Definisi
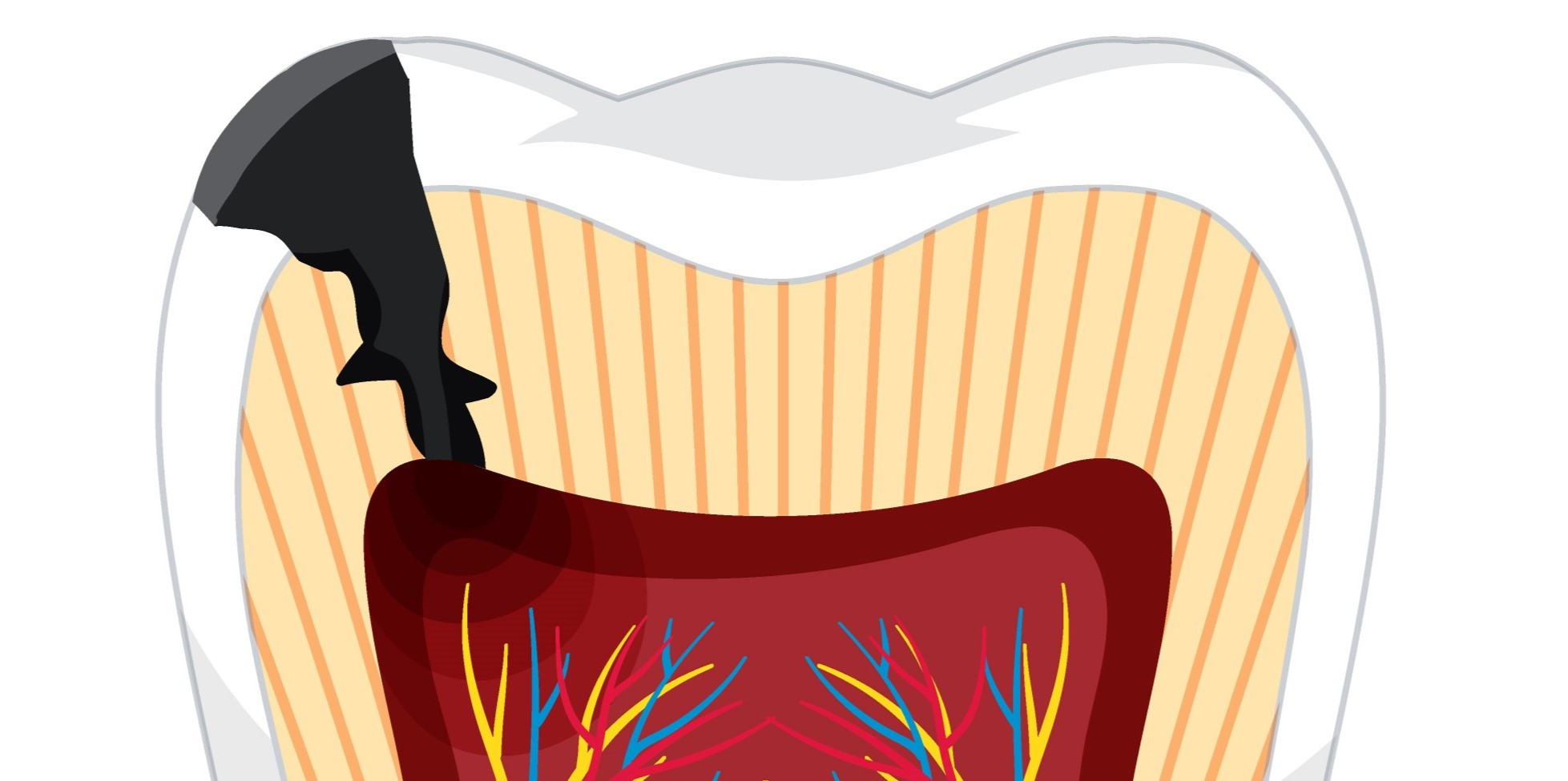
Pulpitis adalah peradangan pada pulpa yang terasa nyeri. Pulpa sendiri adalah jaringan lunak gigi yang paling dalam. Jaringan ini mengandung saraf, pembuluh darah, dan jaringan ikat. Pulpa menyuplai darah dan nutrisi ke lapisan gigi luar yang keras untuk mempertahankan kesehatan gigi.
Pulpitis disebabkan oleh bakteria yang menginvasi pulpa gigi, dan dapat terjadi pada satu gigi atau lebih yang kemudian menyebabkan pembengkakan pada bagian yang terinfeksi. Dokter gigi mengklasifikasikan pulpitis menjadi dua tipe berdasarkan tingkat keparahan infeksi:
- Pulpitis reversibel
Pada stadium awal ini, peradangan ringan dan pulpa gigi masih cukup sehat untuk diselamatkan jika dokter gigi melekukan perawatan gigi dan menutupnya dengan filling.
- Pulpitis irreversible
Pada stadium ini, peradangan lebih berat dan gigi tidak dapat sembuh. Jaringan pulpa pada akhirnya akan mati. Hal ini disebut dengan nekrosis pulpa.
Pulpitis adalah kondisi yang sangat sering terjadi. Centers for Disease Control and Prevention (CDC) Amerika Serikat memperkirakan sekitar 1 dari 4 orang dewasa berusia 20 sampai 64 tahun memiliki lubang pada gigi yang tidak ditangani, yang dapat menyebabkan pulpitis.
Penyebab
Enamel keras gigi Anda melindungi pulpa. Jika enamel mengalami kerusakan, hal ini dapat menyebabkan pulpitis. Kerusakan gigi dapat terjadi akibat:
- Lubang
Bakteria pada mulut Anda memproduksi asam yang dapat merusak enamel dan membentuk lubang pada gigi.
- Retakan
Retakan kecil dapat terjadi ketika Anda mengunyah makanan keras atau ketika Anda mengalami cedera pada gigi.
- Prosedur gigi
Terapi untuk gigi juga memiliki risiko untuk menyebabkan pulpitis. Jika satu gigi tidak ditutup dengan benar saat prosedur gigi, hal ini dapat memungkinkan filling untuk bocor dan menyebabkan pulpitis juga.
- Kerusakan enamel
Menggertakkan gigi atau menggosok gigi dengan agresif dapat menyebabkan kerusakan enamel dan membuat saraf lebih rentan terhadap peradangan.
Faktor Risiko
Semua hal yang meningkatkan risiko kerusakan gigi, seperti tinggal di area tanpa air yang mengandung fluor atau memiliki kondisi medis tertentu, seperti diabetes, dapat meningkatkan risiko pulpitis.
Anak-anak dan orang lanjut usia juga dapat memiliki risiko yang lebih tinggi, namun hal ini sebagian besar ditentukan oleh kualitas perawatan gigi dan kebiasaan kebersihan gigi.
Gaya hidup juga dapat meningkatkan risiko pulpitis, yaitu:
- Kebersihan gigi yang buruk, seperti tidak menggosok gigi setelah makan dan tidak memeriksakan gigi ke dokter gigi secara rutin
- Konsumsi diet yang tinggi gula, atau konsumsi makanan dan minuman yang merusak gigi, seperti karbohidrat olahan
- Memiliki profesi atau hobi yang meningkatkan risiko Anda untuk mengalami cedera pada mulut, seperti tinju atau hockey
- Bruksisme kronis (jangka panjang)
Gejala
Kedua tipe pulpitis memiliki gejala utama sakit gigi dan gigi sensitif. Nyeri yang Anda rasakan bervariasi bergantung pada stadium peradangan. Nyeri akibat pulpitis reversibel dapat lebih ringan dan hanya terjadi ketika makan. Nyeri pada pulpitis irreversible dapat lebih berat dan terjadi sepanjang hari dan malam.
Gejala pulpitis reversibel meliputi:
- Tidak ada nyeri ketika dokter gigi mengetuk gigi Anda
- Tidak ada sensitivitas terhadap panas
- Sensitivitas terhadap dingin atau rasa manis cepat hilang. Orang sering mendeskripsikan hal ini sebagai nyeri yang tajam
Pada pulpitis irreversible, Anda dapat mengalami:
- Nyeri ketika dokter gigi mengetuk gigi Anda
- Sensitivitas terhadap panas, dingin, atau rasa manis yang berlangsung selama lebih dari beberapa detik. Nyeri ini dapat bersifat berdenyut, tumpul, atau nyeri tajam
- Bau mulut
- Rasa tidak enak pada mulut
Jika nekrosis pulpa sudah terjadi dan jaringan saraf mengalami kematian, Anda mungkin tidak mengalami sensitivitas terhadap panas, dingin, atau manis. Namun, gigi Anda tetap dapat nyeri ketika dokter gigi mengetuknya.
Diagnosis
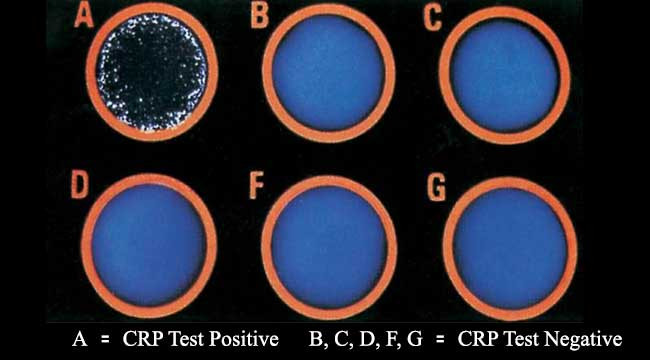
Satu dari cara utama bagi dokter gigi untuk mendiagnosis pulpitis adalah dengan menilai sensitivitas gigi Anda. Tipe tes sensitivitas meliputi:
- Tes pulpa elektrik
Tes ini menentukan apakah pulpa Anda masih hidup atau jika infeksi sudah menyebabkan nekrosis pulpa. Dokter gigi Anda akan menggunakan alat untuk menghantarkan denyut listrik kecil pada gigi. Jika pulpa Anda masih hidup, Anda akan merasakan stimulasi tersebut. Jika jaringan pulpa sudah mati, Anda tidak akan merasakan denyut listrik tersebut.
- Tes panas atau dingin
Dokter gigi akan menyentuh gigi Anda dengan zat panas atau dingin. Pada pulpitis irreversible, sensitivitas akan berlangsung lebih lama daripada beberapa detik. Jika jaringan pulpa sudah mati, Anda tidak akan merasakan sensitivitas.
- Mengetuk gigi
Hal ini dilakukan dengan mengetuk gigi Anda secara lembut. Nyeri setelah ketukan adalah tanda dari pulpitis irreversible.
Dokter gigi Anda juga akan merekomendasikan pemeriksaan X-ray gigi untuk mencari adanya cacat atau gangguan pada gigi dan tanda infeksi.
Tata Laksana
Untuk pulpitis reversibel, dokter gigi Anda akan memulai pengobatan untuk menangani penyebabnya. Terapi meliputi pengangkatan jaringan yang busuk dan menutup gigi dengan filling normal.
Pulpitis irreversible membutuhkan terapi yang lebih intensif untuk membuang jaringan pulpa. Pilihan terapi meliputi:
- Perawatan saluran akar
Anda biasanya akan dirujuk ke dokter gigi yang memiliki spesialisasi dalam konservasi gigi dan merawat infeksi pulpa untuk perawatan saluran akar. Dokter gigi akan membuang pulpa yang terinfeksi dan membersihkan akar gigi. Setelah itu, dokter akan mengisi saluran akar yang kosong dan menutup gigi. Anda akan kembali ke dokter gigi dalam beberapa minggu kemudian untuk pemasangan crown untuk menutup gigi Anda.
- Pencabutan gigi
Beberapa orang memilih untuk melakukan pencabutan gigi. Dokter gigi Anda akan mendiskusikan pilihan untuk mengganti gigi, termasuk pemasangan implan gigi atau dental bridge.
Pemberian obat antibiotik dapat dipertimbangkan untuk membantu mencegah terjadi infeksi apabila pengobatan terlambat dimulai, namun pemberian antibiotik bukan terapi utama untuk pulpitis.
Komplikasi
Jika tidak ditangani dengan baik, pulpitis dapat menyebar, menyebabkan infeksi atau abses periapikal. Abses periapikal adalah infeksi pada akar gigi, dimana terbentuk kantung berisi nanah. Hal ini dapat menyebabkan:
- Nyeri
- Demam
- Pembengkakan kelenjar getah bening pada leher
Jika infeksi tersebut juga tidak ditangani, dapat terjadi penyebaran ke tulang rahang Anda (osteomielitis) dan jaringan lunak pada kepala, leher, dan dada Anda. Jika tidak diterapi, penyebaran infeksi ini dapat mengancam nyawa.
Pencegahan
Kebersihan gigi yang baik merupakan cara terbaik untuk mencegah pulpitis. Hal ini terdiri dari:
- Menggosok gigi Anda dua kali sehari
- Flossing setiap hari
- Memeriksakan gigi pada dokter gigi untuk pembersihan dan kontrol rutin
- Menggunakan night guard jika Anda menggertakan gigi saat tidur
Selain itu, pastikan untuk langsung memeriksakan diri ke dokter gigi jika Anda mengalami nyeri gigi atau gigi Anda sensitif.
Kapan Harus ke Dokter
Anda sebaiknya berkonsultasi ke dokter gigi jika Anda mengalami nyeri gigi atau menyadari adanya sensitivitas baru terhadap makanan atau minuman panas, dingin, atau manis pada gigi Anda. Dengan terapi dini, Anda akan menghabiskan lebih sedikit waktu di dokter gigi dan lebih kecil risiko untuk mengalami kondisi yang lebih serius.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr. Lukita Tarigan
Pulpitis: Types, symptoms & treatment. Cleveland Clinic. (n.d.). Retrieved March 6, 2023, from https://my.clevelandclinic.org/health/diseases/23536-pulpitis
Whelan, C. (2019, April 17). Pulpitis: Treatment, types, symptoms, causes, and more. Healthline. Retrieved March 6, 2023, from https://www.healthline.com/health/pulpitis
WebMD. (n.d.). Pulpitis: Causes, symptoms, and treatments. WebMD. Retrieved March 6, 2023, from https://www.webmd.com/oral-health/what-is-pulpitis