Definition
IInflammatory Bowel Disease (IBD) is a general term for chronic or prolonged inflammation of the digestive tract. There are two main types of IBD:
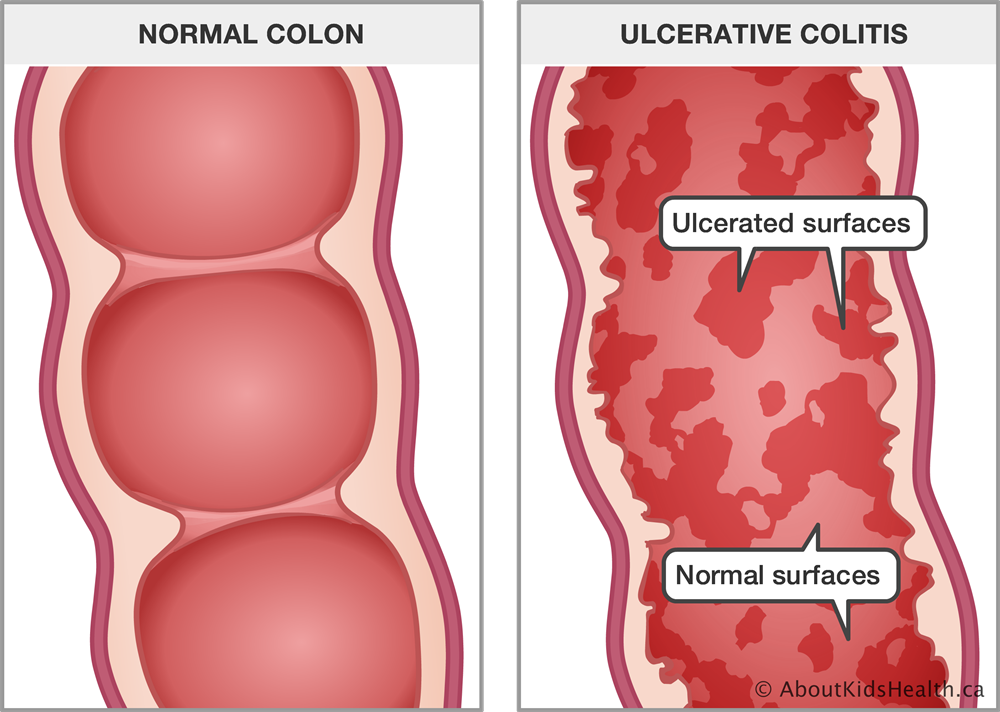
- Ulcerative Colitis: Ulcerative Colitis involves inflammation and ulceration (wounds) on the surface layer of the intestine, particularly in the rectum (which is the end of the large intestine connected to the anus).
- Crohn's Disease: This type of IBD entails inflammation of the digestive tract, specifically affecting the inner layer.
Causes
The exact cause of IBD is not known. While diet and stress were previously suspected as primary causes, they are now recognized as factors that can worsen symptoms rather than the main cause.
One possibility is an autoimmune or immune system problem. In this scenario, the immune system mistakenly attacks the cells around the digestive tract while attempting to target bacteria that are attacking the body.
There may also be a hereditary factor involved, as some individuals with IBD have family members with the condition. However, it's important to note that most people with IBD do not have a family history of the disease.
Risk factor
Risk factors for IBD include:
- Age: Most individuals diagnosed with IBD are older than 30 years, but some may not develop it until around the age of 50 or 60.
- Race: While white individuals are more at risk, IBD can affect individuals of all races.
- Family History: Having a family history of IBD increases the risk of developing the condition.
- Smoking: Smoking is a significant controllable factor for Crohn's disease.
- Improper Use of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Inappropriate use of NSAIDs can contribute to the risk of IBD.
Symptoms
The symptoms of IBD vary and depend on the severity and location of the inflammation. Symptoms can range from mild to severe, typically initiating with an active period followed by a remission or recovery period.
Common signs and symptoms of Crohn's disease and ulcerative colitis include:
- Diarrhea
- Fatigue
- Cramps or abdominal pain
- Blood in stool
- Low appetite
- Unexplained weight loss
Diagnosis
The diagnosis of IBD is typically established by excluding other potential causes. To aid in this diagnosis, the doctor may recommend several examinations, including:
Laboratory test
Laboratory tests are conducted to check for anemia or a deficiency in red blood cells, which supply oxygen and nutrients to the body. These tests also help identify potential infections. Additionally, a fecal examination is performed to detect the presence of blood or bacteria in the feces.
Endoscopy
Endoscopy is a procedure used to directly observe the condition of organs with cavities in the body, employing a small and flexible tube equipped with a lamp and camera at its end. The captured images are displayed on a monitor. Various types of endoscopy can be performed on patients with IBD:
- Colonoscopy: This procedure allows the doctor to visualize the entire large intestine. A small tissue sample (biopsy) may be taken for analysis in the lab. Biopsy helps differentiate IBD from other inflammations.
- Sigmoidoscopy: Used to observe the rectum and sigmoid, the lower part of the large intestine connected to the anus.
- Upper Digestive Tract Endoscopy: This procedure involves examining the esophagus, stomach, and duodenum.
- Capsule Endoscopy: Helpful in diagnosing Crohn's disease in the small intestine. Patients swallow a capsule with a small camera, and the images are transmitted to a recorder. The capsule is expelled with feces without causing pain. However, additional endoscopy with biopsy may still be required to confirm the diagnosis. Capsule endoscopy cannot be performed in cases of intestinal obstruction.
- Enteroscopy with Balloon: This procedure employs a balloon to explore deeper regions of the small intestine that are unreachable by normal endoscopy.
Imaging
X-ray imaging is employed in patients with severe symptoms to rule out serious complications such as a perforated large intestine. CT scan, a technique of X-ray imaging, provides more detailed images. This test allows for the comprehensive visualization of the entire intestine and surrounding tissues. MRI is useful for evaluating fistulas around the anus using hip MRI or around the small intestine with MR enterography.
Management
The goal of treating IBD is to reduce inflammation, alleviate symptoms, facilitate long-term recovery, and minimize the risk of complications. Treatment options include medication or surgery.
Anti-Inflammatory drugs
Anti-inflammatory drugs are often the first choice of therapy for IBD. The type of medication is determined by the affected area of the large intestine.
Immunosuppressants
These medications are used to modulate the immune response that releases substances inducing inflammation in the body, as they can damage the layers of the digestive tract.
Antibiotics
Prescribed antibiotics such as ciprofloxacin and metronidazole are used if there is a bacterial infection.
Other medications and supplements
Additional medications aim to control inflammation and alleviate symptoms. It's crucial to consult with a doctor before using over-the-counter drugs. The doctor may recommend:
- Anti-Diarrhea Drugs: Fiber supplements like psyllium powder or methylcellulose can help with mild to moderate diarrhea. In cases of more severe diarrhea, loperamide may be prescribed.
- Analgesic Drugs: For mild pain, doctors may recommend acetaminophen. Ibuprofen, sodium naproxen, and sodium diclofenac can worsen symptoms.
- Vitamins and Supplements: Given that IBD can affect nutrient absorption, vitamin and supplement intake may be recommended to ensure proper nutrition.
Nutritional treatment
In cases of significant weight loss, doctors may recommend a dietary approach using a feeding tube or intravenous injections. This aims to increase nutritional intake and allow the intestine to rest, potentially reducing inflammation in the short term.
Surgery
If changes in diet, medication, or other treatments fail to alleviate IBD symptoms, surgery may be recommended.
- Ulcerative Colitis: Surgery for ulcerative colitis involves the removal of the entire large intestine and the creation of a permanent opening in the abdomen to serve as an outlet for stool. The stool is expelled and collected in a bag attached to the abdomen or opening.
- Crohn's Disease: Surgery for Crohn's disease is not a complete cure and is often temporary. The disease can easily recur, typically around the connective tissue near the operated area. Medication following surgery is employed to reduce the risk of recurrence.
Diet
Certain foods and drinks can exacerbate symptoms, especially during recurrences. If you identify such foods, it's advisable to avoid them. Here are some dietary recommendations:
- Limit Dairy Products: Some individuals with IBD find that restricting dairy intake helps alleviate symptoms such as diarrhea, abdominal pain, and stomach gas. This may be due to lactose intolerance, where the body cannot process lactose found in dairy products.
- Consume Small Portions: Opt for smaller, more frequent meals (5-6 small portions per day) rather than larger meals (2-3 big portions).
- Stay Hydrated: Ensure an adequate intake of liquids, with mineral water being the preferred choice. Alcohol and caffeine can exacerbate intestinal issues, leading to increased diarrhea. Carbonated drinks may also contribute to frequent gas production.
- Consider Multivitamins: Due to the limited diet caused by Crohn's disease and the impact of inflammation on nutritional absorption, there may be a need for multivitamin supplements. Consult with a doctor before incorporating vitamins or supplements into your routine.
- Consult a Nutritionist: If there is weight loss or if the diet becomes significantly limited, consider consulting with a nutritionist for personalized guidance.
Stop Smoking
Smoking increases the likelihood of developing Crohn's disease and exacerbates its effects if you already have it. Individuals who smoke face a higher risk of recurrence, as well as an increased likelihood of needing medication and undergoing recurring surgeries.
Complications
Complications of Crohn's disease and ulcerative colitis can be similar or specific to each of them. Complications that may be found in both include:
- Bowel Cancer: Screening for cancer is typically recommended 8-10 years after the diagnosis of inflammatory bowel disease (IBD).
- Inflammation of Skin, Eyes, and Joints: Specific disorders like arthritis, skin lesions, and uveitis may occur after the recurrence of IBD.
- Drug Side Effects: Some drugs used for IBD carry a small risk of specific cancers. Corticosteroids are associated with conditions such as osteoporosis and high blood pressure.
- Primary Sclerosing Cholangitis: In this condition, inflammation causes scar tissue on the bile duct, narrowing it and gradually causing liver damage.
- Blood Clotting: IBD increases the risk of blood clotting in veins and arteries.
Crohn's Disease Complications:
- Intestinal Obstruction: Prolonged inflammation can thicken and narrow the intestine, affecting absorption.
- Malnutrition: Diarrhea, abdominal pain, and cramps can make eating difficult, hindering adequate nutrition absorption. There's a higher risk of anemia due to a lack of iron and B12 vitamins.
- Fistula: Inflammation can sometimes lead to fistulas, abnormal connections between body parts that shouldn't be connected. In some cases, fistulas can become infected, causing abscesses.
- Anal Fissure: Small tears in the anus or surrounding skin, which can easily become infected.
Ulcerative Colitis Complications:
- Toxic Megacolon: Rapid widening and swelling of the large intestine.
- Perforated Large Intestine: More often caused by toxic megacolon but can also occur independently.
- Severe Dehydration: Caused by excessive diarrhea.
Prevention
While inflammatory bowel disease (IBD) caused by hereditary factors cannot be prevented, you can reduce the risk of IBD or prevent recurrence by adopting the following measures:
- Eat a Nutritious Diet
- Regular Exercise
- Quit Smoking:
- Prompt Medical Attention: Seek prompt medical attention if you experience symptoms of IBD. Early intervention can help manage severity and reduce the likelihood of recurrence.
When to see a doctor?
Consult with a doctor if you experience prolonged issues with passing stool or exhibit any signs and symptoms of inflammatory bowel disease (IBD). While IBD typically is not considered an emergency in the short term, over a longer period, it can become serious and lead to complications that may be life-threatening.
Looking for more information about other diseases? Click here!
- dr Ayu Munawaroh, MKK
Inflammatory bowel disease. (2020). Retrieved 17 January 2022, from https://www.mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/symptoms-causes/syc-20353315
Healthline Editorial Team. (2021). Understanding the Symptoms of Inflammatory Bowel Disease (IBD). Retrieved 17 January 2022, from https://www.healthline.com/health/inflammatory-bowel-disease#diagnosis
Rowe WA. (2020). Inflammatory bowel disease. Retrieved 24 January 2022, from https://emedicine.medscape.com/article/179037-overview
Inflammatory bowel disease. (2018). Retrieved 24 January 2022, from https://www.cdc.gov/ibd/what-is-IBD.htm#:~:text=Inflammatory%20bowel%20disease%20(IBD)%20is,damage%20to%20the%20GI%20tract.
DerSarkissian C. (2021). Inflammatory bowel disease: symptoms and treatment. Retrieved 24 January 2022, from https://www.webmd.com/ibd-crohns-disease/inflammatory-bowel-syndrome
Inflammatory bowel disease (overview). (2021). Retrieved 24 January 2022, from https://my.clevelandclinic.org/health/diseases/15587-inflammatory-bowel-disease-overview
Inflammatory bowel disease. (2020). Retrieved 24 January 2022, from https://www.nhs.uk/conditions/inflammatory-bowel-disease/