Definition
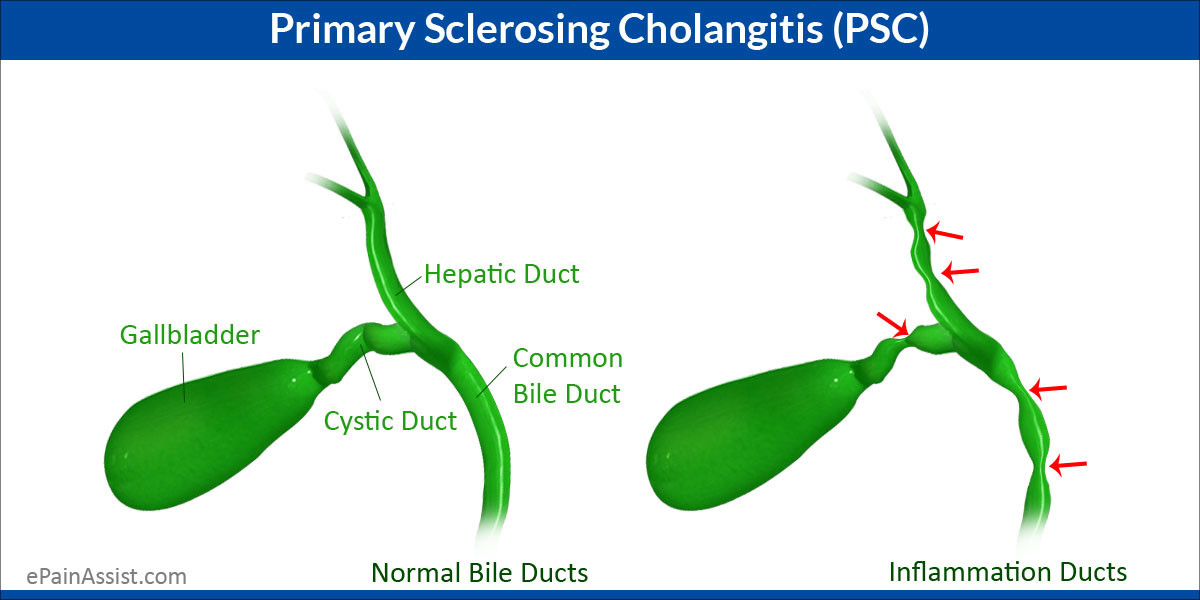
Primary Sclerosing Cholangitis (PSC) is a rare condition primarily affecting the bile ducts. These ducts play a crucial role in transporting bile, a digestive fluid produced by the liver, from the liver to the gallbladder and subsequently to the small intestine, which aids in fat digestion.
PSC is characterized by inflammation in the bile ducts, which causes the formation of scar tissue (sclerosis) and leads to the narrowing of these ducts. Consequently, bile has difficulty reaching the gallbladder and small intestine, resulting in the accumulation of bile within the liver.
Primary Sclerosing Cholangitis (PSC) is typically diagnosed in individuals in their 40s, and it is more prevalent in men than in women. In many cases, there are no specific symptoms or signs at the time of diagnosis, but disruptions in liver function are evident through blood tests.
Early symptoms and signs of PSC may include:
- Fatigue
- Abdominal discomfort
- Severe itching (pruritus)
If the condition worsens, additional symptoms such as jaundice (yellowish discoloration of the skin and eyes) and splenomegaly (spleen enlargement) may occur. The accumulation of bile in the liver can lead to chronic liver diseases like cirrhosis and liver failure.
In PSC, fat digestion is impaired, leading to weight loss and a deficiency in fat-soluble vitamins. One crucial fat-soluble vitamin affected is vitamin D, which plays a role in calcium absorption for bone health. Vitamin D deficiency can result in conditions like osteoporosis in PSC patients.
PSC is associated with other medical conditions, such as inflammatory bowel disease (IBD), specifically ulcerative colitis, where inflammation in the small intestine can cause ulcers and abdominal pain. The reason for this connection is not yet fully understood, but around 70% of PSC patients also have IBD.
Patients with PSC are more prone to autoimmune diseases like type 1 diabetes, celiac disease, or thyroid disorders. Autoimmune diseases involve the immune system attacking the body's tissues and organs. Additionally, individuals with PSC have an increased risk of developing cancer, especially bile duct cancer or cholangiocarcinoma.
It is estimated that 1 in 10,000 people has PSC, with the diagnosis established in approximately 1 in 100,000 people per year worldwide.
Causes
The exact cause of PSC is still not known. There is speculation that genetic and environmental factors sometimes play a role. Genetic factors are considered because PSC tends to occur more frequently in individuals with a family history of the disease. Some researchers also suspect a connection between autoimmune diseases and PSC.
Risk factor
Doctors and medical professionals will assess whether you have risk factors that may increase the likelihood of developing PSC. Some of these risk factors include a family history of PSC and current autoimmune diseases. A history of previous PSC, whether in oneself or the family, can also elevate the risk of developing PSC.
Symptoms
Symptoms that may appear in PSC include:
- Fever
- Shivering
- Upper abdominal pain
- Itching
- Easy fatigue
- Loss of appetite
- Weight loss
- Jaundice or yellowing of the skin and eyes
In severe cases, fat-soluble vitamins such as A, D, E, and K may be deficient due to disruptions in fat absorption. Additionally, bone problems can occur, leading to bone calcification and an increased risk of fractures.
Diagnosis
Individuals can alleviate symptoms at home by applying cold compresses to itchy skin areas and opting for loose, soft clothing. If the symptoms worsen, seeking prompt medical attention is crucial for accurate diagnosis and proper care. If PSC is confirmed, healthcare providers may prescribe Ursodeoxycholic Acid (UDCA). Surgery can sometimes be performed to widen the narrowed bile duct.
Management
Individuals can alleviate symptoms at home by applying cold compresses to itchy skin areas and opting for loose, soft clothing. If the symptoms worsen, seeking prompt medical attention is crucial for accurate diagnosis and proper care. If PSC is confirmed, healthcare providers may prescribe Ursodeoxycholic Acid (UDCA). Surgery can sometimes be performed to widen the narrowed bile duct.
Complications
Complications of PSC can include:
- Deficiency of fat-soluble vitamins A, D, E, and K
- Osteoporosis
- Cholangiocarcinoma (bile duct cancer)
- Gallbladder cancer
- Gallstones (cholelithiasis)
- Portal hypertension
- Hepatocellular carcinoma with liver cirrhosis
- Colon cancer in ulcerative colitis
Prevention
Currently, no specific and guaranteed preventive measures to avoid primary sclerosing cholangitis (PSC). However, certain lifestyle practices may contribute to reducing the risk of developing PSC:
- Consuming a balanced nutritious diet
- Avoiding smoking
- Avoiding alcohol consumption
- Exercising regularly
- Ensuring adequate rest
When to see a doctor?
If your current symptoms worsen, it is advisable to consult with an internal medicine doctor. The doctor will conduct a medical interview and physical examination and may recommend additional diagnostic tests to determine the underlying condition or disease and prescribe the appropriate and necessary treatment.
Looking for more information about other diseases? Clickk here!
- dr Anita Larasati Priyono
Rawla P, Samant H. Primary Sclerosing Cholangitis. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537181/
Medline Plus. Primary sclerosing cholangitis. May 2012. https://medlineplus.gov/genetics/condition/primary-sclerosing-cholangitis/#:~:text=Primary%20sclerosing%20cholangitis%20is%20a,where%20it%20aids%20in%20digestion.
Medscape. Primary sclerosing cholangitis. November 2019. https://emedicine.medscape.com/article/187724-overview