Definition
Colitis is the inflammation of the layer of the colon, disrupting the digestive system in the colon. It can be caused by infection, certain diseases affecting intestinal function, or allergic reactions. The colon, shaped like a tube and formed by smooth muscle, plays a crucial role in processing food from the small intestine, absorbing water, and filtering the food to form feces. Inflammation in the colon can lead to perforation wounds, accompanied by various symptoms. Colitis is a prevalent digestive system disease, affecting all age groups, but it is more common in adults than in children.
Causes
Colitis can be caused by various conditions, including:
- Infection: Bacterial contamination of food is a common cause, with bacteria such as Campylobacter, Shigella, E. coli, Yersinia, and Salmonella being frequent culprits. Cytomegalovirus can also lead to inflammation, particularly in individuals with weakened immune systems. The parasite Giardia, often found in contaminated water, is another source of inflammation.
- Ischemic Colitis: This condition arises when there is insufficient blood supply to body tissues, leading to cell damage. The lack of proper blood flow to the intestine can result in inflammation and wounds.
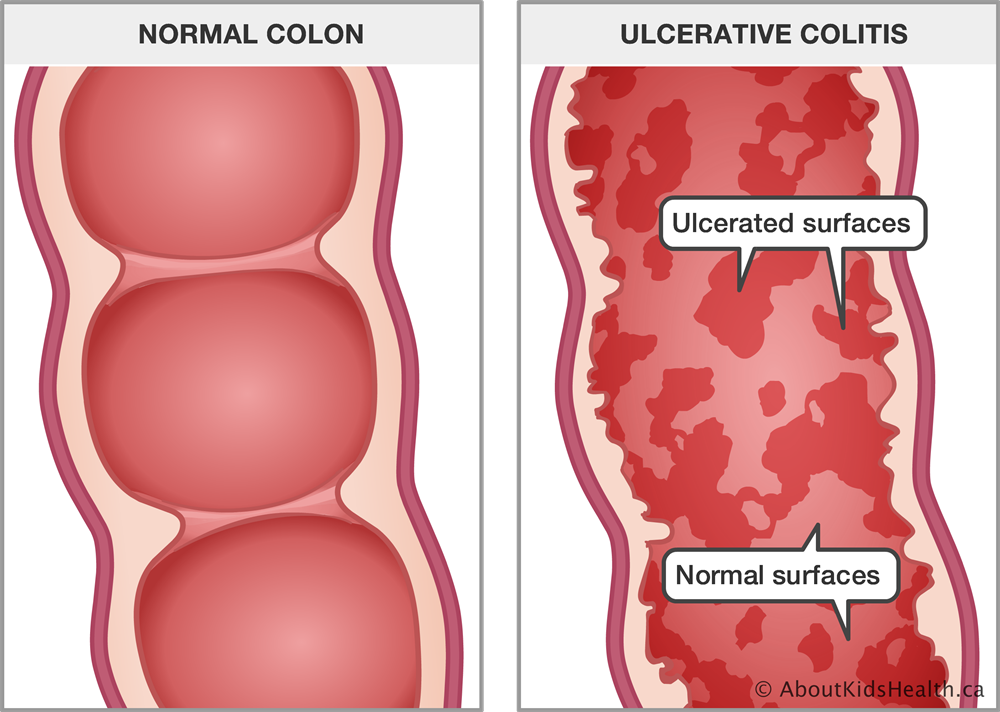
- Inflammatory Bowel Disease (IBD): IBD is an autoimmune disease linked to colitis. In this disease, the immune system mistakenly attacks healthy parts of the intestine, causing inflammation.
- Allergic Reaction: Consuming allergenic foods can induce inflammation in the colon. This is often observed in babies under 1 year old, particularly in response to cow milk or soy milk.
Microscopic Colitis is a rare condition that typically affects elderly women and is suspected to have a genetic component. While the exact cause remains unknown, it results in prolonged diarrhea.
Risk factor
Several factors can increase an individual's risk of colitis, including:
- Genetic Factors: There is an increased risk if someone in the family has a similar disease. This may be due to genetic mutations affecting the immune system in the colon.
- Colon Microbiome: The balance of bacteria, fungi, and viruses in the colon's microbiome usually does not disturb the digestive system. However, changes in the microbiome can trigger an immune response, leading to abnormal inflammation. In some cases, improper antibiotic use can contribute to these changes.
- Environmental Factors: Habits and environmental exposures can pose a risk. Factors such as infrequent consumption of healthy food, smoking, frequent exposure to pollution, and lack of hygiene may contribute to the development of colitis.
Symptoms
The symptoms of colitis include:
- Abdominal Pain: Inflammation leads to increased contractions of smooth muscles, causing intermittent pain or cramps.
- Lower Abdominal Pain: Pain is often felt in the lower part of the abdomen.
- Diarrhea: Disturbance in colon mobility can result in diarrhea. This condition is usually accompanied by pain, whether it occurs before, during, or after bowel movements.
- Fever
- Shivering
- Fatigue: Persistent inflammation and the body's immune response can lead to fatigue.
- Dehydration: Diarrhea and fever can contribute to dehydration.
- Other System Disorders: In some cases, colitis may be associated with joint swelling or inflammation in the eyes, mouth, or skin.
Diagnosis
Diagnosis is established through a medical interview about the symptoms and personal or family medical history. Physical examination is also conducted to assess the patient's condition. In diagnosing the patient, various diagnostic tests are employed, including:
- Fecal Examination: This test checks for an excess number of white blood cells in the feces, a sign of colitis. It can also identify other potential causes besides colitis.
- Colonoscopy: This procedure allows for the visualization of the inner part of the colon.
- Laboratory Tests: Blood tests may be conducted to check for anemia.
- Imaging: X-rays, CT scans, and MRIs may be employed to provide additional insights into the condition.
Management
The therapy aims to reduce and prevent symptom recurrence. It utilizes anti-inflammatory drugs (such as sulfasalazine and corticosteroids), analgesics like paracetamol, TNF inhibitors (such as infliximab), and anti-diarrheal medications like loperamide, along with iron supplements. Surgery is considered a last resort and is only used when other treatments cannot relieve symptoms. The surgical procedure involves the removal of a portion or the entire colon permanently. The doctor then creates a stoma, a permanent hole in the abdomen, to expel feces into a small pouch outside the body. This procedure is known as a colostomy.
Complications
Complications that may arise from colitis include:
- Perforated Colon: Prolonged inflammation can weaken the intestinal wall, leading to the formation of a hole. This perforation allows bacteria to grow, causing infection.
- Fulminant Colitis affects the thickness of the intestinal wall and may lead to temporary colon contraction, causing a loss of muscle mass. The gas produced may become trapped in the paralyzed part of the colon.
- Toxic Megacolon: Characterized by colon enlargement, toxic megacolon results in a loss of the colon's ability to contract properly. If not promptly treated, the colon is at risk of bursting.
- Mutations and Cancer: Prolonged inflammation left untreated can lead to the mutation and abnormal growth of surrounding cells, potentially resulting in cancerous tissue and the development of colon cancer.
Prevention
While there is no specific prevention for colitis, several measures can be taken to manage risk factors:
- RRegular Medical Check-ups: Especially if there is a family history of colitis, routine check-ups can help in early detection and management.
- Prudent Use of Medications: Avoid using drugs without proper medical instruction. If prescribed antibiotics, follow the recommended dosage.
- Healthy Diet: Consume foods rich in antioxidants, such as vegetables and fruits.
- Avoid Smoking
- Personal Hygiene
- Eat Frequent Small Meals: Opt for smaller, more frequent meals rather than large, infrequent ones.
- Stress Management: Utilize relaxation and breathing techniques to manage stress, as stress can exacerbate colitis symptoms.
When to see a doctor?
Suppose you are experiencing prolonged diarrhea lasting 2-3 weeks or displaying symptoms related to colitis or abdominal issues such as intermittent abdominal pain, fever, shivering, bloody stool, fatigue, and dehydration. In that case, it is strongly recommended to seek medical treatment promptly.
- dr Nadia Opmalina
National Health Service (2019). Health A to Z. Ulcerative Colitis.
Mayo Clinic (2021). Diseases & Conditions. Ulcerative Colitis.
Warner, J. EverydayHealth (2017). What to Know about Colorectal Cancer Screening if You Have Ulcerative Colitis.