Definition
Angular stomatitis or angular cheilitis is a condition in which red plaques form at the corner where the upper lip and lower lip meet. These plaques also form an angle. This condition is common in children and adults aged 30-60. Angular stomatitis can occur on one corner of the lip or both corners of the lip at once.
Causes
Infection
There are various causes of angular stomatitis, but Candida fungi and Staphylococcus bacteria are the most common. This condition generally occurs when saliva gets trapped and builds up at the corners of the lips. As the saliva dries up, the skin in the area can form crusts or cracks. This then triggers the sufferer to lick the lips to prevent the skin from drying out again. However, the corners of the lips become warm and moist, providing a suitable environment for fungal growth. This then causes the corners of the lips to become infected with fungus. If someone has a decreased body defense system due to steroid use or diseases such as HIV/AIDS, the risk of this infection will be even higher.
Skin inflammation
Apart from fungal infections, another cause of angular stomatitis is irritant or allergic contact dermatitis, which is skin inflammation caused by contact with irritating or allergy-inducing materials. Items that can cause irritation or allergies include nickel (in braces users), food (especially flavoring ingredients and preservatives), toothpaste, mouthwash, lip balm, lip cosmetic ingredients, anti-acne products, and chewing gum.
Nutrient deficiency
Another cause of angular stomatitis is nutritional deficiencies. The most common nutritional deficiencies that cause this condition are a lack of B vitamins (especially B6, folic acid/B9, and B12), minerals (zinc and iron), and a general lack of protein. These nutritional deficiencies can be caused by a variety of things, such as old age, poor nutrition, vegans, infants who do not get vitamin supplementation other than breast milk, and people with certain diseases such as gastritis (inflammation of the stomach), pancreatitis (inflammation of the pancreas, the organ that produces digestive enzymes), Crohn's disease, and anemia (lack of red blood cells).
Symptoms of other diseases
Angular stomatitis can also be a symptom of other diseases such as Sjogren's syndrome and inflammatory bowel disease (IBD) including Crohn's disease and ulcerative colitis. However, in IBD, angular stomatitis is more common in patients with Crohn's disease compared to ulcerative colitis.
Risk factor
The risk factors for angular stomatitis are highly dependent on the cause. These risk factors may include:
- Problems with the removable denture
- Presence of teeth that are misaligned in position
- Unintended drastic weight loss
- Frequent lip licking
- Smoking
- Having nutritional deficiencies, especially vitamin B
- Overuse of antibiotics
- Use of retinoid products (usually in anti-acne drugs)
- Decreased body defense system due to steroid use, cancer, HIV/AIDS, and so on
- Elderly (especially over 75 years old)
- Dry lips
- Suffering from inflammatory diseases such as Sjogren's syndrome
- Having a long-term disease such as diabetes mellitus and inflammatory bowel disease such as Crohn's disease
- Sufferers of Down syndrome
Symptoms
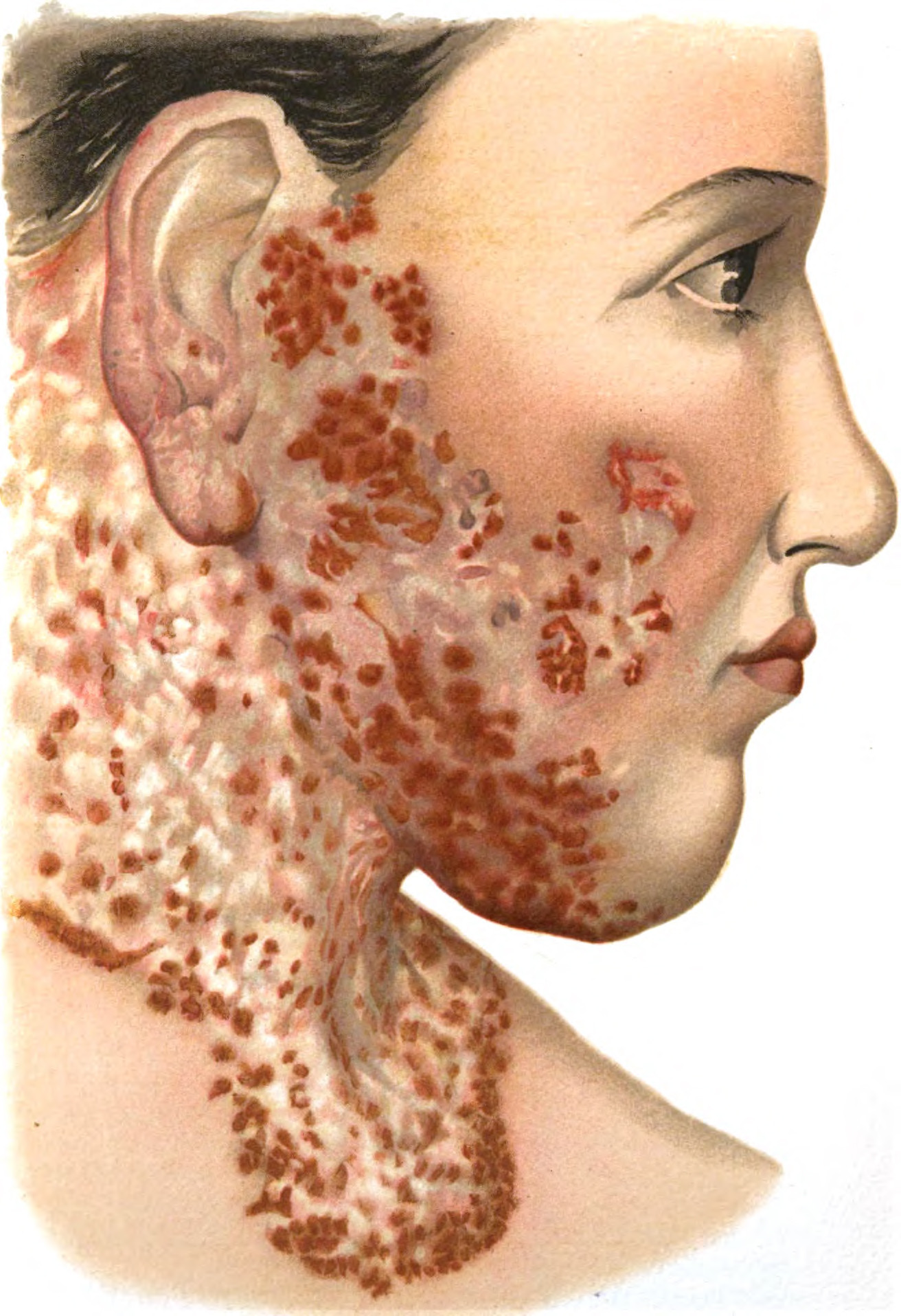
Angular stomatitis symptoms only occur at the corners of the lips. They may appear bleeding, red, swollen, crusty, blistered, scaly, itchy, and painful. These symptoms vary greatly, ranging from mere redness to blistering and bleeding.
Angular stomatitis may be accompanied by accompanying symptoms depending on the cause, such as:
- The presence of whitish crusts in the mouth area (oral thrush) due to fungal infection
- Eczema-like rash (atopic dermatitis) on the lower face
- Redness of the palate (in denture wearers)
- Saliva at the corners of the lips
- Crack-like crusts on the corners of the lips
Diagnosis
Angular stomatitis can be diagnosed based on history, complaints, and symptoms. Usually, the doctor can make this diagnosis by simply observing the corners of your lips. However, due to its various causes, the doctor may ask you about your daily habits that could be risk factors for angular stomatitis. They may also ask about your medication use, daily food consumption, and past and family history.
Angular stomatitis can be caused by a fungal or bacterial infection. To confirm the cause, the doctor may swab the corner of the affected lip for laboratory examination. The swab will then be cultured to determine the presence of fungi and bacteria and the effectiveness of the medication in treating the condition. However, this is usually only done if the previous therapy is not effective.
Assessments related to risk factors for angular stomatitis may also be done. For example, if the condition is suspected to be due to a fungal infection, the doctor will check for HIV/AIDS and blood sugar. If the condition is suspected to be due to allergic or irritant contact dermatitis, the doctor may perform a patch test to determine a further diagnosis. If there is a suspicion of malignancy, the doctor may take tissue from the wound for observation under a microscope.
Management
The management of angular stomatitis largely depends on the cause, which can be infectious and non-infectious. This condition is often caused by a fungal infection, so your doctor may give you antifungal medication as initial therapy. These antifungal medications are usually given in cream form. The other most common cause is a bacterial infection, so your doctor may also give you an antibiotic ointment. If your lips are dry, you can keep your room at home humid and drink enough mineral water daily. Not only that, you need to avoid or quit smoking and not lick your lips.
If angular stomatitis is not caused by infection, it is recommended that you protect the breaks that are usually present at the corners of the lips with petrolatum gel, emollients, or lip balm. This can protect your skin from excess moisture and heal wounds. If there are nutritional deficiencies, your doctor may prescribe vitamins such as vitamin B complex, zinc supplements, and iron supplements such as blood supplement tablets.
If the cause of angular stomatitis is related to dentures, tooth positioning problems, or braces, you can visit an oral dentist for treatment. This may include filling the areas where saliva is at risk of accumulating.
If you have other health conditions such as HIV/AIDS or diabetes mellitus, your doctor will give you appropriate therapy to control these diseases. A controlled HIV and blood sugar can significantly reduce the risk of angular stomatitis.
Complications
Angular stomatitis is typically fairly easy to treat once the cause is identified. If the condition is caused by a fungal or bacterial infection, the infection may spread to other parts of the face if not treated properly. In addition, if the condition persists for a long period of time, there may be a lack of tissue (atrophy) at the corners of the lips, permanent scars, or discoloration of the corners of the lips.
Prevention
Preventing angular stomatitis involves living a clean and healthy life and practicing regular and correct skin care. One way to do this is to keep the skin around your lips moisturized so that irritation does not occur easily.
If the skin around your lips is dry, you may want to consider applying petroleum gel or coconut oil to the corners of your lips. These gels or oils act as a protective barrier against saliva that contains bacteria and fungi. In addition, you can also use lip balm to prevent dry and chapped lips. You can also consume enough mineral water and stop smoking to prevent dry lips.
When to see a doctor?
You can try to manage angular stomatitis by preventing dryness on your lips and the skin at the corners of the lips. If this does not give good results, you can visit a doctor. If you are aware of conditions such as HIV, diabetes, Sjogren's disease, Crohn's disease, etc., you can consult with your doctor regarding the management of angular stomatitis and your comorbidities.
Looking for more information about other diseases? Click here!
- dr Hanifa Rahma
Caldwell, A., Gotter, A., & Zimlich, R. (2022). Angular Cheilitis: Symptoms, Causes, Treatments. Healthline. Retrieved 30 May 2022, from https://www.healthline.com/health/angular-cheilitis.
Ellis, R., & Frisbee, E. (2020). What Is Angular Cheilitis?. WebMD. Retrieved 30 May 2022, from https://www.webmd.com/oral-health/angular-cheilitis.
Federico, J., Basehore, B., & Zito, P. (2021). Angular Chelitis. Ncbi.nlm.nih.gov. Retrieved 30 May 2022, from https://www.ncbi.nlm.nih.gov/books/NBK536929/.