Definition
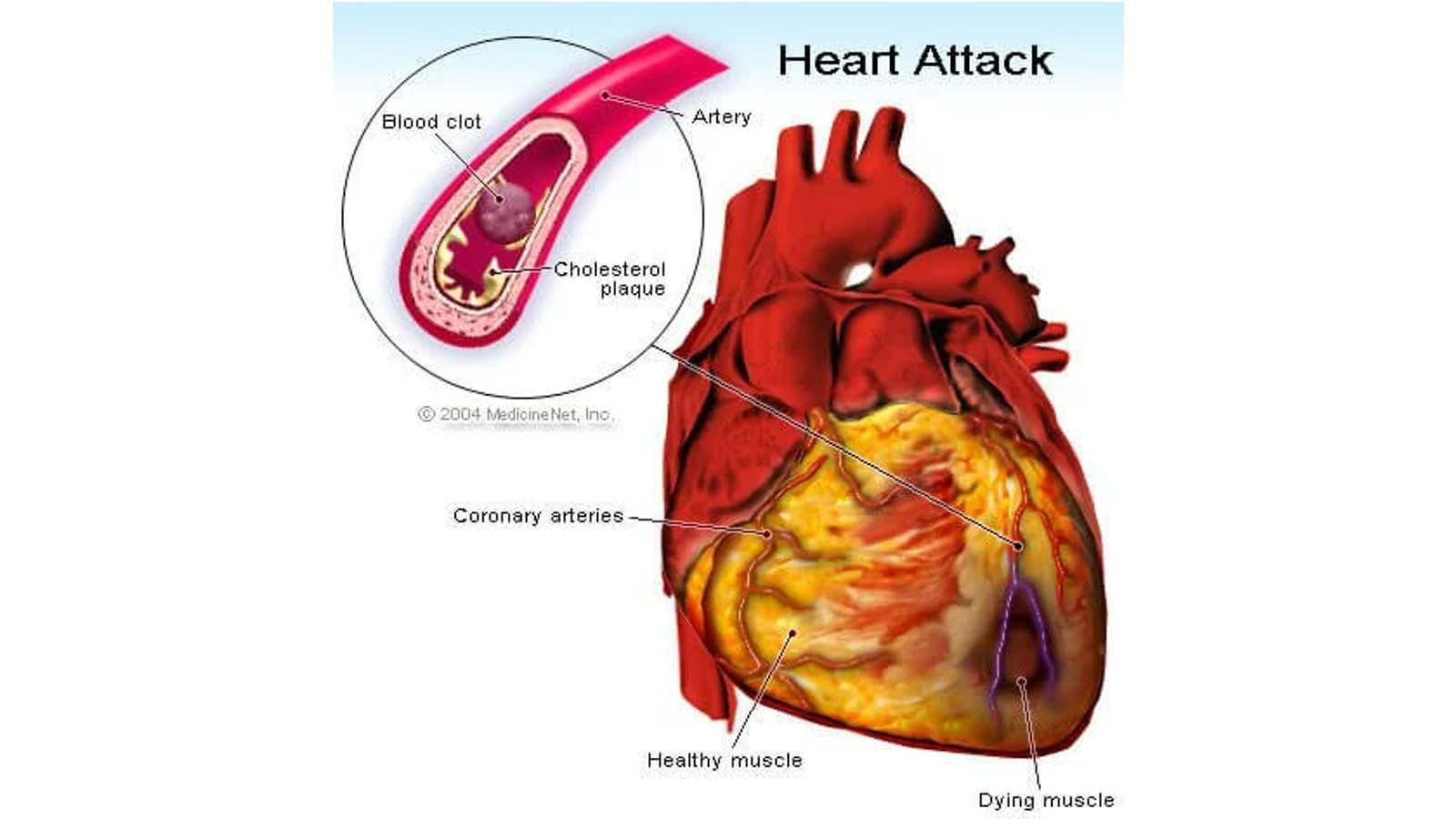
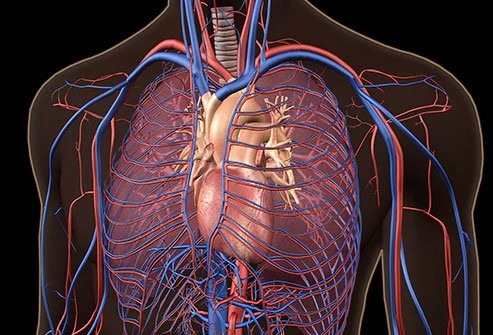
Myocardial infarction, also known as a heart attack, occurs when blood flow to the heart is blocked. The blockage is usually caused by fat, cholesterol, and other substances, which form plaque in the arteries that supply blood to the heart muscles. The arteries that specifically feed the heart muscles are called coronary arteries.
Causes
Myocardial infarction happens when one or more coronary blood vessels become clogged. Over time, fatty deposits, including cholesterol, form plaques that can clog arteries. This sequence is referred to as atherosclerosis.
When a heart attack occurs, the plaque may rupture, releasing cholesterol and other substances into the bloodstream. Meanwhile, a blood clot may form at the site of plaque rupture. If the clot is large, it can obstruct blood flow in the coronary arteries, depriving the heart muscle of oxygen and nutrients. This is a condition of cardiac ischemia. This blockage can be complete or partial.
Another cause of heart attack is coronary artery stiffness, which prevents blood flow to the heart muscles. Tobacco smoking and the use of illicit substances such as cocaine can both cause vascular stiffness. This condition can be life-threatening.
In addition to the causes above, COVID-19 can damage the heart so that heart attacks are more likely to occur.
Risk factor
These risk factors include:
- Age. Men over 45 years old and women over 55 years old
- Tobacco. Tobacco use can be in the form of long-term active or passive smoking
- High blood pressure. High blood pressure can damage the blood vessels that supply the heart's muscles over time. This can be exacerbated by other conditions such as obesity, high cholesterol levels, and diabetes
- High cholesterol and triglyceride levels. High levels of bad cholesterol (LDL) can clog blood vessels. Apart from bad cholesterol, triglyceride fats can cause blockages as well. However, good cholesterol (HDL) can lower this risk
- Obesity. Obesity is associated with elevated levels of cholesterol and triglycerides, high blood pressure, and diabetes. Every 10% weight loss can lower the risk of myocardial infarction
- Diabetes. Diabetes occurs due to insufficient levels of the hormone insulin or the body having difficulty responding to insulin, causing blood sugar levels to rise
- Metabolic syndrome. This is a combination of obesity, high blood pressure, and high blood sugar that increases the risk of myocardial infarction by twofold
- Family history of heart attack. Siblings, parents, or grandparents who had a heart attack at an early age (before age 55 in men and before age 65 in women)
- Lack of physical activity. Lack of physical activity leads to increased cholesterol levels, higher blood pressure, and obesity. People who exercise regularly have better heart health, including lower blood pressure
- Stress. Emotional stress increases hormone levels that increase the risk of heart attack
- Substance abuse. The use of stimulant drugs such as cocaine or amphetamines can cause stiffness of the coronary blood vessels, which can lead to a heart attack
- History of preeclampsia. If you have experienced a sudden rise in blood pressure during pregnancy, you are at higher risk of having a heart attack
- Autoimmune conditions, such as rheumatoid arthritis or lupus
Symptoms
Signs and symptoms of a heart attack generally include:
- A feeling of pressure, squeezing, or pain in the chest that may radiate to the arms, neck, jaw, and back
- Nausea, bloating, burning in the chest, or abdominal pain
- Shortness of breath
- Cold sweat
- Feeling tired
- A sense of floating or dizziness
However, not everyone experiences the same symptoms. Symptoms can range from mild to severe. Symptoms may not appear at all, or the first symptom may be cardiac arrest.
Some heart attacks occur unexpectedly, while others may exhibit warning signs and symptoms hours, days, or weeks in advance. Early warning signs may include chest pain triggered by activity and improvement with rest (angina pectoris).
Diagnosis
Myocardial infarction is a medical emergency. When there is a suspicion of myocardial infarction, a comprehensive examination will be conducted to diagnose this condition definitively. Signs, symptoms, ECG findings, and cardiac biomarkers can recognize myocardial infarction.
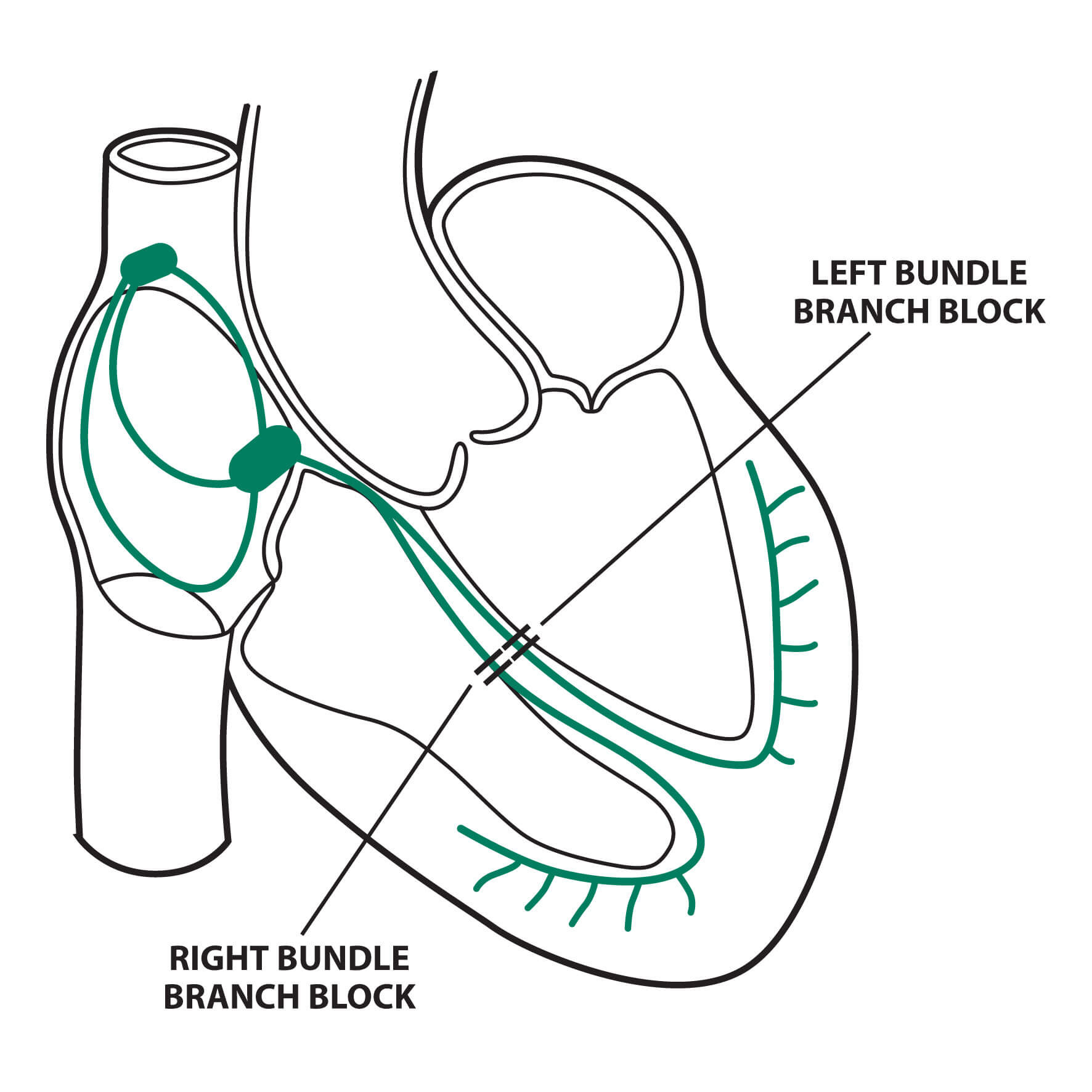
Electrocardiography (ECG) is an examination to detect the electrical flow of the heart. It is performed by attaching a patch to the chest and a particular device to detect the flow of electricity. The findings of the ECG can determine where the heart muscle is having problems. Meanwhile, biomarkers are substances that change in levels during muscle damage. Biomarkers that can be used to detect myocardial infarction are troponin and creatine kinase MB (CK MB).
In addition to these two tests, the doctor may perform imaging tests. Imaging can be ultrasonography (sound waves), radioactive substances, or magnetic resonance imaging (MRI) using magnetic waves.
Management
Myocardial infarction is an emergency. Doctors may insert oxygen tubes, IVs, and monitors to track the patient's condition. Initial treatment may include nitrates and aspirin. Nitrates are usually administered under the tongue as a treatment for a heart attack. This drug helps to reduce the workload on the heart. Meanwhile, aspirin is chewed to help prevent blood clots caused by plaque rupture.
After arriving at the hospital, several action options can be taken. These include primary percutaneous coronary intervention (primary PCI), which aims to open a blocked blood vessel using a stent or ring. Another option is fibrinolytic drugs, which are administered to destroy fibrin, a component of blood clots.
Another treatment option is to administer blood-thinning medications. Usually, aspirin and clopidogrel are used. These drugs prevent blood clots caused by plaque rupture. If the blood pressure is high, the doctor may prescribe medications to lower it.
Treatment for myocardial infarction is long-term and aims to reduce risk factors and prevent recurrent infarction. This may include cholesterol—and fat-lowering medication, diabetes treatment, and lifestyle changes. Lifestyle changes include smoking cessation, diet control, alcohol consumption, and maintaining an ideal body weight.
Complications
Myocardial infarction complications are very diverse and are divided into five groups, which are:
- Ischemia or lack of oxygen to the heart muscles. This complication includes recurring heart attacks, heart muscle death, and chest pain (angina pectoris)
- Arrhythmia or heart rhythm abnormalities. Heart rhythm abnormalities can cause the heart to beat faster or slower and, if left untreated, can result in death
- Mechanical or heart pump-related. Complications include heart muscle dysfunction, heart failure, shock (multiple organ failure), and heart wall damage
- Embolism or the presence of blood clots that block blood vessels
- Inflammation of the heart membrane (pericarditis) and the appearance of excess fluid in the heart membrane (pericardial effusion)
Prevention
Anyone, including those who have had a previous myocardial infarction, can take steps to prevent another. Prevention can include:
- Medications. Certain medications can reduce the risk of a heart attack while also allowing the damaged heart to function properly. These medications are usually prescribed by a doctor and help to control risk factors for heart attacks.
- Lifestyle changes. Keeping a healthy weight, eating a nutritious diet, quitting smoking, exercising regularly, managing stress effectively, and controlling conditions that can lead to heart attacks, such as high blood pressure, high cholesterol, and diabetes.
When to see a doctor?
Suppose you or someone you know is experiencing typical symptoms of a myocardial infarction. In that case, you'll need to act quickly by calling for emergency assistance or taking the patient to the nearest hospital's emergency room. If you have nitrates, take them under the tongue immediately.
If someone suddenly faints, immediately check their heart rate and breathing. If a heartbeat and breathing are not found, ask others to call for medical assistance, and you can begin cardiopulmonary resuscitation (CPR). As a layperson, you can perform rapid and deep chest compressions at a rate of about 100-120 per minute. If you have basic life support training, you can secure the airway and provide breath support to save the person.
Looking for more information about other diseases? Click here!
- dr Anita Larasati Priyono
Heart attack - Symptoms and causes. (2022). Retrieved 11 April 2022, from https://www.mayoclinic.org/diseases-conditions/heart-attack/symptoms-causes/syc-20373106
Ojha, N., & Dhamoon, A. (2021). Myocardial Infarction. Retrieved 11 April 2022, from https://www.ncbi.nlm.nih.gov/books/NBK537076/
Zafari, A. (2019). Myocardial Infarction: Practice Essentials, Background, Definitions. Retrieved 11 April 2022, from https://emedicine.medscape.com/article/155919-overview