Definition
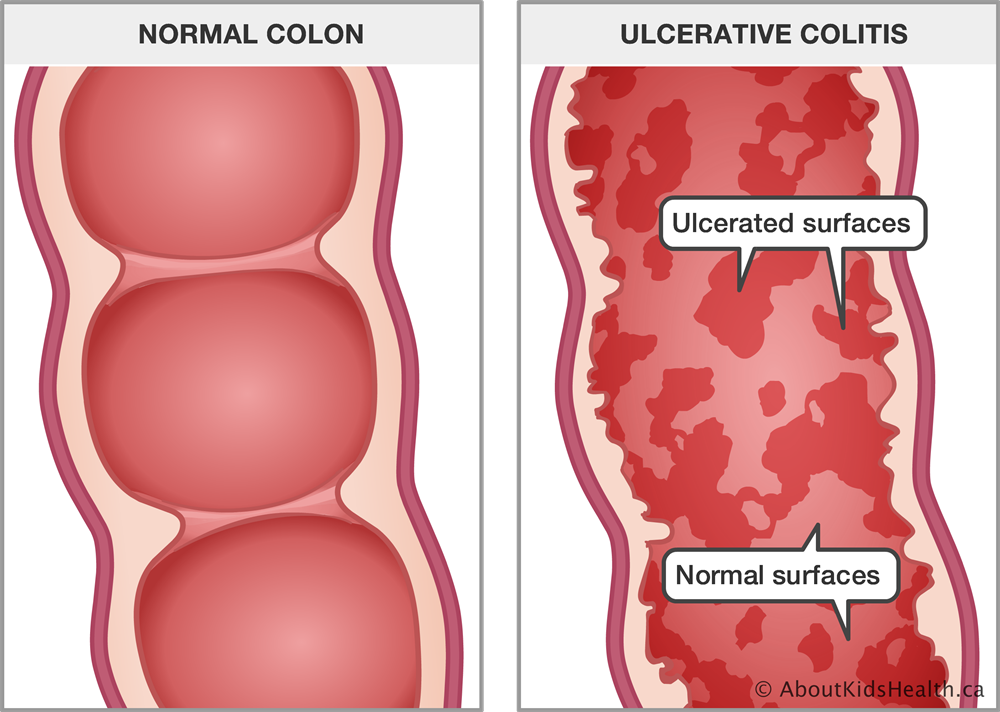
Ulcerative colitis is one of the inflammatory bowel diseases (IBD) characterized by inflammation in the colon and rectum, leading to the formation of small ulcers on the colon's surface. The inflammation typically initiates in the rectum and can extend to other parts of the colon, affecting the entire organ. This condition results in increased and more frequent colon emptying due to heightened motility.
Ulcers are formed from the cells of the colon's surface layer that have died. They can lead to bleeding and the production of pus and mucus. The prevalence of ulcerative colitis is estimated to be 9-20 cases per 100,000 people, with a higher incidence among adults. While the condition can affect individuals of all ages, it is most commonly diagnosed in individuals between the ages of 15 and 30. However, there is also a notable number of cases in individuals older than 50, with a slightly higher occurrence in males.
Causes
Ulcerative colitis is believed to result from an excessive response of the immune system, where the immune system mistakenly attacks the colon. However, the specific reason behind this excessive immune response targeting the colon, as opposed to other parts of the body, is not yet clear. Several factors are thought to contribute to the development of ulcerative colitis, including:
- Genetic factor: Inherited genes from parents can play a role in increasing the risk of ulcerative colitis.
- Autoimmune disorder: Some autoimmune disorders, where the immune system mistakenly attacks the body's own tissues, may increase the risk of ulcerative colitis.
- Environmental factors: Exposure to certain environmental factors, such as specific bacteria, viruses, or other antigens, may trigger an immune system response and contribute to the development of ulcerative colitis.
Risk factor
Several risk factors that increase the likelihood of developing ulcerative colitis include:
- Family History: Having a family history of ulcerative colitis increases the risk, suggesting a genetic predisposition to the condition.
- Ethnicity: White individuals are at a higher risk of developing ulcerative colitis compared to other ethnic groups.
- Isotretinoin Medication: The use of isotretinoin, a medication often prescribed for severe acne treatment, has been associated with an increased risk of ulcerative colitis.
Symptoms
The symptoms of ulcerative colitis can vary widely among individuals and may change over time. Individuals with ulcerative colitis may experience periods of mild symptoms or even be symptom-free (remission). However, symptoms may flare up and become more severe at times.
Common symptoms of ulcerative colitis include:
- Abdominal Pain
- Bloody Stool
- Diarrhea
- Fever
- Pain in the Rectal Area
- Body Weight Loss
- Malnutrition
Additional symptoms that may occur include:
- Joint Pain
- Joint Swelling
- Nausea
- Loss of Appetite
- Skin Problems
- Mouth Ulcers
- Inflammation of the Eyes
Diagnosis
During the physical examination, the doctor evaluates the patient based on reported symptoms to identify objective clinical signs.
For ulcerative colitis, the doctor may specifically look for signs such as abdominal pain and blood in the stool. A rectal examination is commonly performed to assess the condition of the rectum and lower part of the colon.
Physical examination
During the physical examination, the doctor evaluates the patient's symptoms to identify objective clinical signs.
In the case of ulcerative colitis, the doctor may look for signs such as abdominal pain and the presence of blood in the stool through a rectal examination.
Diagnostic test
Diagnostic tests play a crucial role in confirming the diagnosis of ulcerative colitis. These tests provide objective information about various aspects of the disease. Here are some diagnostic tests commonly used:
- Blood Test:
- Evaluate for signs of anemia.
- Measure inflammatory markers such as C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR).
- Fecal Examination:
- Assess for signs of inflammation.
- Detects the presence of blood, parasites, or bacteria.
- CT Scan: Visualize the abdominal and pelvic areas to identify inflammation, abscesses, or other abnormalities.
- Endoscopy:
- Examine the upper gastrointestinal tract, including the stomach, esophagus, and small intestine.
- Helps evaluate the extent of inflammation and identify any lesions.
- Colonoscopy:
- Direct visualization of the colon and rectum.
- Allows for the assessment of inflammation, ulceration, and the overall condition of the colon.
Management
Ulcerative colitis is a chronic disease. Therapy aims to reduce inflammation, which is the underlying cause of symptoms, and achieve longer periods of remission. The choice of medication depends on the severity of the condition.
For mild symptoms, medications to reduce inflammation and swelling may be prescribed. These medications include sulfasalazine, mesalamine, balsalazide, or olsalazine. Corticosteroids may be necessary in some cases, but their use is limited due to potential side effects. Antibiotics can be considered if there is an infection.
In cases of moderate to severe symptoms, immunosuppressant medications may be recommended. These medications, often in the form of antibodies, aim to stop inflammation and help prevent the recurrence of symptoms. Examples of such medications include adalimumab, ustekinumab, infliximab, or tofacitinib.
Complications
Colitis ulcerative can lead to various complications, with one of the most significant risks being the development of colon cancer. The longer the duration of the disease, the higher the risk of colon cancer. Regular colonoscopies are often recommended for individuals with ulcerative colitis who are at high risk of colon cancer. Screening every 1-3 years helps in early detection and intervention. Other complications may include:
- Thickening of the intestinal wall
- Intestinal bleeding
- Sepsis or systemic infection
- Severe dehydration
- Colon rupture
- Inflammation in the skin, eyes, and joints
- Toxic megacolon or rapid swelling of the colon
- Liver disease
Prevention
While there is no definitive evidence for preventing ulcerative colitis, adopting a healthy lifestyle can contribute to overall well-being. It may potentially reduce the risk of certain diseases, including inflammatory bowel diseases. Some lifestyle factors that may help reduce the risk include:
- Balanced Nutrition
- Avoiding Smoking and Secondhand Smoke
- Moderate Alcohol Consumption
- Regular Exercise
- Adequate Rest
- Stress Management
- Adequate Sleep
When to see a doctor?
If you notice worsening symptoms, such as heightened abdominal pain or gastrointestinal bleeding with bloody stools, it is advisable to seek prompt evaluation from an internal medicine doctor or a specialist in gastroenterology.
Consulting a pediatrician is essential for ulcerative colitis in children under 18 years old. The doctor will conduct a thorough medical interview and physical examination and may recommend specific diagnostic tests to accurately diagnose the underlying disease. The subsequent management plan will be tailored to the individual needs of the child.
Lynch WD, Hsu R. Ulcerative Colitis. [Updated 2021 Jun 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459282/
Healthline. Ulcerative collitis. September 2021. https://www.healthline.com/health/ulcerative-colitis#prevention
Medline Plus. Ulcerative collitis. January 2021. https://medlineplus.gov/ency/article/000250.htm