Definition
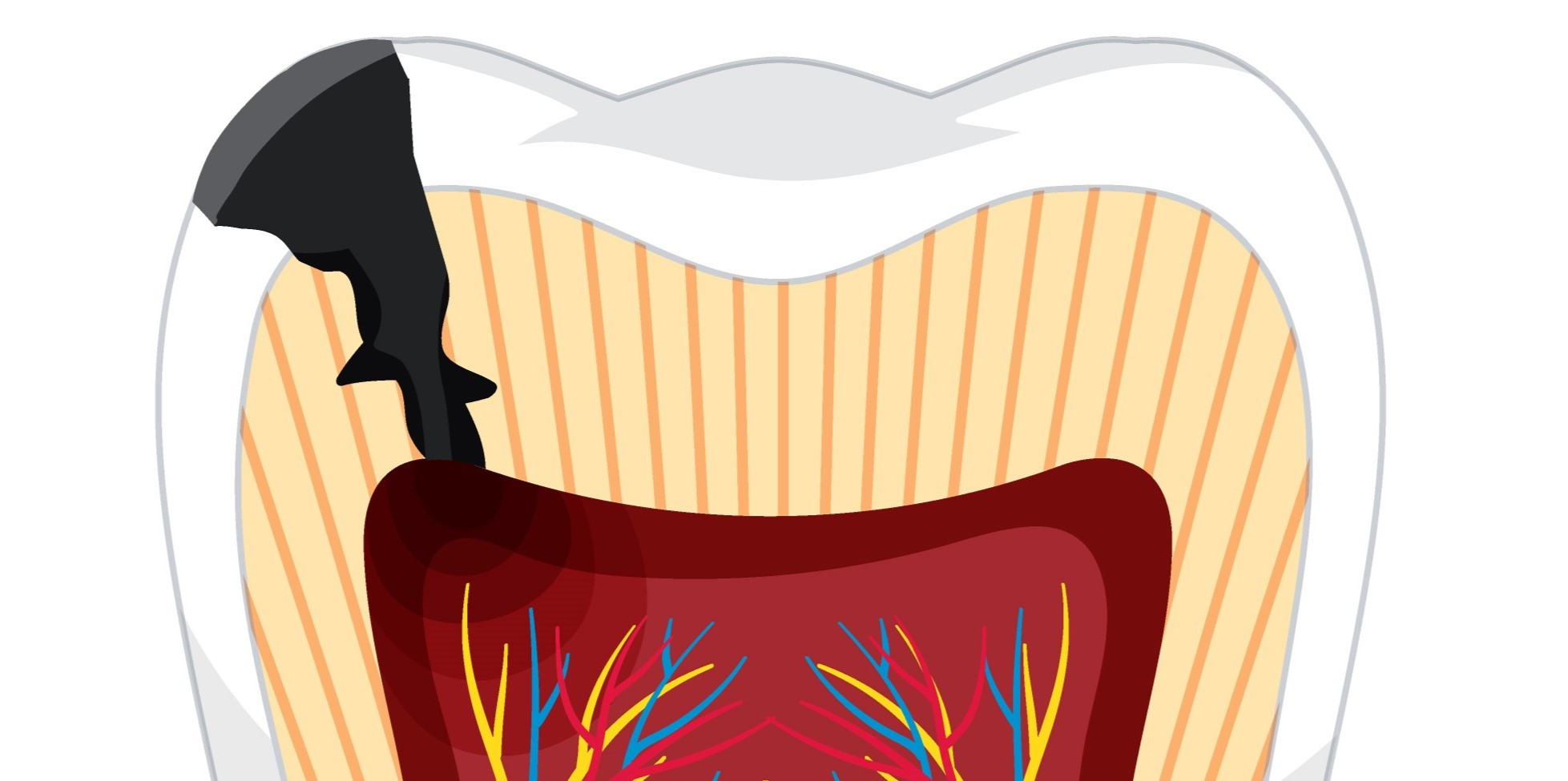
Gingivitis refers to the inflammation of the gum tissues. A bacterial infection usually causes it, and its symptoms include swollen, painful, and bleeding gums. Poor oral hygiene is a significant factor that increases the risk of developing gingivitis. If left untreated, gingivitis can lead to a more severe condition known as periodontitis, which involves inflammation of the gum tissues surrounding the teeth and bones.
Causes
The following factors contribute to the development of gingivitis:
- Accumulation of dental plaque
The buildup of plaque and tartar from food debris is the most common cause of gingivitis. Neglecting dental hygiene can lead to tooth decay and gum decay.
- Hormonal changes
Puberty, menopause, the menstrual cycle, and pregnancy may cause hormonal fluctuations. The gingiva becomes more sensitive, which increases the risk of inflammation.
- Medical history
Gingivitis is related to diseases such as cancer, diabetes, and HIV. These associated medical conditions may weaken the immune system, raising the risk of inflammation and infection.
- Medications
Decreased salivary production is a common adverse effect of medications that affect oral health.
- Smoking
Gum inflammation is more common in smokers. Free radicals, originating from the tar in cigarettes, lead to inflammation in the oral cavity. They cause potential harm to the oral tissues.
- Age
According to reports, the incidence of gingivitis increases with age.
- Poor nutrition
Gingivitis is frequently associated with vitamin C deficiency.
Risk Factor
Several factors can raise the risk of gingivitis, including:
- Not maintaining oral hygiene, such as neglecting tooth brushing and not doing routine dental examinations at the dentist
- Smoking
- Taking certain medications, such as birth control pills, steroids, anticonvulsants (seizure medications), chemotherapy, blood thinners, and calcium channel blockers, increases the risk of gingivitis
- Immunocompromised disorders such as HIV/AIDS and diabetes
- Deficiency in nutrition, specifically vitamin C, increases the susceptibility to oral and dental problems
- Dry mouth (xerostomia) may impact periodontal health. Diminished salivary secretion may cause inflammation and swelling of the gums
- Possessing undesirable behaviors, such as chewing on hard items
- Past medical histories, such as agranulocytosis, thrombocytopenia, hemophilia, anemia, and leukemia
- Hormonal changes during pregnancy, menstruation, and menopause can increase blood circulation, making them more susceptible to inflammation, swelling, and bleeding
Symptoms
Gingivitis is a common dental problem, but it is hard to recognize in the early stages since the symptoms are not always obvious. However, as the condition progresses, it can cause swollen, painful, reddish gums that bleed easily. Bad breath, tooth loss, and receding gums are other symptoms that may accompany gingivitis. It is important to seek treatment for gingivitis as soon as possible to prevent further damage to your teeth and gums.
Diagnosis
Gingivitis can be identified with a dental examination. The doctor will assess the condition of the gums to ascertain the presence of inflammation while also requesting a comprehensive medical history. The doctor will additionally measure the periodontal pockets. The ideal range for the periodontal pocket depth is 1-3 millimeters (mm).
Management
Immediate treatment is required to relieve the symptoms and prevent complications, specifically the progression of damage to the gums and teeth. Plaque removal is the initial treatment for gingivitis, followed by administering antibiotics and if required, surgical intervention.
However, if plaque removal is insufficient or hardened deposits of plaque in the mouth are present, then it is necessary to undergo professional treatments such as scaling and root planing.
Complications
Untreated gingivitis can lead to more severe problems, such as periodontitis. Infection can spread to the soft tissue around the gums and the bone supporting the teeth. As the infection progresses, it can spread and harm other organs, such as the heart and lungs. Periodontitis-causing bacteria may enter the bloodstream through the gum tissue to cause this.
Prevention
Maintaining good oral and dental hygiene can help prevent gingivitis. The following procedures may help prevent gingivitis:
- Brush your teeth regularly
Brush your teeth using the appropriate technique twice daily with twenty seconds of circular motions from the top to the bottom on each side. A toothbrush with a small-tipped head and delicate bristles can effectively clean all areas of your oral cavity. Additionally, select toothpaste that includes fluoride. This toothpaste's mineral composition effectively fortifies and safeguards teeth against injury.
- Use dental floss
Flossing is an effective method for removing food particles lodged between the teeth and below the gum line.
- Stop smoking
Cigarettes are one of the most important factors in gingivitis. As a result, you should make every effort to quit smoking. Smoking cessation not only prevents gingivitis or gum inflammation, but it also improves your general health.
- Consume healthy diet
Eating healthy foods helps your immune system fight gingivitis-causing bacteria. Vitamin C and E from fruits and vegetables are good for your teeth and mouth. These vitamins can also repair the tissue damage.
- Avoid stress
Stress may also affect your dental and oral health. If stressed, the immune system cannot fight the bacteria responsible for the infection.
- See your dentist regularly
Regular dental check-ups can help doctors monitor the health of your teeth. The doctor can also immediately begin treatment and identify any concerns. Visit your dentist every 6 to 12 months. If you are more prone to gingivitis, your doctor may recommend more frequent checks. Your doctor may recommend more frequent check-ups if you are at a higher risk of developing gingivitis.
When to see a doctor?
Regular dental check-ups every 6 months are recommended to prevent gingivitis and its complications. To avoid complications, see a dentist immediately if you have dental issues.
Want to know more information about other diseases? Click here!
- dr. Benita Kurniadi
Trombelli L. (2018, June 21). Plaque-induced gingivitis: case definition and diagnostic considerations. Retrieved January 21, 2023. Available from: https://aap.onlinelibrary.wiley.com/doi/10.1002/JPER.17-0576
Mayo Clinic. (2017). Gingivitis: diagnosis and treatment. Retrieved January 21, 2023, from https://www.mayoclinic.org/diseases-conditions/gingivitis/diagnosis-treatment/drc-20354459
American Dental Association. (2022). Gingivitis. Retrieved 21 January 21, 2023, Available from: https://www.mouthhealthy.org/all-topics-a-z/gingivitis