Definisi
Angina pektoris merupakan istilah medis yang menerangkan kondisi nyeri dada akibat penyakit jantung koroner. Angina pektoris sendiri terbagi atas angina pektoris stabil dan tidak stabil (unstable), tergantung kapan gejala nyeri muncul. Angka kejadian angina pektoris meningkat seiring usia, baik pada pria dan wanita.
Penyebab
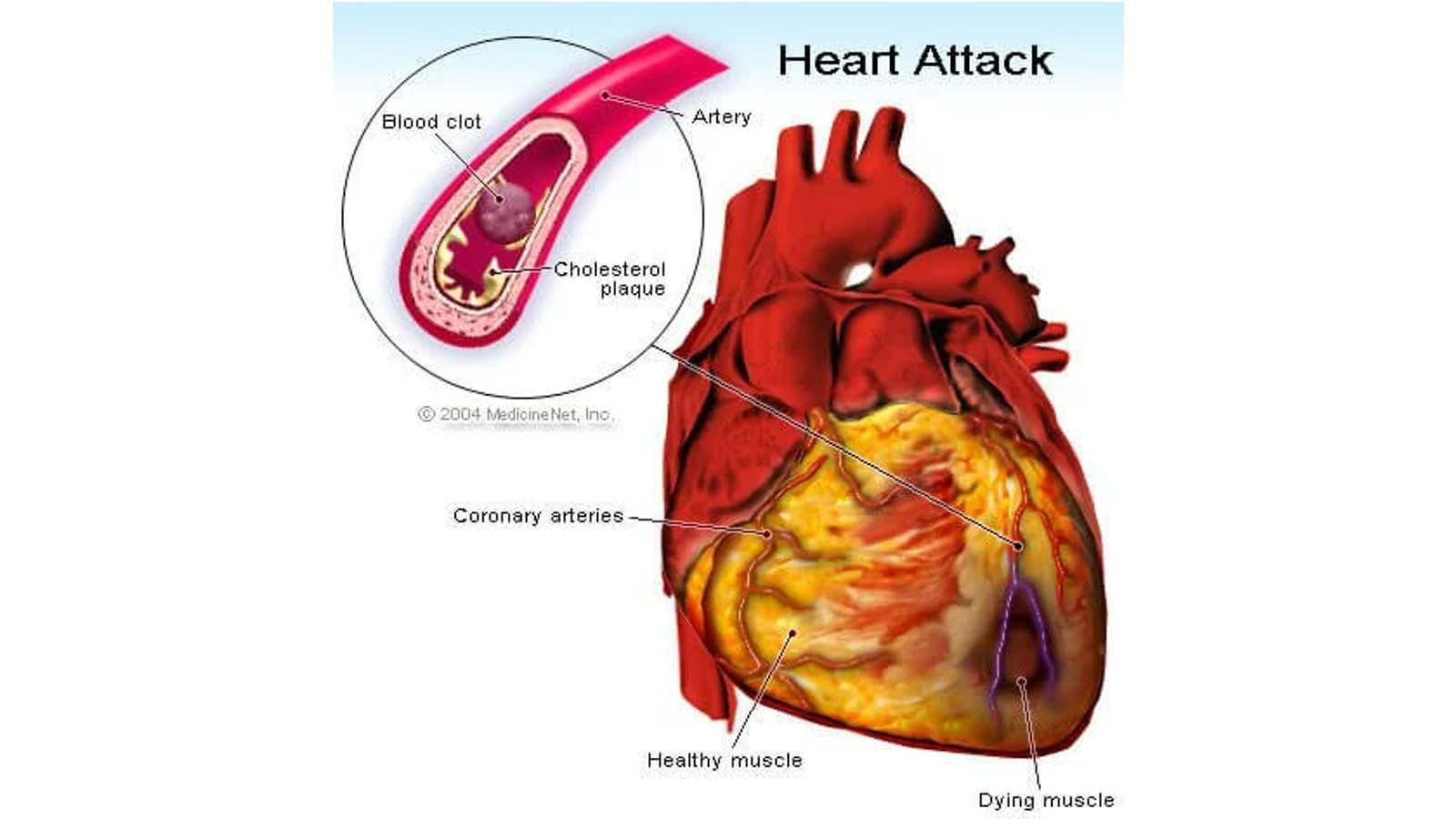
Angina pektoris disebabkan oleh penurunan aliran darah ke otot-otot jantung. Darah mengantarkan oksigen ke seluruh organ, dan otot jantung juga membutuhkan oksigen untuk bisa bekerja memompa darah dengan baik. Jika salah satu bagian tubuh atau contohnya otot-otot jantung mengalami kekurangan oksigen akibat penurunan aliran darah, terjadi sebuah kondisi yang disebut iskemia.
Penurunan aliran darah ini biasanya disebabkan oleh penyakit jantung koroner. Pada kondisi ini, ruang pembuluh nadi (arteri) di jantung menyempit akibat adanya plak endapan lemak. Plak tersebut dapat pecah atau terluka sehingga terjadi pembentukan bekuan darah. Jika hal-hal ini terjadi, area pembuluh nadi menyempit sehingga aliran darah pada pembuluh nadi dapat berkurang atau bahkan berhenti total, karena sulit lewat akibat terhalang plak. Hal inilah yang menyebabkan otot-otot jantung kekurangan oksigen.
Pada saat tubuh memiliki kebutuhan oksigen rendah (misalnya seperti saat beristirahat), otot-otot jantung masih dapat bekerja tanpa menghasilkan gejala nyeri dada meskipun aliran darahnya berkurang. Namun, jika kebutuhan oksigen meningkat (misalnya pada saat berolahraga), gejala nyeri dada dapat muncul.
Faktor Risiko
Risiko angina pektoris meningkat akibat hal-hal sebagai berikut:
1. Peningkatan Usia
Gejala nyeri dada angina paling sering terjadi pada orang berusia 60 tahun atau lebih.
2. Riwayat Keluarga dengan Penyakit Jantung
Keluarga yang dimaksud di sini adalah keluarga inti seperti ayah, ibu, atau saudara kandung.
3. Penggunaan Tembakau
Merokok, mengunyah tembakau, serta paparan terhadap asap rokok dalam jangka waktu lama (perokok pasif) dapat merusak lapisan pembuluh darah, sehingga kolesterol bisa mengendap, berkumpul, dan menyumbat aliran darah.
4. Diabetes
Diabetes meningkatkan risiko penyakit jantung koroner, yang pada akhirnya dapat menghasilkan gejala nyeri dada dan serangan jantung, dengan mempercepat pembentukan plak-plak lemak dalam pembuluh darah dan meningkatkan kadar kolesterol.
5. Tekanan Darah Tinggi
Tekanan darah yang tinggi dapat merusak pembuluh nadi dengan membuat pembuluh menjadi kaku.
6. Kadar Kolesterol atau Trigliserida Tinggi
Kadar kolesterol jahat (low-density lipoprotein, LDL) yang tinggi pada darah dapat menyebabkan penyempitan pembuluh nadi. Kadar LDL yang tinggi meningkatkan risiko angina dan serangan jantung. Kadar trigliserida yang tinggi pada darah juga dapat menyebabkan hal serupa.
7. Kondisi Kesehatan Lainnya
Kondisi kesehatan seperti gagal ginjal kronik, penyakit pembuluh nadi perifer, sindrom metabolik, dan riwayat stroke dapat meningkatkan risiko angina.
8. Kurang Berolahraga
Gaya hidup seperti ini dapat meningkatkan kadar kolesterol, tekanan darah, risiko diabetes, dan obesitas.
9. Obesitas
Kelebihan berat badan dapat memperberat kerja jantung dalam memompa darah.
10. Stres Emosional
Stres dan kemarahan yang terlalu sering dapat meningkatkan tekanan darah. Tidak hanya itu, peningkatan hormon yang terjadi saat stres dapat mempersempit pembuluh nadi.
11. Obat
Obat yang mengecilkan pembuluh darah, seperti obat-obatan migrain, dapat menyebabkan tipe angina tertentu.
12. Penyalahgunaan Zat
Kokain dan obat-obatan stimulan lainnya dapat membuat pembuluh darah kaku dan memicu nyeri dada angina.
13. Suhu Dingin
Suhu dingin dapat memicu salah satu tipe angina, yaitu angina Prinzmetal (kondisi nyeri dada kiri yang muncul saat beristirahat karena pembuluh nadi koroner jantung mengalami spasme).
Gejala
Angina pektoris ditandai dengan nyeri dada di area kiri, namun nyeri dada ini memiliki kekhususan tertentu. Bila gejala angina pektoris termasuk stabil, bisa dilihat tanda-tanda khas nyeri seperti:
- Nyeri muncul saat kerja jantung meningkat, misalnya saat beraktivitas fisik
- Tidak terjadi tiba-tiba, dan ada episode nyeri dada lainnya yang serupa
- Terjadi dalam waktu yang singkat (di bawah 5 menit)
- Dapat membaik dengan istirahat atau konsumsi obat tertentu
- Nyeri bisa terasa seperti pengumpulan gas atau kembung
- Dapat terasa seperti menjalar ke leher, lengan, rahang, dan punggung
Namun, apabila gejala nyeri dada terasa semakin parah, misalnya tidak membaik dengan istirahat atau konsumsi obat, kemungkinan angina pektoris yang terjadi adalah angina pektoris tidak stabil. Tidak hanya itu, gejala yang semakin parah dapat menjadi penanda adanya serangan jantung. Segala perburukan gejala angina sebaiknya segera dikonsultasikan kepada tenaga kesehatan terdekat. Gejala lainnya yang dapat menyertai angina adalah pusing, lelah, sesak napas, mual, dan berkeringat banyak.
Diagnosis
Diagnosis angina pektoris dapat dilakukan dengan pertanyaan mengenai riwayat pasien dan pemeriksaan. Riwayat dapat mencakup riwayat episode sebelumnya, peningkatan keparahan episode, serta faktor risiko angina pada seseorang.
Pemeriksaan yang dapat dilakukan berupa:
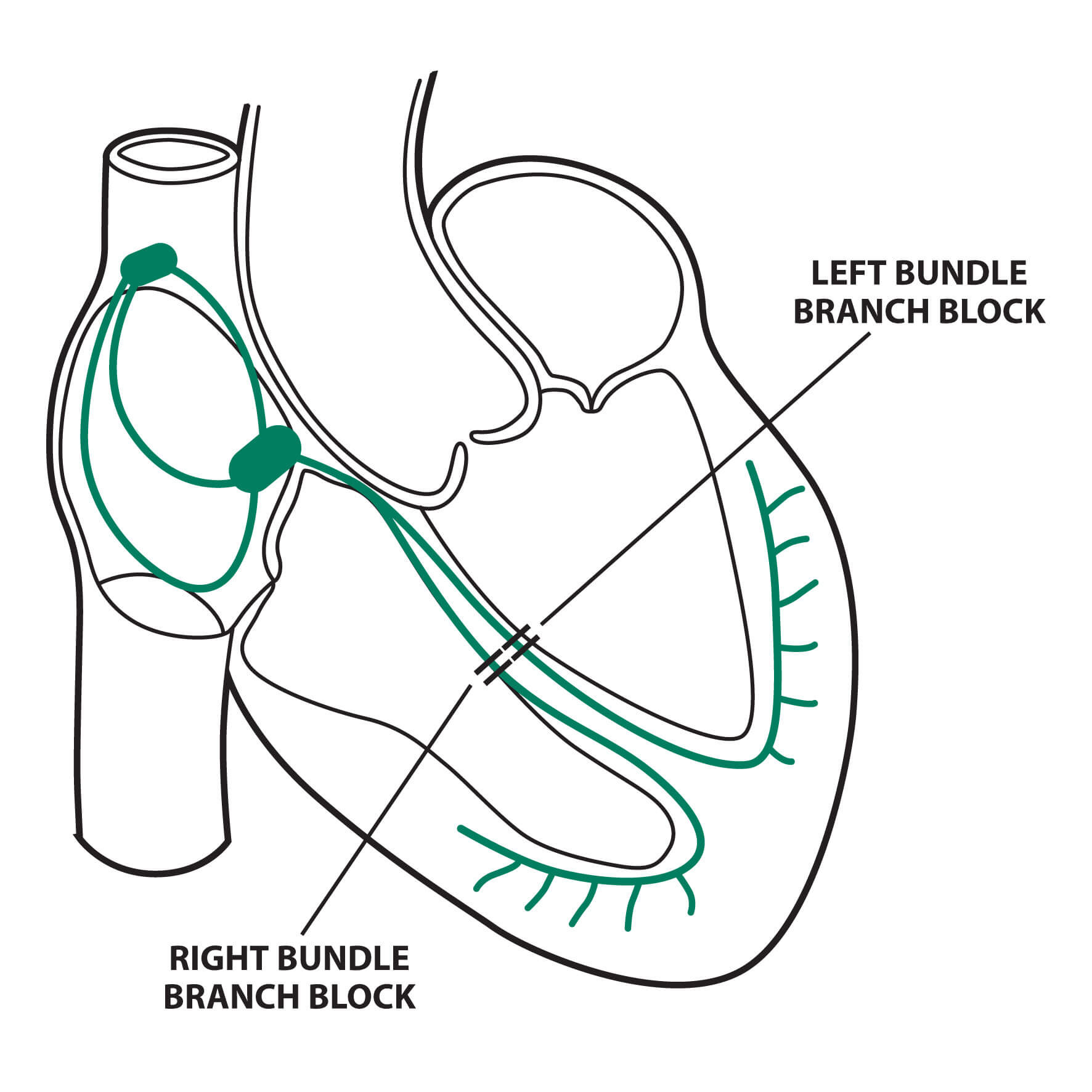
1. EKG (Elektrokardiografi)
Pemeriksaan EKG merupakan sebuah pemeriksaan yang berfungsi untuk melihat aliran listrik pada jantung. Anda akan dipasangi beberapa patch yang dapat mendeteksi aliran listrik pada jantung Anda.
2. Rontgen Dada
Pemeriksaan rontgen dada dilakukan dengan menggunakan sinar X yang kemudian ditangkap oleh film untuk melihat isi rongga dada Anda (seperti bentuk jantung dan paru).
3. Pemeriksaan Darah Lengkap
Pemeriksaan darah lengkap mencakup pemeriksaan kadar hemoglobin (zat pada darah yang mengikat oksigen), sel darah merah, sel darah putih, dan trombosit.
4. Profil Metabolik Dasar
Pemeriksaan profil metabolik dasar mencakup pemeriksaan gula darah, fungsi ginjal, dan beberapa elektrolit di dalam tubuh (yang berperan dalam menjaga keseimbangan cairan).
5. Pemeriksaan Stress Test
Tes ini merupakan tes untuk membandingkan kerja jantung Anda sebelum dan sesudah beraktivitas fisik atau penggunaan obat tertentu. Pemeriksaan dilakukan saat Anda berjalan pada treadmill atau sepeda stasioner.
6. Pemeriksaan Enzim Jantung
Jika pemeriksaan ini tersedia dan ada kecurigaan serangan jantung, bisa diperiksa enzim jantung. Troponin merupakan salah satu jenis protein yang bisa ditemukan pada otot-otot jantung. Ketika sel otot jantung mengalami kerusakan, kadar troponin akan meningkat dalam darah.
7. Kateterisasi Jantung
Kateterisasi jantung merupakan pemeriksaan dengan menggunakan selang yang dimasukkan ke jantung, kemudian digunakan untuk melihat aliran darah di dalam pembuluh nadi.
Tata Laksana
Angina pektoris stabil biasanya dapat membaik dengan istirahat atau pemberian obat tertentu. Biasanya, obat yang dapat digunakan untuk menurunkan gejala angina akan diresepkan kepada Anda jika Anda berkonsultasi. Obat ini adalah golongan nitrat, yang berfungsi untuk melemaskan otot-otot pada pembuluh darah, sehingga pembuluh darah menjadi lebih elastis dan jantung pun dapat memompa darah dengan lebih mudah. Darah yang dipompa jantung juga akan masuk ke dalam otot-otot jantung itu sendiri.
Jika Anda mengalami perburukan gejala, misalnya nyeri dada kiri yang dirasakan tidak membaik dengan istirahat atau obat, Anda dapat berkonsultasi kepada dokter. Dokter dapat merujuk Anda untuk melakukan pemeriksaan yang dapat menentukan kondisi Anda dan tata laksana selanjutnya.
Selain itu, Anda dapat melakukan perubahan gaya hidup. Perubahan gaya hidup yang disarankan adalah menjaga berat badan ideal, olahraga teratur, dan berhenti merokok. Anda dapat berkonsultasi kepada dokter mengenai target dan cara penurunan berat badan yang terbaik untuk Anda. Olahraga yang disarankan adalah olahraga berintensitas sedang seperti aerobik, jogging, bersepeda, atau berenang, yang dilakukan sekitar 30 menit per hari, 3-5 kali per minggu.
Jika Anda mengalami kondisi kesehatan lainnya seperti diabetes, kadar kolesterol tinggi, atau penyakit gagal ginjal kronik, Anda dapat berkonsultasi kepada dokter terkait cara mengontrol kondisi tersebut. Jika kondisi-kondisi tersebut dapat dikontrol, risiko Anda mengalami gejala nyeri dada angina akan menurun.
Komplikasi
Nyeri dada yang terjadi akibat angina dapat membuat aktivitas menjadi tidak nyaman. Namun, komplikasi terbesar dadri angina pektoris adalah serangan jantung. Jika Anda mengalami gejala-gejala nyeri dada yang merupakan tanda waspada untuk serangan jantung, segera pergi ke IGD terdekat.
Tanda dan Gejala Waspada Serangan Jantung
- Nyeri dada yang terasa seperti tertindih beban berat atau tertekan pada bagian tengah atau kiri dada yang terjadi selama lebih dari 5 menit
- Pusat nyeri tidak dapat ditunjuk secara pasti, namun nyeri dapat menjalar ke arah pundak, lengan, punggung, dan rahang
- Pingsan
- Tingkat nyeri bisa dideskripsikan sangat hebat
- Peningkatan episode nyeri
- Mual dan muntah
- Nyeri menjalar ke lambung
- Napas pendek
- Banyak berkeringat
Pencegahan
Anda dapat mencegah terjadinya gejala nyeri dada angina dengan memperbaiki pola gaya hidup. Perubahan gaya hidup tersebut meliputi:
- Tidak merokok
- Konsumsi makanan bergizi, mengutamakan konsumsi sayuran dan buah-buahan
- Menghindari atau membatasi alkohol
- Berolahraga teratur
- Menjaga berat badan ideal
- Mengontrol kondisi kesehatan lain yang dapat meningkatkan risiko terjadinya angina pektoris
- Menurunkan stres emosional
Kapan Harus ke Dokter?
Jika Anda baru pertama kali mengalami kondisi mirip angina, Anda dapat berkonsultasi kepada dokter. Dokter mungkin akan melakukan beberapa tes untuk menguji kesehatan jantung Anda. Tidak hanya itu, dokter akan meresepkan obat-obatan serta memberikan saran untuk mengontrol kondisi tersebut.
Jika Anda mengalami perburukan gejala, misalnya nyeri dada yang semakin lama, atau tidak membaik dengan pemberian obat atau beristirahat, sebaiknya Anda segera ke IGD terdekat. Anda sangat tidak disarankan untuk menyetir atau pergi sendirian ke IGD. Jika Anda mengalami perburukan gejala, segera minta pertolongan orang terdekat untuk mengantar Anda ke IGD.
Mau tahu informasi seputar penyakit lainnya? Cek di sini, ya!
- dr Hanifa Rahma
Angina - Symptoms and causes. (2022). Retrieved 10 April 2022, from https://www.mayoclinic.org/diseases-conditions/angina/symptoms-causes/syc-20369373
Angina Pectoris. Retrieved 10 April 2022, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/angina-pectoris
Hermiz, C., & Sedhai, Y. (2021). Angina. Retrieved 10 April 2022, from https://www.ncbi.nlm.nih.gov/books/NBK557672/