Definisi
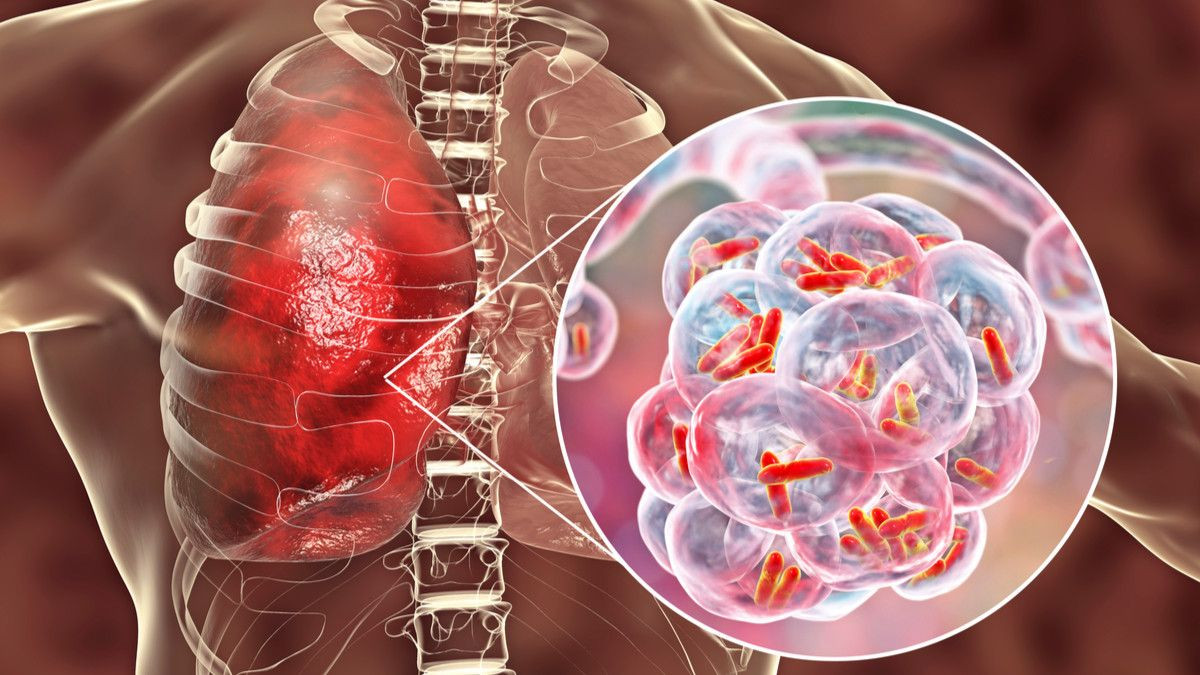
Pneumonia adalah peradangan paru yang paling sering disebabkan oleh infeksi kuman. Sementara, pneumonia komunitas atau community-acquired pneumonia (CAP) adalah jenis pneumonia yang ditemukan di luar rumah sakit atau fasilitas kesehatan lainnya. Seseorang dikatakan mengidap pneumonia komunitas jika terinfeksi pneumonia dan tidak memiliki riwayat perawatan di rumah sakit atau fasilitas kesehatan lainnya dalam beberapa waktu terakhir. Pneumonia komunitas merupakan jenis pneumonia yang paling umum.
Penyebab
Pneumonia adalah penyakit umum yang menginfeksi jutaan orang setiap tahunnya. Kuman seperti bakteri, virus, dan jamur dapat menyebabkan pneumonia. Pada orang dewasa, bakteri adalah penyebab pneumonia yang paling sering.
Beberapa cara kuman dapat masuk ke paru-paru adalah melalui:
- Bakteri dan virus yang normalnya hidup di hidung, sinus, atau mulut dapat menyebar ke paru-paru
- Menghirup kuman dari udara dan langsung masuk ke paru-paru
- Menghirup makanan, cairan, atau muntahan ke paru-paru (pneumonia aspirasi)
Pneumonia dapat disebabkan oleh banyak jenis kuman, yaitu:
- Bakteri. Penyebab paling umum pneumonia bakteri adalah Streptococcus pneumoniae (pneumokokus). Pneumonia bakterial dapat terjadi dengan sendirinya atau timbul setelah pasien mengalami pilek atau influenza. Pneumonia bakteri dapat mengenai satu bagian (lobus) paru-paru, yang disebut dengan pneumonia lobar
- Organisme mirip bakteri. Mycoplasma pneumoniae juga dapat menyebabkan pneumonia. Pneumonia jenis ini biasanya menyebabkan gejala yang lebih ringan daripada jenis pneumonia lainnya
- Jamur. Pneumonia karena jamur paling sering terjadi pada orang dengan penyakit kronis atau jangka panjang, pasien dengan sistem kekebalan tubuh yang lemah, dan pada orang yang menghirup organisme dalam jumlah banyak. Jamur penyebab pneumonia dapat ditemukan di tanah atau kotoran burung dan bervariasi tergantung pada lokasi geografis. Contoh jamur penyebab pneumonia adalah Pneumocystis jirovecii
- Virus, termasuk SARS-CoV-2. Beberapa virus penyebab pilek dan influenza dapat menyebabkan pneumonia juga. Virus adalah penyebab pneumonia paling umum pada anak-anak di bawah 5 tahun. Pneumonia virus biasanya ringan. Namun, beberapa kasus dapat berkembang menjadi kondisi serius, seperti penumonia pada Covid-19.
Faktor Risiko
Faktor risiko pneumonia meliputi:
- Penyakit paru-paru kronis, seperti PPOK, bronkiektasis, fibrosis kistik
- Merokok
- Demensia atau penurunan kognitif pada lansia, stroke, cedera otak, cerebral palsy, atau gangguan otak lainnya
- Masalah sistem kekebalan tubuh, seperti sedang dalam pengobatan kanker, sakit HIV /AIDS, atau transplantasi organ
- Penyakit serius lainnya, seperti penyakit jantung, sirosis hati, atau diabetes
- Operasi atau trauma yang baru saja terjadi
- Operasi untuk mengobati kanker mulut, tenggorokan, atau leher
Gejala
Gejala pneumonia yang paling umum adalah:
- Batuk, dapat disertai dengan lendir kehijauan atau kuning, atau bahkan lendir berdarah
- Demam, bervariasi dari ringan hingga tinggi
- Menggigil
- Sesak nafas, biasanya timbul saat beraktivitas
Gejala lainnya termasuk:
- Kebingungan, terutama pada orang tua
- Keringat berlebih dan kulit lembab
- Sakit kepala
- Kehilangan nafsu makan, kekurangan energi, dan kelelahan
- Malaise (tidak enak badan)
- Nyeri dada tajam atau menusuk yang memberat saat menarik nafas atau saat batuk
- Sindrom kuku putih atau leukonikia
Diagnosis
Dalam mendiagnosis, dokter akan menanyakan keluhan dan riwayat kesehatan, melakukan pemeriksaan fisik, serta pemeriksaan penunjang. Pada pemeriksaan fisik, dokter akan mendengarkan apakah ada suara nafas abnormal pada paru melalui stetoskop. Pada pneumonia, umumnya terdengar bunyi nafas tambahan bernada rendah yang disebut ronki akibat adanya penyumbatan jalan napas oleh lendir. Ronkhi dapat terdengar pada saat menarik nafas maupun saat menghela nafas.
Jika dicurigai mengidap pneumonia, dokter akan merekomendasikan rontgen dada. Tes lain yang mungkin juga akan dilakukan adalah:
- Tes gas darah arteri, untuk melihat kecukupan oksigen di paru yang dapat masuk ke darah
- Kultur darah dan dahak, untuk mencari kuman yang mungkin menyebabkan pneumonia
- Hitung darah lengkap, untuk memeriksa jumlah sel darah putih. Peningkatan jumlah sel ini dan jenis sel darah putih tertentu dapat menandakan adanya infeksi bakteri
- CT scan dada
- Bronkoskopi, yaitu melihat ke dalam tenggorokan dan paru menggunakan selang fleksibel dengan kamera di ujungnya. Gambar akan ditampilkan di layar
- Torasentesis, yaitu mengeluarkan cairan dari ruang antara lapisan pembungkus paru
- Swab nasofaring untuk menilai virus seperti influenza dan SARS-CoV-2
Tata laksana
Dokter harus menentukan apakah pasien perlu rawat inap atau cukup rawat jalan. Jika diperlukan rawat inap, pasien akan menerima:
- Cairan dan antibiotik melalui infus
- Terapi oksigen
- Perawatan pernapasan sesuai keperluan
Pada pneumonia bakteri, pasien harus memulai terapi antibiotik segera setelah masuk rumah sakit. Sedangkan pada pneumonia virus, tidak akan diberikan antibiotik karena antibiotik tidak membunuh virus. Anda dapat memperoleh obat lain, seperti antivirus, jika mengalami influenza.
Kemungkinan besar pasien akan dirawat di rumah sakit jika:
- Memiliki penyakit serius lainnya
- Memiliki gejala yang parah
- Tidak dapat merawat diri sendiri di rumah
- Tidak bisa makan dan minum
- Berusia lebih dari 65 tahun
- Telah menggunakan antibiotik di rumah namun kondisi belum membaik
Kebanyakan kasus masih bisa dirawat di rumah. Jika demikian, dokter akan meminta memberikan obat-obatan termasuk antibiotik dalam bentuk tablet.
Yang harus Anda perhatikan saat minum antibiotik:
- Minum antibiotik sesuai aturan dokter
- Minum antibiotik sampai habis, bahkan ketika Anda sudah mulai merasa lebih baik
- Jangan minum obat batuk atau obat flu kecuali atas izin dokter, karena batuk dapat membantu membuang lendir dari paru-paru
Menghirup udara hangat dan lembab dapat membantu melonggarkan lendir yang mungkin membuat tenggorokan terasa tidak nyaman. Hal-hal berikut dapat membantu mengurangi keluhan Anda:
- Letakkan waslap basah yang hangat di atas hidung dan mulut
- Isi mesin pelembab udara dengan air hangat dan hirup udara hangat perlahan
- Tarik napas dalam 2 atau 3 kali setiap jam. Napas dalam akan membantu membuka paru-paru
- Ketuk dada dengan lembut beberapa kali sambil berbaring dengan kepala lebih rendah dari dada. Tindakan ini membantu mengeluarkan lendir dari paru-paru sehingga Anda bisa mengeluarkannya melalui mulut
Minum banyak cairan, selama dokter tidak membatasinya.
- Minum air putih, jus, atau teh tidak kental
- Minum air putih setidaknya 6 hingga 10 gelas (1,5 hingga 2,5 liter) sehari
- Jangan minum alkohol
Istirahat yang cukup saat sudah pulang ke rumah. Jika sulit tidur di malam hari, dapat ditambahkan dengan tidur siang.
Komplikasi
Dengan pengobatan, kebanyakan orang akan membaik dalam waktu 2 minggu. Orang dewasa yang lebih tua atau orang yang sakit berat mungkin memerlukan perawatan lebih lama. Mereka yang biasanya perlu mendapat perawatan lebih lama adalah:
- Orang tua
- Orang yang sistem kekebalannya tidak bekerja dengan baik
- Orang dengan penyakit serius lainnya, seperti diabetes atau sirosis hati
Pada semua kondisi di atas, pneumonia dapat menyebabkan kematian jika sudah parah.
Pada kasus yang jarang terjadi, dapat berkembang masalah yang lebih serius akibat pneumonia, yaitu:
- Perubahan paru yang mengancam jiwa sehingga membutuhkan alat bantu nafas
- Terbentuk cairan di antara selaput pembungkus paru (efusi pleura)
- Terbentuk nanah di antara selaput pembungkus paru (empiema)
- Abses paru, yaitu kumpulan nanah di dalam jaringan paru
Dokter akan melakukan rontgen dada lagi untuk memastikan paru-paru Anda bersih. Umumnya, diperlukan waktu beberapa minggu agar rontgen paru Anda bersih, dan biasanya Anda sudah merasa lebih baik sebelum gambaran rontgen dada bersih.
Pencegahan
Anda dapat mencegah pneumonia dengan mengikuti langkah-langkah berikut:
- Sering-seringlah mencuci tangan, terutama:
-
- Sebelum menyiapkan dan memakan makanan
- Setelah membuang ingus
- Setelah menggunakan toilet
- Setelah mengganti popok bayi
- Setelah kontak dengan orang yang sakit
- Hindari kontak dengan orang yang sakit
- Jangan merokok. Tembakau merusak kemampuan paru-paru untuk melawan infeksi
- Vaksin dapat membantu mencegah beberapa jenis pneumonia. Pastikan untuk mendapatkan vaksin berikut:
- Vaksin flu dapat mencegah pneumonia yang disebabkan oleh virus flu
- Vaksin pneumokokus menurunkan kemungkinan terkena pneumonia karena Streptococcus pneumoniae
- Vaksin Covid-19
Vaksin bahkan sangat penting untuk orang dewasa yang lebih tua dan penderita diabetes, asma, emfisema, HIV, kanker, orang dengan transplantasi organ, atau penyakit jangka panjang lainnya.
Kapan harus ke dokter?
Konsultasi dengan dokter jika Anda memiliki:
- Batuk yang mengeluarkan lendir berdarah atau berwarna seperti karat
- Gejala pernapasan yang memburuk
- Nyeri dada yang memburuk saat batuk atau bernapas
- Pernapasan cepat atau nyeri
- Keringat malam atau penurunan berat badan yang tidak dapat dijelaskan
- Sesak nafas, menggigil kedinginan, atau demam terus-menerus
- Tanda-tanda pneumonia pada kondisi sistem kekebalan tubuh yang lemah misalnya, pada penderita HIV atau pasien kemoterapi
- Memburuknya gejala setelah perbaikan awal
- dr Anita Larasati Priyono
Community-acquired pneumonia in adults. (2020). Retrieved 28 February 2022, from https://medlineplus.gov/ency/article/000145.htm
Baer SL. (2022). Community-acquired pneumonia (CAP). Retrieved 28 February 2022, from https://emedicine.medscape.com/article/234240-overview
Ramirez JA. (2021). Overview of community-acquired pneumonia in adults. Retrieved 28 February 2022, from https://www.uptodate.com/contents/overview-of-community-acquired-pneumonia-in-adults#H3873548286
Pneumonia. (2020). Retrieved 28 February 2022, from https://www.mayoclinic.org/diseases-conditions/pneumonia/symptoms-causes/syc-20354204#:~:text=Community%2Dacquired%20pneumonia&text=It%20may%20be%20caused%20by,a%20cold%20or%20the%20flu.
Regunath H, Oba Y. (2021). Community-Acquired Pneumonia. Retrieved 28 February 2022, from https://www.ncbi.nlm.nih.gov/books/NBK430749/