi
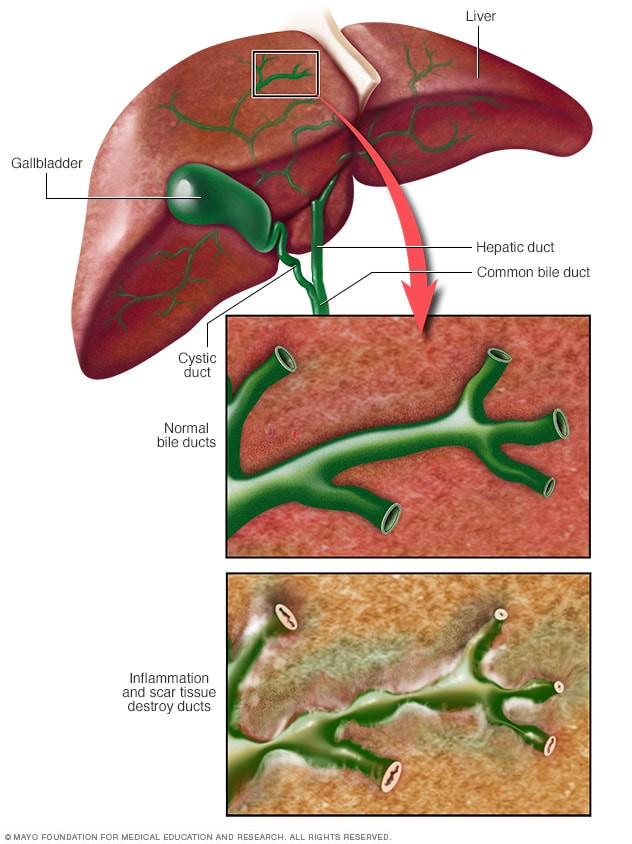
Sirosis bilier primer adalah penyakit hati yang dapat memburuk seiring waktu. Pada penyakit ini, saluran-saluran empedu di dalam hati mengalami peradangan sehingga pada akhirnya mengalami kerusakan. Tanpa saluran empedu, getah empedu akan menumpuk dan menyebabkan kerusakan hati. Penyakit ini paling banyak diderita oleh wanita berusia 40 hingga 60 tahun.
Penyebab
Getah empedu merupakan cairan yang dihasilkan oleh hati dan berfungsi untuk mencerna lemak, membantu penyerapan beberapa vitamin, dan membuang sisa-sisa racun dari dalam tubuh. Getah empedu mengalir keluar hati melalui saluran-saluran empedu.
Pada sirosis bilier primer, sel-sel kekebalan tubuh salah mengenal saluran ini sebagai sesuatu yang asing, sehingga sel-sel tersebut menyerang saluran empedu. Peradangan pada saluran empedu ini dimulai ketika salah satu jenis sel darah putih yang bernama sel limfosit T berkumpul di hati. Biasanya, sel limfosit T bekerja dengan mengenali kuman dan mempertahankan diri dari kuman. Namun, pada kondisi ini, sel limfosit T menyerang saluran-saluran empedu di dalam hati. Peradangan yang terjadi akan menyebar ke sel-sel hati di sekitarnya, membuat sel-sel yang meradang tersebut mulai digantikan oleh jaringan parut.
Jika terjadi peradangan, kondisi hati dapat memburuk hingga menyebabkan sirosis. Sirosis merupakan perubahan sel-sel hati menjadi jaringan parut, sehingga hati tidak dapat berfungsi dengan baik.
Faktor Risiko
Terdapat beberapa faktor yang dapat meningkatkan risiko seseorang mengalami sirosis bilier primer, yaitu:
1. Jenis kelamin
Umumnya orang yang mengalami sirosis bilier primer adalah perempuan.
2. Usia
Sirosis bilier primer pada umumnya terjadi pada rentang usia 30-60 tahun.
3. Faktor Genetik
Anda akan lebih berisiko mengalami sirosis bilier primer apabila ada anggota keluarga yang mengalami hal tersebut.
4. Faktor Ras
Sirosis bilier primer lebih sering ditemukan pada orang-orang Eropa Utara dan jarang ditemukan pada orang-orang Afrika, walaupun kondisi ini dapat terjadi pada seluruh ras.
5. Lingkungan
Risiko sirosis bilier primer meningkat apabila terdapat infeksi (misalnya infeksi saluran kemih), merokok, dan paparan terhadap zat-zat beracun.
Gejala
Sirosis bilier primer tidak selalu menyebabkan gejala. Bahkan, kondisi ini seringkali ditemukan secara tidak sengaja saat pemeriksaan darah rutin. Gejala utama yang sering dikeluhkan oleh pasien adalah lelah (65%), gatal (55%), dan rasa tidak nyaman di perut bagian atas kanan (8-17%). Gejala lain yang dapat muncul bisa berupa nyeri tulang dan sendi serta mulut dan mata kering. Jika sudah mencapai tahap yang berat, gejala yang muncul bisa berupa:
- Pembengkakan (edema) kaki
- Perut membuncit karena berisi cairan (asites)
- Penumpukan lemak pada kulit di dekat mata, kelopak mata, atau pada lekukan telapak tangan, tumit, siku, atau lutut (xanthoma dan xanthelasma)
- Kulit dan bagian sklera mata yang berwarna putih berubah warna menjadi kuning
- Terdapat bercak kulit yang warnanya semakin gelap bukan diakibatkan oleh paparan sinar matahari (hiperpigmentasi)
- Diare disertai BAB berlemak
- Pengeroposan tulang sehingga tulang lebih rapuh dan mudah patah
- Penurunan berat badan yang signifikan
Diagnosis
Wawancara dan Pemeriksaan Fisik
Diagnosis sirosis bilier primer dapat ditegakkan berdasarkan wawancara terkait keluhan dan riwayat medis pasien, serta pemeriksaan-pemeriksaan, baik pemeriksaan fisik maupun pemeriksaan penunjang. Pemeriksaan fisik dilakukan oleh dokter untuk menemukan tanda-tanda pada tubuh yang dapat menunjukkan adanya pembesaran organ limpa dan kerusakan hati, seperti perut buncit berisi air, penurunan massa otot, pembengkakan di ujung tangan atau kaki, telapak tangan yang berwarna merah, dan tanda-tanda lainnya.
Pemeriksaan Laboratorium
Pemeriksaan penunjang yang seringkali menjadi dasar penemuan sirosis bilier primer adalah pemeriksaan laboratorium rutin, seperti pemeriksaan enzim hati, kolesterol, bilirubin (zat warna kuning), darah lengkap, dan laju endap darah. Pemeriksaan laboratorium lainnya juga dapat dilakukan, seperti alkalin fosfatase (ALP), serta antibodi antimitokondria (AMA). ALP bisa dilihat untuk mengetahui bila organ hati mengalami kerusakan, dan AMA merupakan penanda utama penyakit ini, karena ditemukan pada 90-95% pasien sirosis bilier primer.
Pemeriksaan Pencitraan
Selain itu, pemeriksaan penunjang yang dapat dilakukan adalah pencitraan. Pencitraan pada umumnya berfungsi untuk mencari adanya sumbatan pada saluran empedu. Pencitraan ini dapat berupa ultrasonografi (menggunakan gelombang suara), computed tomography scan (CT scan), atau magnetic resonance imaging (MRI). Pada tahap sirosis, dapat ditemukan hipertensi porta, suatu kondisi tekanan darah tinggi pada pembuluh darah porta, yang membawa seluruh darah dari saluran pencernaan menuju hati agar nutrisi dapat diproses lebih lanjut.
Pemeriksaan Penunjang Lain
Pemeriksaan lainnya yang dapat dilakukan adalah biopsi atau pengambilan jaringan. Pengambilan jaringan ini merupakan pemeriksaan baku emas untuk menentukan diagnosis sirosis bilier primer, karena sampel jaringan yang diambil akan diamati secara langsung di laboratorium. Selain itu, pengamatan terhadap jaringan ini dapat digunakan untuk menentukan tingkat keparahan penyakit.
Tata Laksana
Sirosis bilier primer merupakan sebuah kondisi yang dapat berlanjut hingga menyebabkan kerusakan yang lebih parah. Oleh karena itu, terapi bertujuan untuk memperlambat laju perburukan penyakit dan untuk menangani gejala. Terapi ini dilakukan menggunakan obat-obatan. Obat-obatan ini dapat berupa obat yang biasa dipakai untuk menangani batu empedu atau obat-obatan yang biasa dipakai untuk menurunkan reaksi peradangan dalam tubuh.
Untuk menangani gejala gatal, dokter dapat memberikan obat-obatan antihistamin, untuk meredakan gejala peradangan dan gejala gatal yang timbul. Pemberian obat ini perlu dilakukan secara hati-hati karena pada pasien sirosis, obat antihistamin dapat memperparah fungsi otak.
Selain pemberian obat-obatan, aktivitas fisik tetap dianjurkan pada pasien sirosis bilier primer. Aktivitas fisik ini bertujuan untuk mencegah pengeroposan tulang yang terjadi, terutama pada wanita yang sudah berhenti haid karena terjadi penurunan hormon estrogen.
Pada kasus yang berat, dokter dapat mempertimbangkan cangkok hati. Cangkok hati juga dapat dilakukan pada kondisi-kondisi yang mengancam nyawa.
Komplikasi
Komplikasi sirosis bilier primer adalah sebagai berikut:
1. Pembesaran Pembuluh Darah Balik (Varises)
Pembuluh darah porta yang terdapat di dalam hati bisa tersumbat akibat pengerasan hati. Jika hal ini terjadi, darah akan mengalir kembali ke pembuluh darah sebelumnya, biasanya pada lambung dan kerongkongan. Jika jumlah darah yang menumpuk pada daerah tersebut terlalu banyak, dapat terjadi peningkatan tekanan pada pembuluh darah. Peningkatan tekanan ini dapat memecah pembuluh darah tersebut sehingga terjadi perdarahan. Perdarahan pada lambung dan kerongkongan merupakan kondisi kegawatdaruratan yang mengancam nyawa dan perlu ditangani dengan cepat.
2. Pembesaran Limpa (Splenomegali)
Limpa Anda akan membengkak dan berisi sel darah putih serta keping darah (trombosit), karena tubuh tidak dapat menyaring racun dari dalam darah tanpa bantuan hati.
3. Batu Empedu
Jika getah empedu tidak dapat mengalir, getah tersebut dapat mengendap hingga membentuk batu, yang dapat menyebabkan rasa nyeri dan infeksi.
4. Kanker hati
Sirosis meningkatkan risiko kanker hati, sehingga perlu pemantauan secara berkala.
5. Pengeroposan Tulang (Osteoporosis)
Orang dengan sirosis bilier primer berisiko tinggi mengalami osteoporosis, sehingga tulang lebih rapuh dan mudah patah.
6. Kekurangan Vitamin
Tidak adanya getah empedu akan mempersulit usus dalam menyerap vitamin, terutama vitamin yang larut lemak seperti vitamin A, D, E, dan K. Oleh karena itu, penderita penyakit ini dapat mengalami kekurangan vitamin tersebut, yang selanjutnya menyebabkan komplikasi seperti rabun senja dan gangguan pembekuan darah.
7. Kolesterol Tinggi (Hiperlipidemia)
Sekitar 80% penderita sirosis bilier primer memiliki kolesterol tinggi.
8. Gangguan Fungsi Otak (Ensefalopati Hepatikum)
Hal ini terjadi karena otak keracunan zat-zat yang seharusnya dapat disaring oleh hati. Ensefalopati hepatikum dapat menyebabkan perubahan kepribadian serta gangguan memori dan konsentrasi.
9. Peningkatan Risiko Penyakit Lainnya
Sirosis bilier primer terkait dengan penyakit lainnya, seperti penyakit kelenjar tiroid dan penyakit autoimun lainnya (penyakit yang disebabkan oleh sel-sel kekebalan tubuh yang salah menyerang sel tubuh sendiri).
Pencegahan
Pencegahan sirosis bilier primer sulit untuk dilakukan, karena penyakit ini seringkali muncul tanpa gejala dan kepastian untuk mengalaminya tidak diketahui. Oleh karena itu, pencegahan yang paling mungkin dilakukan adalah pencegahan komplikasi penyakit ini dengan memperlambat laju kerusakan hati.
Kapan Harus ke Dokter?
Jika Anda mengalami nyeri perut bagian kanan atas, perut semakin membengkak, serta kuning pada kulit dan mata, Anda dapat berkunjung ke dokter. Gejala-gejala ini dapat menunjukkan adanya masalah pada hati, salah satunya sirosis bilier primer. Penyakit-penyakit ini pada umumnya dapat berlanjut hingga menjadi parah, sehingga terapi awal diperlukan untuk memperlambat laju perburukan penyakit.
Mau tahu informasi seputar penyakit lainnya, cek di sini ya!
- dr Hanifa Rahma
Primary biliary cholangitis - Symptoms and causes. (2021). Retrieved 23 March 2022, from https://www.mayoclinic.org/diseases-conditions/primary-biliary-cholangitis/symptoms-causes/syc-20376874
Primary biliary cirrhosis. (2021). Retrieved 23 March 2022, from https://www.nhs.uk/conditions/primary-biliary-cirrhosis-pbc/
Pyrsopoulous, N. (2017). Primary Biliary Cholangitis (Primary Biliary Cirrhosis): Practice Essentials, Background, Pathophysiology. Retrieved 23 March 2022, from https://emedicine.medscape.com/article/171117-overview